In addition to local treatment of chronic wounds with the use of phase-appropriate modern wound dressings, causal therapy of the underlying cause is crucial for therapeutic success. The use of systemic therapeutics depends on the underlying disease. Especially for dermatological wounds, the range of possible system therapies has increasingly expanded in recent years.
In addition to local treatment of chronic wounds with the use of phase-appropriate modern wound dressings, causal therapy of the underlying cause is crucial for therapeutic success. The use of systemic therapeutics depends on the underlying disease. Especially for dermatological wounds, the range of possible system therapies has increasingly expanded in recent years. However, due to the rarity of many dermatologic conditions presenting with chronic ulcers as a symptom, most of the systemic medications are off-label uses, except for individual approvals, and their use can lead to problems with reimbursement, for example. This manuscript is intended to provide an overview of current systems therapies for selected dermatologic wounds.
The most common causes of non-healing wounds are vascular diseases such as chronic venous insufficiency or peripheral arterial occlusive disease, diabetic foot syndrome or pressure ulcers. By definition, chronic wounds are wounds that have persisted for at least eight weeks despite treatment or in which the above-mentioned underlying diseases are present as the cause of the wound [1]. Identifying the cause of the wound is essential for choosing the right and thus promising causal therapy. Therefore, a detailed history, diagnostic workup, and interdisciplinary medical treatment are required for structured patient care.
Adequate pain therapy, the administration of antibiotics in the presence of a wound infection, or the treatment of nutritional deficiencies by taking dietary supplements can support wound healing. However, since this type of drug therapy applies to all wound types, it will only be briefly mentioned here.
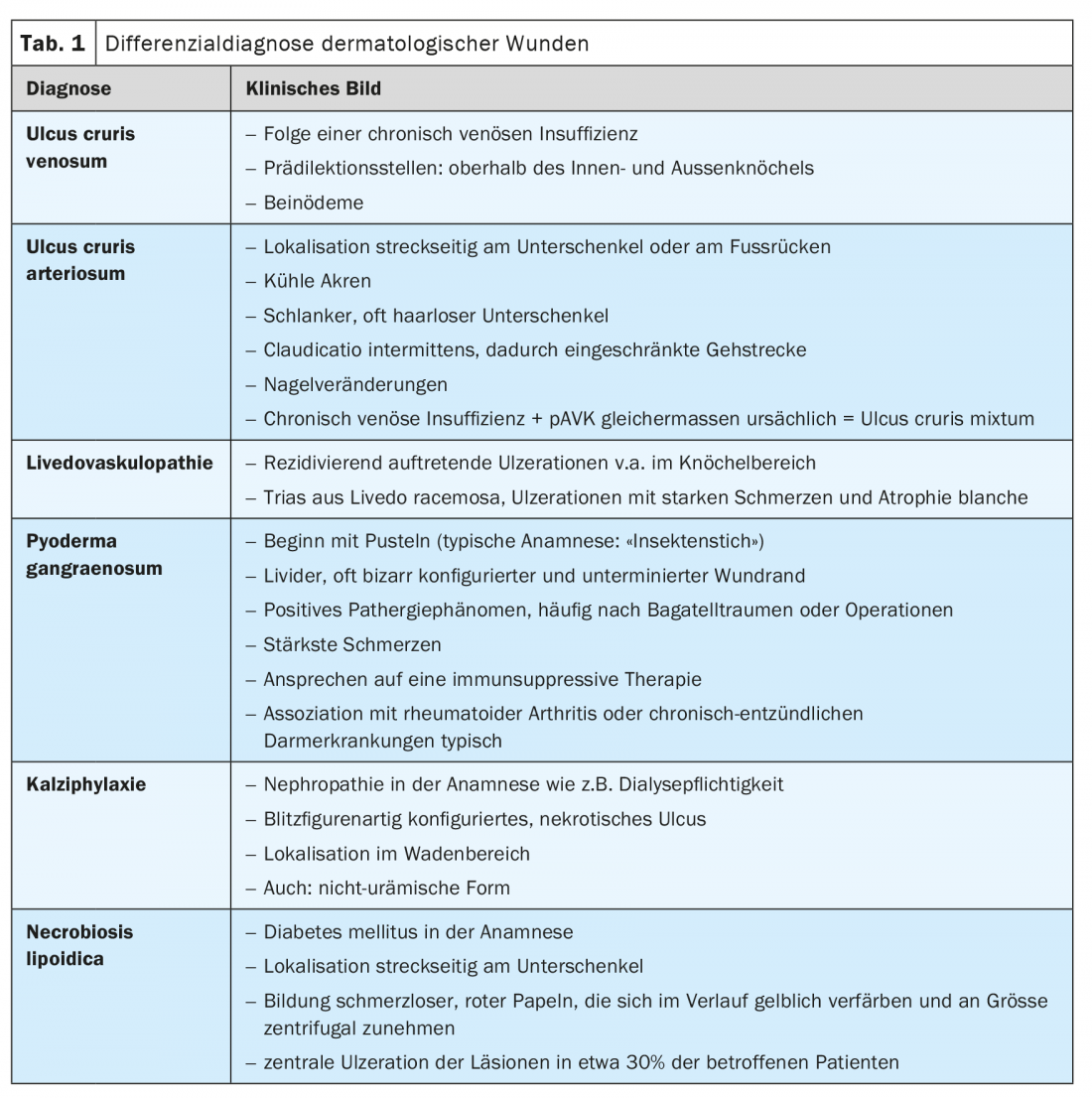
The causal therapeutic options for selected clinical pictures are presented below. Table 1 shows an overview of the most important dermatological differential diagnoses of chronic wounds.
Vascular ulcers
Starting from chronic venous insufficiency, venous leg ulcer (UCV) may develop, showing an age-dependent prevalence with a peak in 70-79-year-olds [2]. Predilection sites of UCV are located above the medial and lateral malleolus (Fig. 1). Therapy is primarily aimed at improving the underlying disease, but in some cases does not lead to success despite optimal wound care due to already very pronounced dermatolipofasciosclerosis and is subject to a high recurrence rate. An extension of therapy on a systemic level may improve wound healing; in particular, drugs with anti-inflammatory and circulation-enhancing effects such as acetylsalicylic acid, statins, low-molecular-weight heparin, or pentoxifylline show positive results in individual cases, but high evidence is not available [1]. Compression therapy remains the first-line treatment for UCV.

The differential diagnosis and pathophysiological distinction must be made between leg ulcers and arteriosclerosis. The cause here is peripheral arterial occlusive disease (PAVD). The ulcers are typically located pretibially or in the toe area. In addition to improving the blood flow situation through interventional/vascular surgical procedures, platelet aggregation inhibitors, prostaglandins, or prostacyclins may be used. Secondary prevention of atherosclerosis is important in order to prolong life expectancy and reduce the risk of amputation. Possible preventive measures include lifestyle changes, optimal adjustment of blood glucose levels and blood pressure, and reduction of the cardiovascular risk profile, e.g., through nicotine abstinence or the use of statins [1].
In the case of permanent elevated blood pressure values, calcifications of the lower leg vessels can lead to a hypertonic leg ulcer typically located on the dorsal lower leg (= “Ulcus cruris Martorell”). In addition to the diagnostic difficulty, there are no clear recommendations for targeted treatment other than optimization of blood pressure control.
|
Excursus Janus kinase inhibitors Janus kinases (JAKs) belong to the group of cytoplasmic tyrosine kinases. They are activated by stimulation of receptors by specific growth factors, growth hormones, chemokines and cytokines. After activation, they phosphorylate STAT transcription factors and thus transport STAT factors into the nucleus. This affects the expression of specific genes, such as proinflammatory cytokines and enzymes. There are four known types of JAK kinases: JAK1, JAK2, JAK3 and TYK2, which are mainly found in hematopoietic cells [9]. The recognition that Janus kinases contribute significantly to the immunological processes of inflammatory diseases has led to the development of Janus kinase inhibitors, which are now established in oncology but are also increasingly used in rheumatology and dermatology [9]. They are approved for rheumatoid arthritis, psoriatic arthritis and severe atopic dermatitis. There are currently five approved preparations with varying specificity that are taken orally or applied topically as a cream. |
Pyoderma gangraenosum
Pyoderma gangraenosum (PG) is an immunologically induced wound, although its exact pathogenesis has not yet been elucidated [3]. With the help of the Paracelsus Score, the PG can be better diagnosed: Rapid dynamics of the disease course, livid and often bizarrely configured ulcerations with undermined margins (Fig. 2) , and severe pain are indicative of the disease. A positive pathergy phenomenon (triggering of pathologic skin lesions by trivial trauma), histologic signs of suppurative inflammation, and response to immunosuppressive therapy also support the diagnosis [4].

Pyoderma gangraenosum occurs preferentially (up to 70%) on the legs, particularly the tibial region, but may also occur on other areas of the body. There is also often an association with other (autoinflammatory) diseases such as rheumatoid arthritis, inflammatory bowel disease, as well as malignancies or metabolic syndrome. Often the PG cannot be adequately controlled by topical therapy, necessitating the use of systemic therapeutics.
In most patients, immunosuppressive systemic therapy is indicated [3]. Currently, only glucocorticoids (prednisone, prednisolone) are approved; all other immunosuppressants are used off label. These include, for example, ciclosporin A and infliximab. In addition, therapy with dapsone, azathioprine, mycophenolate mofetil, and intravenous immunoglobulins may be considered. The use of monoclonal antibodies against proinflammatory cytokines such as IL-1 (anakinra, canakinumab), IL-12 and IL-23 (ustekinumab), IL-17 (secukinumab), and TNF-alpha (adalimumab, etanercept) is promising [1,3].
Positive effects in smaller case numbers of pa-tients were observed for several biologics, i.v. immunoglobulins (IVIG), and IL-1 receptor antagonists. However, due to the rarity of the disease, large randomized trials of newer therapeutic approaches are lacking. The use of newer system therapeutics in label is occasionally possible via the indication in the presence of an underlying rheumatologic disease [5]. In such cases, an interdisciplinary case discussion and treatment decision is recommended.
With the S1 guideline published in 2020, structured therapy recommendations are available for the first time [6]. In this regard, the systemic therapy of PG depends on the presence of an associated underlying disease [3]:
- In inflammatory bowel disease or rheumatoid arthritis, TNF-alpha inhibitors (infliximab, adalimumab, etanercept) are the first choice as monotherapy or in combination with glucocorticoids. Administration of ciclosporin A, IVIG, or other immunosuppressants (e.g., MTX, azathioprine) as monotherapy or combination therapy is also possible.
- In cases of underlying malignancy, IVIG is initially recommended as monotherapy or in combination with glucocorticoids. In addition, TNF-alpha inhibitors or immunosuppressants may be used depending on the activity of the malignancy.
- In PG of other causes, glucocorticoids are agents of first choice. Again, therapy with TNF-alpha inhibitors, immunoglobulins, or immunosuppressants may be considered [3].
If the aforementioned approaches do not improve pyoderma gangraenosum, a therapeutic trial with other biologics may be appropriate [3].
Calciphylaxis
Calciphylaxis is a rare and life-threatening arteriolopathy that in most cases results from disturbances in calcium-phosphate balance and resulting calcification of the media with consecutive vascular occlusion. Among other features, it is characterized by bizarrely configured necrotic ulcers (Fig. 3) and is frequently associated with nephropathy, dialysis dependency, and renal transplantation [1].

In addition, hyperparathyroidism, albumin deficiency, obesity, and the use of certain medications are risk factors for the development of calciphylaxis. These include coumarin-containing anticoagulants, corticosteroids, calcium supplements, and active vitamin D [7].
Diagnosis is made on the basis of the clinical picture, history, and a histologic triad of
- Intimal hyperplasia, fibrosis, vascular thrombosis.
- Calcification of the media
- Necrosis of epidermis, surrounding dermis and subcutis.
Due to possible organ involvement and often multimorbid patients, this clinical picture has a high mortality rate [1]. In addition, there are also non-uremic forms of calciphylaxis, for which, however, no uniform therapeutic recommendations exist due to the lack of randomized studies [5].
Multidisciplinary patient care by nephrologists, dermatologists, specialized wound experts, nutritionists and pain therapists is also important for therapy in these cases. There is no specifically approved systemic therapy. In the uremic form of calciphylaxis, regulation of calcium and phosphate balance via dialysis or medication may be considered, as a reduction in calcium and phosphate levels shows beneficial effects. Other drugs have also been used successfully in case series, such as sodium thiosulfate. It forms hydrophilic complexes with metals and minerals and must be applied intravenously several times a week. Other case reports on the use of cinacalcet or bisphosphonates are also available. Because of the described association of the occurrence of calciphylaxis with the use of vitamin K antagonists, coumarin medication should be implemented in patients with calciphylaxis or vitamin K substitution should be performed on a case-by-case basis [1].
|
Excursus Biologics Biologics are artificially produced proteins that intercept messenger substances for inflammation or block their signal transmission. These are very expensive therapies, most of which are still used off-label for the indications presented here. One problem with biologics is the risk of reactivation of latent infections, increased susceptibility to infection, and possible alteration of the blood count. In addition, contraindications such as decompensated heart failure, pre-existing serious infections, pregnancy, severe liver disease or history of malignancy must be considered. |
Necrobiosis lipoidica
Necrobiosis lipoidica (NL) is an inflammatory, non-infectious skin disease, the exact cause of which is not clear. It occurs especially in patients with diabetes mellitus (0.3-1% of all diabetic patients) and may appear even before the diagnosis of diabetes. About 50% of all patients with NL have other metabolic syndrome disorders. Thyroid disorders also appear to be clustered in this patient group [1].
Inflammatory breakdown of collagen with granulomatous tissue reaction in the dermis, sometimes also in the subcutaneous adipose tissue, initially results in painless, red papules or plaques, which later turn yellowish to brownish and increase in size. The typical picture of necrobiosis lipoidica is lesions with a yellowish center and dark brown surrounding area with raised, inflammatory active margins. Efflorescences may also occur on the forearms, hands and trunk. Unusual locations, such as the scalp or genital area, may also occur [1]. In about 30% of NL cases, therapy-resistant ulcerations occur in the affected skin areas.
In case of an association with diabetes, the optimal adjustment of blood glucose levels is initially the most important step. Systemically and topically, NL is treated with glucocorticoids. Possible alternatives include fumaric acid esters, ciclosporin A, dapsone, and anti-malarial agents such as (hydroxy)chloroquine. Biologics such as TNF-alpha inhibitors (e.g., adalimumab) can also be used, but because of their off-label use, they should be used with caution and detailed patient education about potential side effects [1]. Nevertheless, due to the rarity of the disease, randomized studies and clear treatment guidelines are lacking.
The use of Janus kinase (JAK) inhibitors is new. Good response to therapy, including ulceration, in patients with necrobiosis lipoidica suggests a link between the JAK-STAT pathway and the pathogenesis of the disease [8].
Livedovasculopathy
Livedovasculopathy (LV) is characterized by recurrent, very painful ulcerations primarily in the ankle region, the course of which is typically divided into three stages [10]. In the first stage, a livedo racemosa pattern appears in the wound area. These are livid, irregularly circumscribed, reticular macules caused by inadequate perfusion. Tissue ischemia results from the underperfusion in the second stage. Due to obliterative vasculopathies and microemboli, cutaneous ischemia and necrotic ulcerations (“skin infarcts”) occur. Superficial capillaries are particularly affected. In the last stage, partly chronic, scarring remodeling processes take place, the so-called atrophie blanche forms. These are lightning or star-shaped, porcelain-colored scars [11].
Early initiation of drug therapy is necessary to prevent worsening of the ulcerations in terms of scarring of the skin infarcts. The period between the onset of the first symptoms and the diagnosis should be shortened as much as possible. All current therapies are off label for livedovasculopathy [10,11]. An S1 guideline was also recently published for livedovasculopathy [11].
For systemic treatment, anticoagulants are agents of first choice because of the pro-coagulant mechanisms that contribute to disease development. Low-molecular-weight heparin (NMH) and direct oral anticoagulants (DOAKs, e.g., dabigatran, rivaroxaban) are used [1]. Therapy with low-molecular-weight heparin leads to rapid improvement in most cases [11].
Low-molecular-weight heparin at full therapeutic doses is recommended for initial diagnosis of livedovasculopathy or exacerbation. If the findings are stable or the ulcerations have healed, the dose can be reduced and the drug discontinued completely if necessary. If there is a risk of deterioration, therapy should be continued or switched to rivaroxaban, a factor Xa inhibitor. Potential clinical worsening of ulceration can be identified by increasing pain and can be detected early by keeping a pain diary [11].
Intravenous immunoglobulins represent an important therapeutic alternative (off label). In addition, vitamin K antagonists or iloprost may be used. The administration of vitamins B6, B12, and folic acid in addition to anticoagulation also shows beneficial effects in patients with hyperhomocysteinemia [11]. In addition, rheologics such as cilostazol, naftidrofuryl, and pentoxifylline should be considered in therapy-resistant individual cases [5].
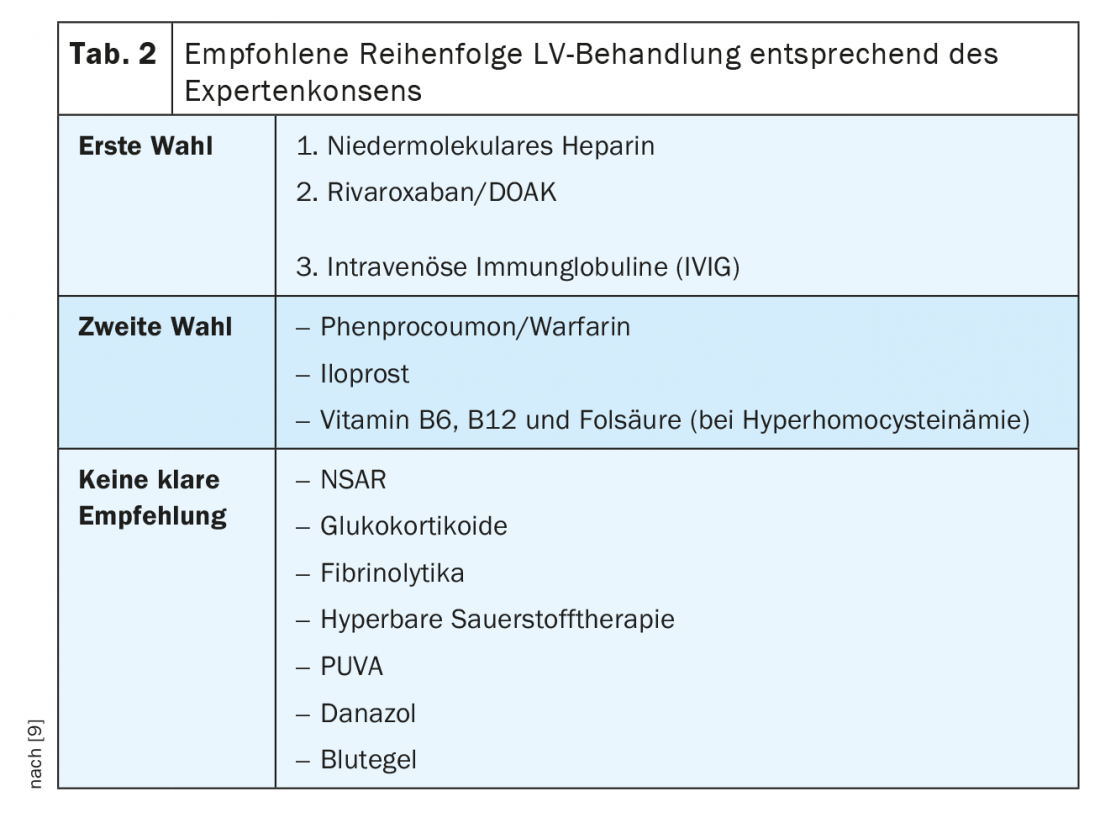
Table 2 summarizes the recommendations of the guideline again.
Conclusion for practice
For most of the diseases mentioned, the evidence for treatment recommendations is currently largely derived from clinical experience and various case reports in small patient populations rather than from randomized trials. Therefore, the majority of the therapies used are still off-label uses. However, these new therapies, particularly the increasing use of biologics and Janus kinase inhibitors, are very promising and allow for a broader spectrum of available therapeutics in the treatment of dermatologic wounds. The initial diagnostic workup of the cause of the chronic wound remains crucial for targeted therapy.
Take-Home Messages
- Diagnosis and therapy of the underlying disease are the starting point of a goal-oriented treatment of chronic wounds.
- Interdisciplinary involvement of various medical specialties is often required.
- Newer systemic therapy options are promising, but should be used judiciously.
- Drugs that cause or aggravate ulcers and individual risk factors must also be considered.
Literature:
- Dissemond J, et al: Systemic therapies for leg ulcers. J Dtsch Dermatol Ges 2018; 16(7): 873-890.
- Erfurt-Berge C, Renner R: Chronic wounds – Recommendations for diagnostics and therapy. J Reviews in Vascular Medicine 2015; 3(1): 5-9.
- AWMF, S1 Guideline Pyoderma gangrenosum 2020. www.awmf.org/uploads/tx_szleitlinien/013-091l_S1_Pyoderma-gangrenosum_2020-10_1.pdf (last accessed 03/06/2022).
- Jockenhöfer F, et al: The PARACELSUS score: a novel diagnostic tool for pyoderma gangrenosum. Br J Dermatol 2019; 180: 615-620.
- Erfurt-Berge C, Renner R: Interdisciplinary approach in diagnosis and therapy of leg ulcers. Geriatrics up2date Thieme 2022; 04(01): 41-55.
- Quist SR, Kraas L: Therapeutic options in pyoderma gangraenosum. J Dtsch Dermatol Ges 2017; 15(1): 34-41.
- Erfurt-Berge C, Renner R: Management of patients with calciphylaxis: current perspectives. Chronic Wound Care Management and Research 2019; 6: 109-115.
- Erfurt-Berge C, Sticherling M: Successful treatment of ulcerative necrobiosis lipoidica with janus kinase inhibitor. Journal of the European Academy of Dermatology and Venereology 2020; 34(7): 331-333.
- Shreberk-Hassidim R, et al: Janus kinase inhibitors in dermatology: A systematic review. J Am Acad Dermatol 2017; 76(4): 745-753.
- Schiffmann M, et al: S1 Guideline Diagnostics and Therapy of Livedovasculopathy. JDDG – Journal of the German Dermatological Society 2021; 19(11): 1667-1678.
- Görge T, et al: S1 Guideline Diagnostics and Therapy of Livedovasculopathy 2021. www.awmf.org/uploads/tx_szleitlinien/013-098l_S1_Diagnostik-Therapie-Livedovaskulopathie__2021-02.pdf (last accessed: 03/06/2022).
DERMATOLOGIE PRAXIS 2022; 32(3): 6-11