When dealing with allergy patients, frustrating situations can easily arise in everyday life, both for those affected and for the doctors treating them: As a patient, one is disappointed because the therapy does not have the hoped-for effect; as a physician, one is dissatisfied because the allergy sufferer does not adhere to the medication regimen despite comprehensive information. Often, this is simply due to misunderstandings that can be easily resolved.
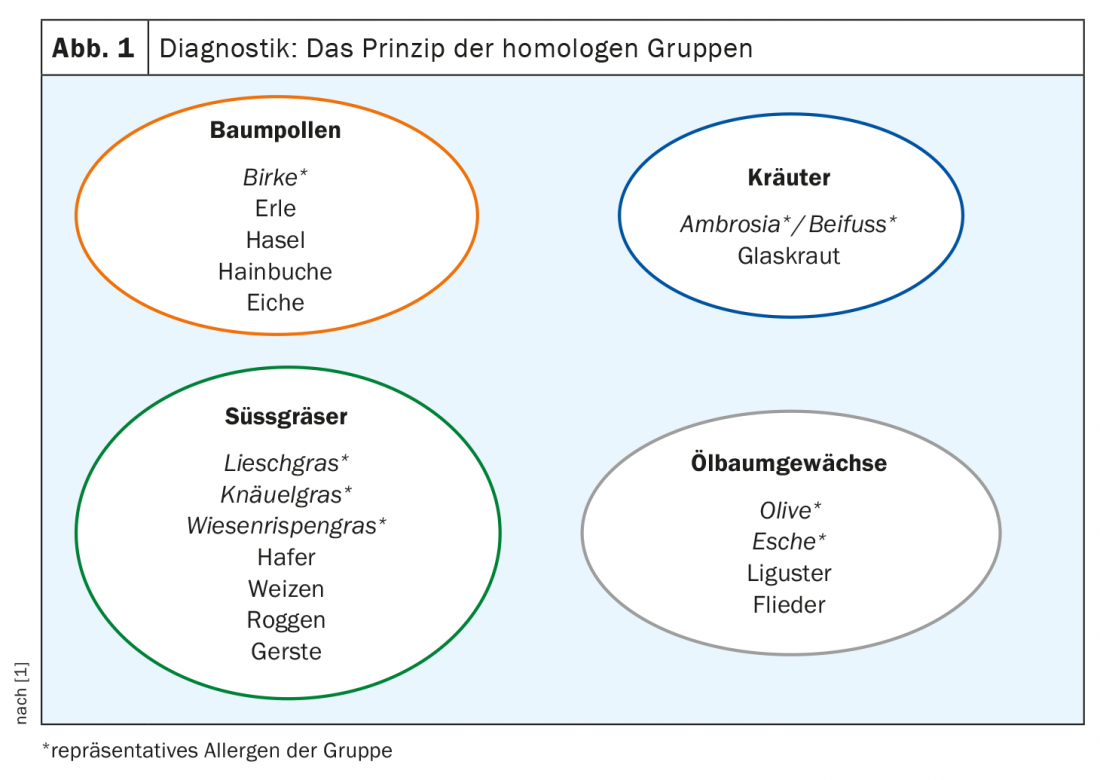
It already starts with diagnostics, where Prof. Dr. Natalija Novak, Clinic and Polyclinic for Dermatology and Allergology, University Hospital Bonn, recommends the motto “keep it simple”. According to the principle of homologous groups, the birch pollen allergen, for example, can be taken as representative for tree pollen and thus alder, hazel, hornbeam and oak can be included, both in diagnostics and in therapy. Similarly, timothy grass, knapweed and bluegrass can be used as representative allergens of the sweet grass group, which also includes oats, wheat, rye and barley due to their high cross-reactivity (Fig. 1).
When selecting the appropriate form of therapy, Prof. Novak considers it the physician’s task to work with the patient to find the best option for him or her. There are a few things to keep in mind: When choosing between subcutaneous (SCIT) and sublingual immunotherapy (SLIT), there are various preparations available, and as a treatment provider you should also take a look at the studies on which their approvals are based. The patient’s wishes should also be listened to: Some patients prefer to be “kept on a short leash”, i.e. they say themselves that they need regular monitoring. For other patients, it is logistically impossible to come to the practice or clinic every four weeks and wait half an hour after the injection. The expert recommends that physicians pay attention to previous compliance experiences, especially with patients they have known for a long time. And at the level of contraindications, he said, patients with cardiovascular disease who are taking beta blockers, for example, have somewhat more freedom in the area of sublingual immunotherapy because the safety profile is better.
|
Side effect management
|
Side effects are our friends!
Adherence to therapy is always a big issue with both SCIT and SLIT. “Here we have to find ways to build a commitment between doctor and patient.” According to Prof. Novak, the ideal solution is to conclude a written contract and have the patient sign it. Or even pledge to be available as a physician by phone or email. Especially with sublingual immunotherapy, he said, one can see patients dropping out of therapy during the first prescription. Here the possibility must be given to be able to address as a patient again short term inquiries.
Correct and sensitive patient management is the be-all and end-all for adherence, the Bonn allergist explained. “Set the right expectations” is the central starting point here. In the field of allergen-specific immunotherapy with aeroallergens, it must be said that even with the best possible and most effective preparation, it is first of all only a matter of reducing the symptoms and medication. Good effects can be achieved after just one year, but the best effects are achieved over a therapy period of three years – many patients, on the other hand, expect to have no symptoms at all after six months. On the other hand, one should also critically question oneself as a physician at re-presentation after the first year if, for example, the patient reports no symptom improvement at all.
Side effect management is also a process that takes time with allergen-specific immunotherapy. “First of all, the patient just has problems: especially when you start with a very high allergen dose in sublingual immunotherapy, the mast cells in the oral mucosa report and make side effects.” The physician has to get his patient through this phase, according to Prof. Novak. After all, he has to wait until the next pollen season to feel that the whole thing works. Education is therefore necessary, not least to make it clear to the patient that side effects are good per se, because they make you realize that the allergen really does arrive.
However, as a clinician, you also have the option of counteracting the side effects, such as administering an antihistamine 10 to 15 minutes before AIT or changing the target region in the mouth, for example, from the sublingual to the vestibular region, where the lower lip is adjacent to the teeth. It may also make sense to postpone taking the medication until the evening before going to bed instead of in the morning before work.
Two birds with one stone?
Most adult patients have sensitizations to multiple aeroallergens. That is, the effect of AIT on grass pollen in the spring is not so resounding, if directly thereafter the next allergy in the summer takes hold. The solution here can be a therapy that is directed against several allergens from the beginning. This not only better addresses different symptoms, but also multiple organ systems: for example, not only rhinoconjunctivitis complaints are treated, but also problems with the lungs. “After all, that’s also something that significantly increases patient retention and satisfaction,” Prof. Novak said. Her advice: It is quite reasonable to combine two different AIT, even in short intervals (about 4 weeks, when the side effects of the first preparation have leveled off).
Source: German Allergy Congress 2020, Wiesbaden (D)
Literature:
- German Allergy Congress 2020, Wiesbaden (D), Lunchsymposium “Let’s tALK about … allergology!”, ALK-Abelló.
InFo PNEUMOLOGY & ALLERGOLOGY 2020; 2(4): 28-29 (published 12/1/20, ahead of print).