Target values for blood pressure and LDL have become more stringent in recent years, so extended risk stratification may make sense. Hypertension and dyslipidemia are among the most important cardiovascular risk factors and are common comorbidities. Combination therapies in the form of a “single pill” strategy may be a key to success.
Cardiovascular disease is the second leading cause of death after cancer in Switzerland [1]. Hypertension and hypercholesterolemia/dyslipidemia are among the most important cardiovascular risk factors that can be influenced. According to the Global Burden of Disease Study published in the Lancet, hypertension tops the list of risk factors for disability-adjusted life years, ahead of smoking, diabetes, and obesity [2]. Adequate control of dyslipidemia and hypertension results in a significantly reduced overall patient risk. Lifestyle interventions alone are usually insufficient to achieve the recommended target values – most patients require pharmacotherapy. According to current consensus recommendations, substances with multiple effects are to be preferred. Statins, calcium channel blockers, and angiotensin-converting enzyme (ACE) inhibitors have led to significant improvement in relevant outcome parameters, and dual or triple therapy for coronary artery disease (CAD) has been shown to contribute to a significant reduction in major cardiovascular events [3].
Concept of risk-adapted treatment
Estimation of total cardiovascular risk is a component of all current European and North American guidelines [1]. Based on this, a risk-adapted treatment strategy is possible. The European Society of Cardiology (ESC) has published new guidelines on dyslipidemia in 2019, in which numerous points have been adapted or supplemented compared with the 2016 version. This concerns, among other things, new LDL-C target values, as well as new criteria for risk stratification – for example, through differentiations with regard to age, diabetes and renal insufficiency, as well as greater consideration of imaging and lipoprotein [1,4]. The AGLA risk calculator is the equivalent of the ESC-SCORE (“Systematic Coronary Risk Estimation”) used in Switzerland [5]. In contrast to the ESC-SCORE, the values of the AGLA online tool are not only based on mortality data, but nonfatal myocardial infarctions are also considered [1,5].
Very high cardiovascular risk (AGLA* score ≥10%) includes known CHD/atherosclerosis, type 1 or type 2 diabetes with end-organ damage (retinopathy, neuropathy, or microalbuminuria), and/or GFR <30 ml/min/1.73 m2. A high cardiovascular risk (AGLA* score >20%) is given by one or more of the following risk factors: total cholesterol >8 or LDL >4,9 mmol/l, blood pressure ≥180/110 mmHg, chronic renal insufficiency (GFR 30-59 ml/min), type 1 or type 2 diabetes present for more than 10 years without end-organ damage. Intermediate cardiovascular risk (AGLA* score ≥10-<20%) typically affects young diabetics (type 1: <35 years, type 2: <50 years) without other risk factors with a duration of diabetes <10 years.
With regard to blood pressure, the general target value is 140/90 mmHg; 140/80 mmHg would be better, explains Thilo Burkhard, MD, University Hospital Basel [6]. What has changed compared to the past: multilevel treatment and blood pressure target ranges are now defined [9]. Patient-specific (lower) target values vary according to age, comorbidities, and tolerability and can be determined using the following questions:
- Is the patient younger than 65 years?
- Is renal function good (eGFR >60 ml/min)?
- Is medication tolerability and compliance good?
If all three of these questions are answered “yes,” the following applies to the adapted target range: 120-129/70-79 mmHg. According to current guidelines, there is also a lower limit: 120 mmHg should not be undercut.
Combination therapy recommended instead of monotherapy
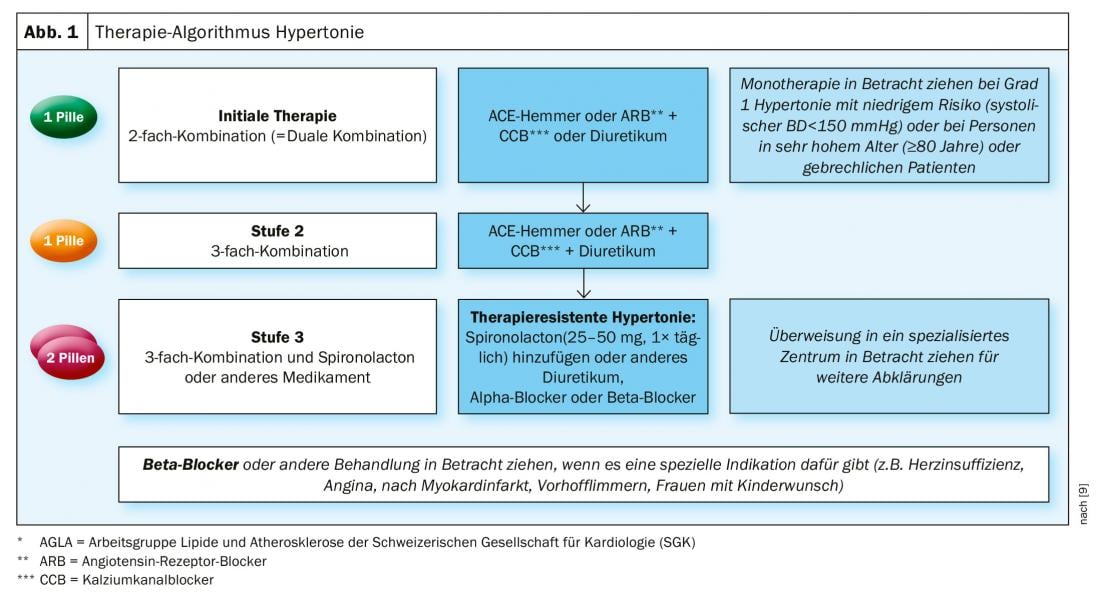
The current ESC/ESH guidelines on blood pressure management already initially recommend dual-combination antihypertensives (dual therapy). Monotherapy is now advised in most guidelines only in grade I hypertension (systolic BP <150 mmHg) and low cardiovascular risk [7]. In terms of dual therapy, the best studied are combinations of the following drug classes: Thiazide + ACE inhibitor/ ARB**, CCB*** + ACE inhibitor/ ARB** [8]. To improve treatment adherence, fixed combinations with only one tablet daily should be used if possible (“single pill” strategy). If the target values are not reached, it is possible to switch to a triple combination (“triple” therapy) – this usually achieves the target range. Truly refractory hypertension occurs in about 10% of cases, Dr. Burkhard said. In high-risk cardiovascular patients, two lipid-lowering agents are often additionally required to achieve target values below 70 mg/dl and below 55 mg/dl in high-risk patients, respectively [7]. In patients who have already suffered a second cardiovascular event within two years, LDL cholesterol should be lowered to below 40 mg/dl.
Ideally, this is done with one tablet (statin plus ezetimibe) [7]. The concept of using fixed combinations across indications to simplify therapy in patients who require both (antihypertensive plus statin) is relatively new. The goal: comprehensive vascular protection with only one tablet daily [7]. In Switzerland, for example, the combination preparation Triveram® [10] is available, which combines the three active ingredients atorvastatin (statin), perindopril arginine (ACE inhibitor) and amlodipine (calcium channel blocker) [8]. According to the speaker, prescribing a combination preparation not only makes sense in terms of adherence, but also from an economic point of view, as it is no more expensive than separate single-agent preparations.
Source: FOMF Basel
Literature:
- Riesen WF, et al: New ESC/EAS dyslipidemia guidelines: an annotated review by the AGLA. Swiss Medical Forum, Online Magazine, published 06.01.2020, https://medicalforum.ch
- GBD 2017 DALYs and HALE Collaborators: Global, regional and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Diease Study 2017. The Lancet 2018; 392(10159): 1859-1922.
- Bertrand ME, Vlachopoulos C, Mourad JJ: Triple Combination Therapy for Global Cardiovascular Risk: Atorvastatin, Perindopril, and Amlodipine. Am J Cardiovasc Drugs 2016; 16(4): 241-253.
- European Society of Cardiology: 2019 ESC Guidelines Dyslipidaemia (Management of). ESC Clinical Practice Guidelines. www.escardio.org/Guidelines
- AGLA: Lipids and Atherosclerosis Working Group of the Swiss Society of Cardiology (SGK), www.agla.ch
- Burkhard T: Treating hypertension and dyslipidemia “as a whole”. Thilo Burkhard, MD, University Hospital Basel, FOMF Basel, Jan. 31, 2020
- Dechend R, Derer W: Relevance of combination therapy for cardiovascular patients: Blood pressure and cholesterol lowering in focus – Update 2019. Prof. Dr. med. Ralf Dechend, Dr. med. Wolfgang Derer. CME-Verlag – Fachverlag für medizinische Fortbildung GmbH, www.cme-kurs.de/kurse/kombinationstherapie-fuer-kardiovaskulaere-patienten
- Huber F, Beise U: Hypertension, last modified 3/2019, mediX, www.medix.ch/wissen/guidelines/herz-kreislauf-erkrankungen/hypertonie.html
- Williams B, Mancia G: Ten Commandments of the 2018 ESC/ESH HTN Guidelines on Hypertension in Adults. European Heart Journal 2018; 39(33): 3007-3008.
- Triveram®, https://compendium.ch
GP PRACTICE 2020: 15(4): 28-29