In particular, IBS patients with predominant diarrhea suffer from a high burden of disease. This is shown, among other things, by a large international survey study conducted by a Swedish research team. Therapy of irritable bowel syndrome is multimodal and symptom-oriented. An overarching goal is to improve the quality of life of those affected. In the new edition of the irritable bowel guideline published last year, the use of phytotherapeutics is also recommended, among other things.
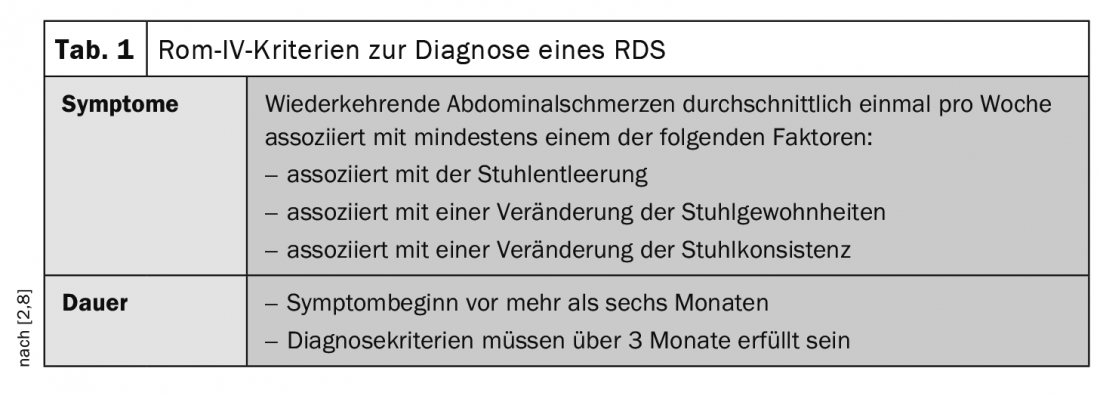
The term irritable bowel syndrome (IBS) is used to describe non-specific functional digestive disorders. Typical symptoms include abdominal pain, cramps, flatulence, and changes in bowel movements such as diarrhea and/or constipation [1]. The diagnosis of IBS is based on the Rome IV criteria (Table 1) and on a focused gastroenterological history including psychosocial aspects [2,9]. The etiology is multifactorial, and various factors are suspected or discussed without necessarily being proven in individual cases [2]. Because the different pathophysiologies are often not apparent in the clinic, a multimodal treatment strategy is used [3]. In addition to dietary measures and psychosocial interventions, symptom-oriented drug therapy options are also used. It can be a lengthy process before the individually appropriate treatment strategy is found for a patient. Phytotherapeutics that have scientifically proven specific effects are also frequently used. The fact that IBS can be very stressful for sufferers is shown, among other things, by a survey study involving the University of Gothenburg and various research institutions in the United Kingdom [4].
Online survey: Assessments of IBS patients and physicians
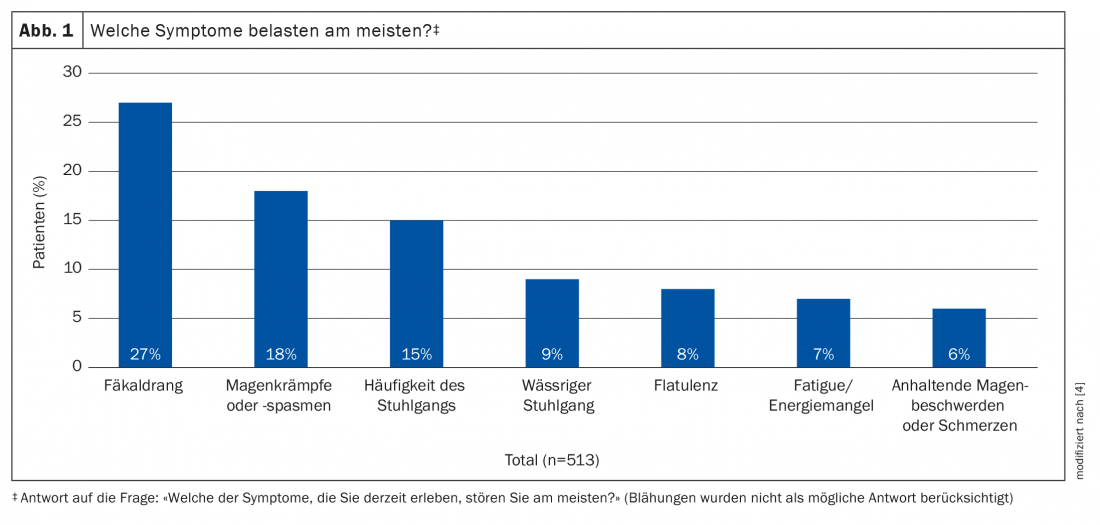
Of 8627 screened patients, researchers interviewed a total of 513 irritable bowel patients who met inclusion criteria during 2016 [4]. One of the inclusion criteria was that diarrhea was a major symptom. Of the respondents, 70% were female and the average age was 40.9 years. Study participants were from Australia (n=76), Canada (n=66), France (n=43), Germany (n=80), Italy (n=85), Spain (n=81), and the United Kingdom (n=82). All participants completed a 30-minute web-based structured questionnaire. The survey included several questions about patients’ subjectively perceived “burden of disease” and previous treatments and experiences, as well as their expectations of therapy.
In addition to the patient survey, a survey of HCPs was conducted. 366 primary care physicians and 313 gastroenterologists participated.
Severity of symptoms correlates with quality of life
The most debilitating symptom reported by the IBS patients surveyed was fecal urination (27%) [4] (Fig. 1) . Fatigue occurred on the most days per month (18 days on average). The most commonly reported comorbidities were anxiety (37%), depression (27%), and migraine (26%). The most common reason for making an initial appointment with a physician was that IBS severely impacted quality of life (49%). Other reasons included increasing frequency of symptoms (48%), concern about duration of symptoms (44%), and increasing severity (42%). The S3 guideline Irritable Bowel Syndrome, updated in 2021, identifies an evidence-based association between IBS severity and quality of life impairment [5,8]. Accordingly, perceived impairment in quality of life apparently influences not only the management of gastrointestinal symptoms, because extraintestinal symptoms are also reported more frequently [6,7].
More than half of patients take multiple medications
A total of 97% of patients surveyed reported taking at least one type of medication intermittently or daily [4]. 61% of patients reported using ≥3 treatment types daily or intermittently. 19% reported taking antidepressants daily, and 73% were using over-the-counter medications at the time of the survey, either alone (42%) or with prescription medications (31%). Antidiarrheal agents were most commonly used intermittently in 64% and daily in 12% of patients. The most commonly taken daily medications were antidepressants (19%), followed by probiotics (18%). 33% of respondents reported taking codeine-based pain medications occasionally or daily. Patients who had seen a gastroenterologist had a higher proportion of those taking antispasmodics (14% vs. 15.8%), bile acid sequestrants (5% vs. 1%), anti-nausea agents (6% vs. 1%), and antibiotics (4% vs. 1%) daily than the rest of the patients (all comparisons: p<0.05). A total of 366 primary care physicians and 313 gastroenterologists participated in the physician survey: a total of 70% and 65%, respectively, agreed it was important for patients with IBS to feel supported and 73% said their main goal was to improve quality of life.
Phytotherapy recommended as part of a multimodal therapy
According to the current S3 guideline, a multimodal, integrative treatment approach is most promising [1]. Among other things, the use of herbal preparations or phytotherapeutics is also recommended. In addition to the use of soluble fiber for obstipative and diarrheal symptoms, the guideline also recommends the use of STW5* for irritable bowel syndrome, with particular emphasis on the relief of abdominal pain. Clinical evidence for relief of irritable bowel symptoms is also available for the combination of peppermint and caraway oil.
* STW5 is a herbal combination preparation with alcoholic extracts of the fresh plant Iberis amara and angelica root, chamomile flowers, caraway fruit, milk thistle, lemon balm leaves, peppermint leaves, celandine and sweetroot.
Literature:
- Layer P, et al: Update S3-Leitlinie Irritable Bowel Syndrome: Definition, Pathophysiology, Diagnosis and Therapy. Joint guideline of the DGVS and the DGNM, AWMF registration number 021/016. Z Gastroenterol 2021; 59(12): 1323-1415.
- Dolder M, Wilhelmi M, Huber F: Irritable bowel syndrome (Colon irritabile), www.medix.ch/wissen/guidelines/magen-darm-krankheiten/reizdarmsyndrom-colon-irritabile, (last accessed 02.09.2022).
- Frieling T: Functional disorders of the digestive tract and functional gastrointestinal diseases, www.arzneimitteltherapie.de/heftarchiv/2017/09/funktionsstorungen-im-verdauungstrakt-und-funktionelle-magen-darm-erkrankungen.html, (last accessed 02.09.2022).
- Törnblom H, et al: Understanding symptom burden and attitudes to irritable bowel syndrome with diarrhoea: results from patient and healthcare professional surveys. United European Gastroenterol J 2018; 6(9): 1417-1427.
- Drossman DA, et al: Severity in irritable bowel syn drome: a Rome Foundation Working Team report. Am J Gastroenterol 2011; 106: 1749-1759.
- Levy RL, et al: Intergenerational trans mission of gastrointestinal illness behavior. Am J Gastroenterol 2000; 95: 451-456.
- Whitehead WE, et al: Learned illness behav ior in patients with irritable bowel syndrome and peptic ulcer. Dig Dis Sci 1982; 27: 202-208.
- Drossman D: Functional gastrointestinal disorders: history, pathophysiology, clinical features, and rome IV. Gastroenterology 2016; 150: 1262-1279.
- Lacy BE, Patel NK: Rome Criteria and a Diagnostic Approach to Irritable Bowel Syndrome. J Clin Med 2017; 6(11).
GP PRACTICE 2022: 17(9): 31-32











