With a median survival of about two years, the prognosis for metastatic colorectal cancer remains poor. New therapeutic options have brought some improvement in recent years, but major breakthroughs have been lacking. This year’s ASCO Annual Meeting was again all about the details. And yet, some exciting insights into optimizing first-line therapy were presented.
Even with established first-line therapy for metastatic colorectal cancer, many questions remain. For example, it is unclear whether the addition of an anti-EGFR antibody is superior to that of the anti-VEGF antibody bevacizumab to FOLFOXIRI in tumors without a RAS mutation. So far, this has only been prospectively investigated for FOLFIRI – and even here it has not yet been conclusively clarified. Another question on which prospective data were presented for the first time at this year’s ASCO Annual Meeting is that of the benefit of treatment directed against EGFR in the presence of a BRAFV600E mutation. In addition, the focus was on optimizing maintenance therapy.
Therapy Intensification: Battle of the Points of Attack
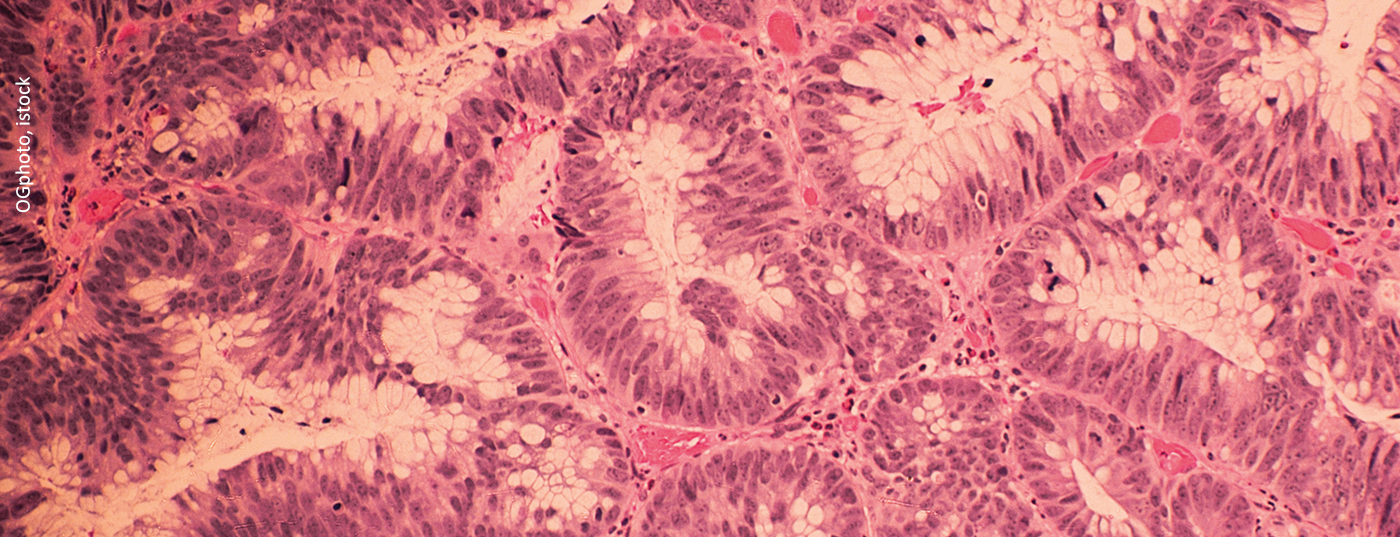
Depending on the localization of the tumor and the presence of mutations, chemotherapy in metastatic colorectal cancer is now supplemented by an anti-EGFR antibody or the antibody bevacizumab directed against VEGF. Thus, bevacizumab is used particularly in right-sided, RAS- or BRAF-mutated tumors (Fig. 1) [1]. If neither a RAS nor a BRAF mutation is present, an anti-EGFR antibody such as cetuximab is usually used in addition to chemotherapy. In particular, the use of cetuximab in BRAF-mutated tumors and the superiority of anti-EGFR antibodies in RAS wild-type colorectal carcinomas were scrutinized more closely at the ASCO Annual Meeting. The conclusion of the two studies: For the time being, everything will probably remain as it is. But based on a broader data set.

The extent to which preferential administration of cetuximab is warranted in tumors without RAS mutation was investigated by the Japanese phase II DEEPER trial [2]. It was the first to compare the addition of cetuximab with that of bevacizumab to FOLFOXIRI (folinic acid, 5-fluorouracil, oxaliplatin, irinotecan) in first-line treatment. Several years ago, the two agents were already directly compared in this indication, but at that time in combination with FOLFIRI (folinic acid, 5-fluorouracil, irinotecan) [3]. In left-sided tumors, the latter study showed superiority of the anti-EGFR antibody cetuximab in terms of overall survival, but no difference in progression-free survival (PFS) was observed. In a depth-of-response analysis, tumors shrank by a median of 48.9% with cetuximab treatment and 32.3% with bevacizumab administration [4]. Similar results were presented from the recent DEEPER study, which included 360 patients. Again, the median depth of response was greater with cetuximab than with bevacizumab – and this was independent of tumor location, although the effect was more pronounced in left-sided tumors. No statistically significant differences were seen with regard to overall response rate, which was approximately 70%, disease control rate, and R0 resection rate. However, the proportion of complete remissions was higher with cetuximab, 6.3%, than with bevacizumab, 2.3%. Median overall survival (OS) and PFS were presented for both arms only together and were 37.6 and 12.7 months, respectively – good values overall. In summary, FOLFOXIRI + cetuximab appears to be superior, particularly in left-sided, RAS wild-type tumors. However, the transferability of the depth of response to PFS and OS cannot be assessed at this time.
Unlike colorectal carcinomas without RAS mutation, the use of the anti-VEGF antibody bevacizumab is recommended for those with BRAFV600E mutation. However, no prospective data existed to date on the use of anti-EGFR antibodies in first-line metastatic BRAFV600E-mutated, RAS wild-type tumors. Two meta-analyses with the same data basis came to contradictory results regarding this question [5,6]. For the first time, the randomized phase II FIRE-4.5 trial now provided a prospective investigation [7]. Including 109 patients, the addition of bevacizumab to up to 12 cycles of FOLFOXIRI was compared with that of cetuximab. Regarding the primary endpoint of objective response rate (ORR), bevacizumab showed a numerical advantage with an ORR of 60%, compared with 49.2% with cetuximab treatment, but without statistical significance. Disease control rate and OS also tended to be better with bevacizumab, but without reaching statistical significance. The trend in favor of the anti-VEGF antibody persisted across all subgroups, but was particularly pronounced in those over 65 years of age and in men. Overall, the addition of bevacizumab in BRAFV600E-mutated tumors appears to be superior to that of cetuximab, making treatment appropriate based on current guidelines. What the results cannot hide is the still extremely poor prognosis in this group of patients – with treatment with bevacizumab and FOLFOXIRI, the median PFS was 10.1 months with a median overall survival of only 17.1 months. The medical need for better therapeutic options remains high. A possible ray of hope could be the currently ongoing BREAKWATER study. This investigates the combination of chemotherapy with the BRAF inhibitor encorafenib and cetuximab in patients with metastatic colorectal cancer with BRAFV600E mutation.
News on maintenance therapy
Two interesting studies were also presented at the ASCO Annual Meeting in the area of maintenance. On the one hand, the focus was on the optimal maintenance therapy in patients receiving FOLFOX (folinic acid, 5-fluorouracil, oxaliplatin) in combination with the anti-EGFR antibody panitumumab in the first line of therapy. On the other hand, maintenance therapy with capecitabine was compared with a pause in therapy. Progression-free survival was well below one year in all cases – and in all cases, careful cost-benefit consideration must be made.
After previously confirming the superiority of 5-fluorouracil (5-FU)/folinic acid (LV) maintenance therapy in combination with panitumumab over panitumumab alone, the PANAMA trial now addressed the question of whether the combination of 5-FU/LV and panitumumab is also superior to 5-FU/LV alone [8]. For this purpose, the authors investigated both options in patients with metastatic colorectal cancer without RAS mutation who had previously received FOLFOX panitumumab. To date, 5-FU/LV has been the standard backbone of most maintenance therapies. And the PANAMA study clearly shows that this backbone should be supplemented by panitumumab in appropriately pretreated patients. This is because from the time of randomization, i.e., after first-line therapy, the median PFS with 5-FU/LV + panitumumab was 8.8 months, compared to 5.7 months with 5-FU/LV maintenance therapy alone (p=0.014). Overall survival data remain to be seen.
The usefulness of maintenance therapy per se was questioned in the FOCUS4-N trial [9]. This compared maintenance with capecitabine with surveillance of patients with metastatic colorectal cancer whose disease was stable after 16 weeks of first-line treatment. Tumor progression and quality of life of the included 254 patients were analyzed. Previous studies have shown that a combination of capecitabine and bevacizumab prolongs PFS but does not appear to have statistically significant effects on overall survival [10]. The FOCUS4-N trial also demonstrated a significant PFS benefit with maintenance therapy. While the median PFS with capecitabine was 8.84 months, it was a meager 1.87 months without therapy. However, there were no differences in terms of quality of life and significant toxicity with capecitabine treatment. In particular, there was clustered diarrhea, nausea, fatigue, and polyneuropathy. Accordingly, maintenance therapy must be discussed in detail, taking various factors into account, as opposed to the so-called treatment holiday. This is because maintenance with currently available agents prolongs the time until second-line therapy is needed, but also brings toxicity.
Source: “Lower GI Cancer” highlight lecture, Prof. Sebastian Stintzing, MD, ASCO Direct, June 08, 2021.
Literature:
- Hofheinz R-D, et al: Colon cancer – Onkopedia 2018. www.onkopedia.com/de/onkopedia/guidelines/kolonkarzinom/@@guideline/html/index.html#ID0ER3AE (last accessed 07/03/2021).
- Tsuji A, et al: The randomized phase II trial of FOLFOXIRI plus cetuximab versus FOLFOXIRI plus bevacizumab as the first-line treatment in metastatic colorectal cancer with RAS wild-type tumors: the DEEPER trial (JACCRO CC-13). Journal of Clinical Oncology. 2021; 39(15_suppl): 3501.
- Heinemann V, et al: FOLFIRI plus cetuximab or bevacizumab for advanced colorectal cancer: final survival and per-protocol analysis of FIRE-3, a randomised clinical trial. Br J Cancer. 2021; 124(3): 587-594.
- Stintzing S, et al: FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): a post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol. 2016; 17(10): 1426-1434.
- Rowland A, et al: Meta-analysis of BRAF mutation as a predictive biomarker of benefit from anti-EGFR monoclonal antibody therapy for RAS wild-type metastatic colorectal cancer. Br J Cancer. 2015; 112(12): 1888-1894.
- Pietrantonio F, et al: Predictive role of BRAF mutations in patients with advanced colorectal cancer receiving cetuximab and panitumumab: a meta-analysis. Eur J Cancer. 2015; 51(5): 587-594.
- Stintzing S, et al: Randomized study to investigate FOLFOXIRI plus either bevacizumab or cetuximab as first-line treatment of BRAF V600E-mutant mCRC: The phase-II FIRE-4.5 study (AIO KRK-0116). Journal of Clinical Oncology. 2021; 39(15_suppl): 3502.
- Modest DP, et al: Maintenance therapy with 5-fluorouracil/leucovorin (5FU/LV) plus panitumumab (pmab) or 5FU/LV alone in RAS wildtype (WT) metastatic colorectal cancer (mCRC) – the PANAMA trial (AIO KRK 0212). Journal of Clinical Oncology. 2021; 39(15_suppl): 3503.
- Adams R, et al: Oral maintenance capecitabine versus active monitoring for patients with metastatic colorectal cancer (mCRC) who are stable or responding after 16 weeks of first-line treatment: results from the randomized FOCUS4-N trial. Journal of Clinical Oncology. 2021; 39(15_suppl): 3504.
- Goey KKH, et al: Maintenance treatment with capecitabine and bevacizumab versus observation in metastatic colorectal cancer: updated results and molecular subgroup analyses of the phase 3 CAIRO3 study. Ann Oncol. 2017; 28(9): 2128-2134.
InFo ONCOLOGY & HEMATOLOGY 2021; 30-32