Pathophysiologically, a disturbed skin barrier with a lack of natural moisturizing factors and altered lipid and protein composition plays a key role in atopic dermatitis. Restoring physiological skin barrier function is an important therapeutic goal. Consistent basic care with lipid-containing, hydrating topical topicals is therefore an important pillar in the successful management of atopic dermatitis. This is especially true for infants and young children.
Neurodermatitis (synonym: atopic dermatitis) is the most common chronic inflammatory skin disease in childhood [1]. The most important leading symptoms are eczema at age-dependent typical predilection sites and excruciating pruritus [2]. The prevalence of atopic dermatitis in children in Central Europe is about 10-15%, with the majority of symptoms appearing in the first year of life [3–5]. From 2 to 12 years of age, the typical chronic eczema of childhood is found with involvement of the large flexures and dry skin (xerosis cutis) [1]. In the vast majority, atopic dermatitis manifests by the fifth year of life; only about 10% do not develop eczema until the seventh year of life [5].
Skin barrier defect and itch-scratch circuit as pathomechanisms.
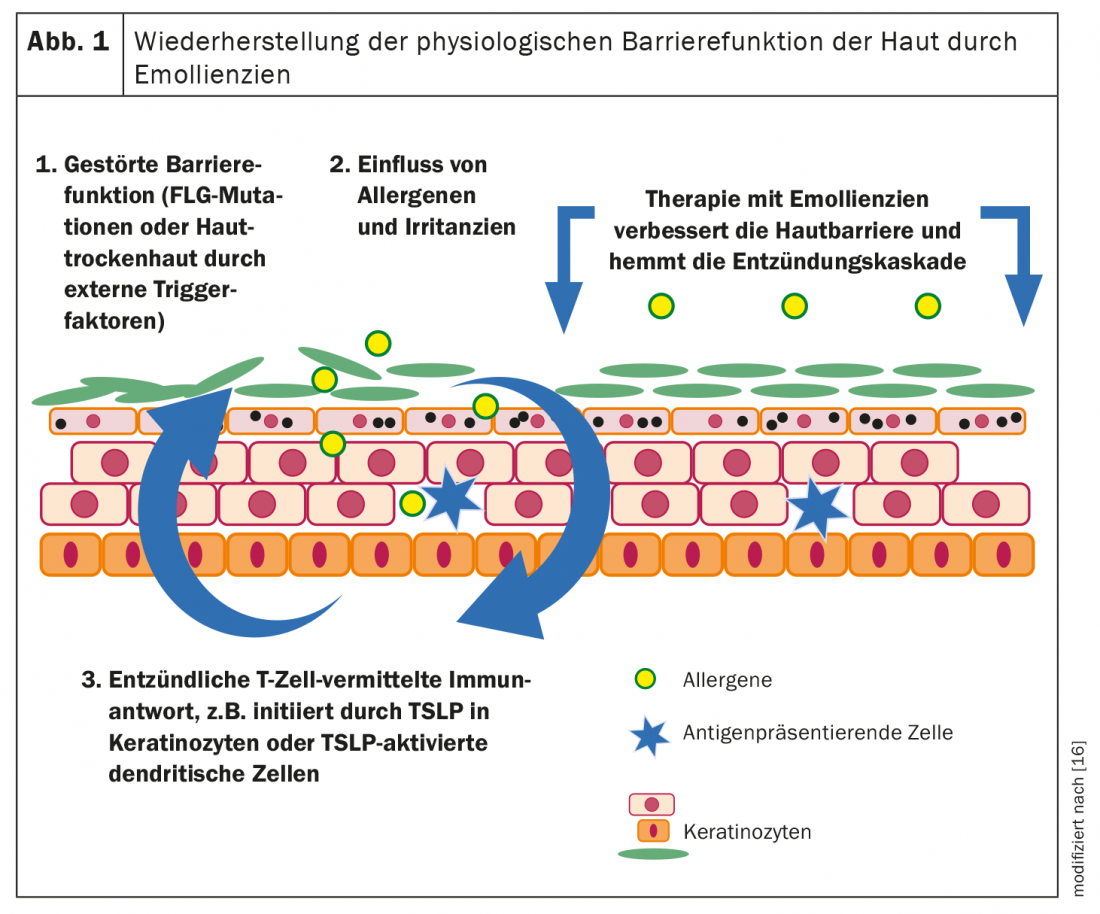
Neurodermatitis is based on a multifacorial pathogenesis. A genetically determined disturbance of epidermal barrier function and characteristically altered immune responses are pathophysiologically relevant processes. The structure of the epidermal barrier shows specific alterations in atopic skin. If the protective mantle of the epidermis is inadequate, exogenous factors can penetrate the skin more easily, which further weakens the skin barrier and provokes eczema flare-ups (Fig. 1). Trigger factors that initiate or exacerbate a cutaneous inflammatory response include microbial, irritant, allergenic, or nonspecific irritants [7–9].
A cutaneous inflammatory response may result in an itch-scratch cycle, which can aggravate symptoms and promote acute exacerbations [6–8]. This is because scratching triggers inflammatory processes and contributes to a deterioration of the already defective skin barrier, leading to the release of epidermal cytokines that activate cells in the dermis, which in turn produce increased proinflammatory factors, which in turn increase inflammation and itching [25].
“Natural Moisturizing Factor” regulates transepidermal water loss
Genetic loss-of-function mutations in the filaggrin gene can lead to filaggrin deficiency [10]. Filaggrins are proteins with an important structure-forming function for the skin barrier. In the upper layers of the stratum corneum, filaggrin is degraded to pyrrolidone carboxylic acid, urocanic acid and free amino acids, which together form the so-called “natural moisturizing factor” (NMF), which is essential for the water-binding capacity of the stratum corneum [11]. Healthy skin should normally be able to retain 10-20% water for ensuring an intact barrier function [11]. For such moisture content of the skin, a functioning intercellular lipid layer, proper arrangement and differentiation of corneocytes with sufficient content of natural moisturizing factor (NMF) is crucial [11]. Due to its water-retaining effect, NMF reduces transepidermal water loss (TEWL).
Basic care with hydrating and refatting emollients is central
The therapy of neurodermatitis depends on the course and severity of the symptoms and follows a graduated scheme. Adequate basic therapy can prevent an itch-scratch cycle and thus extend the recurrence-free interval. In addition to a reduction of provocation factors, this is based in particular on the use of emollients – i.e. topical externals which have lipid-replenishing properties and are free of active ingredients. The regular use of emollients is useful in several respects [12]:
- Xerosis cutis is a common problem in atopic dermatitis
- Dry skin leads to itching and burning sensation
- If the skin is dried out, there is an increased risk of inflammation
- Skin dryness is associated with a barrier defect and a disturbed skin barrier can promote allergic sensitization
Basic topical skin care is recommended in national and international guidelines not only for interval treatment but for all stages and severities of atopic dermatitis [13–15]. First, consistent basic care is an essential factor for regeneration of the impaired barrier function, as well as for reduction of xerosis and itch symptoms (Fig. 1) [9,24]. Second, acute eczema episodes require less topical steroids.
Use care products suitable for infants and young children
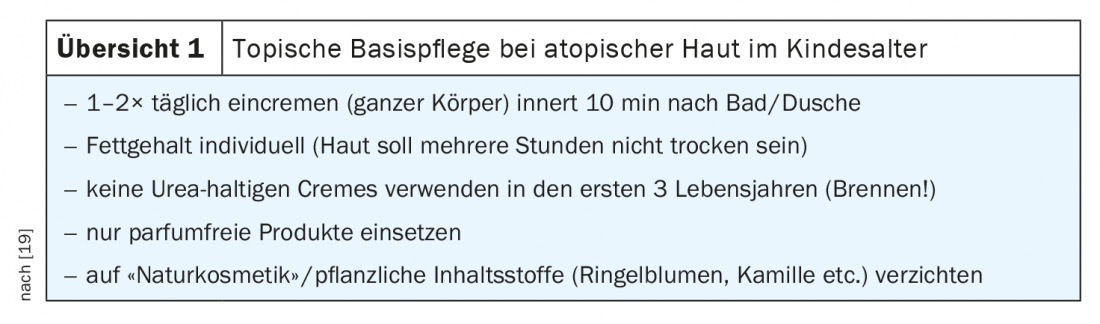
Dry skin should be treated 1-2× daily with re-hydrating lotions, creams or ointments to achieve adequate oil and moisture content and to strengthen the skin barrier (overview 1) [17]. Suitable basic therapeutics should on the one hand ensure a good and sustained supply of lipids and moisture to the skin and on the other hand be hypoallergenic. Studies show that starting basic care as early as three weeks of age in infants with a family history of atopy can reduce the development of atopic dermatitis by up to 50% [16,17]. However, the use of preparations containing urea should be avoided in infants and young children, as even low concentrations of these preparations cause burning sensations on the skin in children up to the age of five (“stining” effect) [18]. Basic care products with moisturizing active ingredients that do not contain urea are, for example, formulations based on glycerin or lactic acid and almond oil. Lactic acid derivatives are among the active ingredients of NMF [11], the natural moisturizing factor that hydrates the cornea and reduces transepidermal water loss (TEWL).
|
Neurodermatitis training Education programs for parents and children also play an important role in optimal patient care, and evidence-based benefit has been demonstrated in several randomized-controlled trials [21,22]. Participants are taught practical knowledge about their disease and the therapeutic principles derived from it. Particularly important is the understanding of adequate local therapy including systematic skin care and the selection of skin care products appropriate for the skin condition. Daily skin care with moisturizers, sometimes several times a day, is essential [23]. |
Apart from regular application of cream, daily lukewarm bathing or showering with mild washing lotions and anti-allergic, lipid-replenishing oil additives is recommended for children with atopic skin. In addition to removing microbes and ointment residues, this hydrates the skin and subsequently applied creams are better absorbed [19]. In neurodermatitis training courses, theoretical and practical know-how relevant to everyday life is imparted for disease management in everyday life; these are interdisciplinary, regional offers (box) .
Literature:
- Aberer W, et al: Neurodermatitis. Expert statement. Austrian Medical Journal, September 2019.
- Bieber T: N Engl J Med 2008; 358(14): 1483-1494.
- Schnopp C, Mempel M: Dermatologist 2015; 66: 245-251.
- Weidinger S, Novak N: The Lancet 2016; 387: 1109-1122.
- Bieber T, et al: J Allergy Clin Immunol 2017; 139(4S): S58-S64.
- Rerknimitr P, et al: Inflamm Regen 2017; 37: 14.
- Volz T, et al: Dermatologist 2015; 66: 90-95.
- Biedermann T, et al: Front Immunol 2015; 6: 353.
- Chylla R, Schnopp C, Volz T: JDDG 2018; 16 (8): 976-980.
- Engebretsen KA, Thyssen JP: Karger Compass Dermatol 2017; 5: 7-13.
- Augustin M, et al: Position paper: diagnosis and therapy of xerosis cutis. JDDG 2018; 16 Suppl 4: 3-35.
- Neurodermatitis [atopic eczema; atopic dermatitis] long version 2014; AWMF, registry number: 013-027 (as of 03/2015).
- Eichenfield LF, et al: J Am Acad Dermatol 2014; 71: 116-132.
- Werfel T, et al: JDDG 2016; 14: 92-106.
- Wollenberg A, et al: J Eur Acad Dermatol Venereol 2018; 32: 657-682.
- Simpson EL, et al: J Allergy Clin Immunol 2014; 134: 818-823.
- Horimukai K, et al: J Allergy Clin Immunol 2014; 134: 824-830.
- Deutsche Apotheker Zeitung: www.deutsche-apotheker-zeitung.de/daz-az/2018/daz-38-2018/hochempfindlich, (last accessed 05.08.2021)
- Weibel L: Pediatric Dermatology – Successfully Treating Common Dermatoses, www.kispi.uzh.ch/de/zuweiser/fachbereiche/dermatologie/Documents/Handout_Davos_2017_Weibel.pdf (last accessed 08/05/2021).
- Deutsche Allergie- und Hauthilfe, e.V., www.dha-neurodermitis.de/therapie/basistherapie.html, (last accessed 05.08.2021).
- Heratizadeh A, et al: Dermatologist 2018; 69: 225-231.
- Staab D, et al: BMJ 2006; 332(7547): 933-938.
- Knoll Ch, et al. Professional association of pediatricians and adolescents in practice. 03 / 2014: 14-15.
- Grether-Beck S, et al: J Invest Dermatol 2012; 132(6): 1561-1567.
- Kim B, Lio P: Confronting Issues and Challenges Beneath the Surface: Biology and Pathophysiology of Eczema, www.hmpgloballearningnetwork.com/site/thederm/article/confronting-issues-and-challenges-beneath-surface-biology-and-pathophysiology-eczema (last accessed Aug. 05, 2021).
DERMATOLOGIE PRAXIS 2021; 31(4): 23-24











