Prophylaxis of scars represents an important component of successful wound management. Nowadays, a wide range of invasive and non-invasive measures is available. At the EADV Annual Congress, international experts gave an update on this.
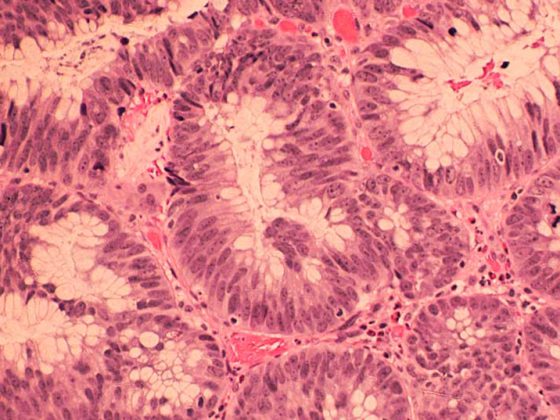
Regulation of wound healing and promotion of tissue regeneration are complex processes that have not yet been fully understood [1]. Scars differ from healthy skin in aesthetic, functional and morphological aspects. In the case of a small, superficial injury, only the epidermis is affected and a new intact skin layer can form starting from the basal cell layer. If the injury extends into the dermis, scar tissue remains, consisting of an accumulation of unpliable, poorly structured collagen fibers [2].
Prevent negative consequences of scars
In the case of scars resulting from burns, in addition to immediate negative consequences, there may be various long-term sequelae: Contractures and stiffness of joints, chronic pain, chronic itching, decreased sweating. On a psychological level, impairments in body perception, social anxiety and depressive disorders are possible sequelae.
Aleksejs Zavorins, MD, Riga, gave a presentation on prevention of scars and keloids at the EADV Annual Congress [1]. The goal in each case is to achieve a skin condition that is as scar-free as possible. It is known that this is sometimes achieved as part of a natural healing process. For example, there are reports of neogenesis of hair follicles, sebaceous glands, dermis, and cartilage in untreated mammals [3,4].
From analyses of the physiological and biochemical processes involved, important insights have been gained for the further development of scar prevention techniques.
Methods of scar prophylaxis
Botulinum tox in A is a neurotoxin (derivative of the anaerobic bacterial strain Clostridium botulinum) that leads to inhibition of the presynaptic release of acetylcholine. Side effects such as skin atrophy and telangiectasia had not occurred. The mechanism of action is not fully understood; there are several hypotheses: Reduction of wound tension; direct modulation of fibroblast activity by altering apoptotic, migratory and fibrotic pathways; inhibition of TGFα-1, VEGF, MMP1, PDGFA gene expression.
Mesenchymal stem cells can positively influence the wound healing process via paracrine activity and produce the following effects: Migration of fibroblasts and keratinocytes (in vitro); wound closure (in rat model); remodeling of extracellular matrix through synthesis of collagen and elastin; inhibition of MMP-1 expression (in vitro); expression of VEGF and angiogenesis (in rat model); suppression of inflammatory processes (lowering TNF-alpha and IL1) (in rat model) [5]. Split-thickness skin grafting is considered the standard treatment for large-area burn wounds. Possible complications of this procedure: pain, pruritus, infection, dyschromia, depigmentation, delayed healing, hypertrophic scarring. In addition, the availability of extraction sites is limited [6].
For sprays made from autologous skin substance, the skin of the donor site is placed in a specialized enzyme solution. These cells are then applied as a spray to a second-degree burn wound. Studies have demonstrated the non-inferiority of this technique compared to skin grafting. In addition, the spray technique offers the advantage that a suitable sampling site should be only 1/80 of the area of the injured area to be treated. This is much less than the 2:1 ratio required for split thickness skin grafting [6].
In terms of scaffolds to promote skin tissue regeneration after burns, there is a wide range of natural (collagen), synthetic (polycaprolactone) and hybrid materials available today, the speaker said. Scaffolds not only support cell migration, maintenance, and differentiation toward dermis restoration, but can also serve as carriers for cells or drugs [7]. Among others, a growth factor(TGF)β-1 inhibitor-based scaffold was developed, which can be used for the prevention of hypertrophic scars.
Pulsed dye laser (PDL) at a wavelength of 585-595 nm is strongly absorbed by oxyhemoglobin. The blood vessel walls are heated and coagulated or destroyed. This technique is used for the prevention of keloid and hypertrophic scars. PDL can lead to significant improvement including vascularization, pigmentation and pliability, the speaker said. Positive effects were also seen with regard to IGA (Investigators global assessment) and PGA (Participants global assessment) scores. In a comparative study, dye laser resulted in decreased expression of TGFβ-1, increased MMP activity, and decreased fibroblast proliferation and type III collagen production [9]. In the past, it was common to start treatment with dye laser only 6 months after trauma, nowadays some experts recommend to start therapy immediately after removal of sutures [10,11].
Radiotherapy after surgical excision resulted in a reduction in relapse rate compared with surgical excision alone. Especially in difficult-to-treat keloids, the use of radiotherapy is advisable, he said. X-rays can prevent relapses of keloids by controlling fibroblast proliferation and interrupting the cell cycle, including apoptosis. Brachytherapy, superficial and orthovolt irradiation resulted in the following effects [1,18,19]: The recurrence rate was reduced to 9.59%, which is a significantly better rate compared to surgical excision alone (45-100%). Higher relapse rates occurred in male gender, age <28 years, irradiation more than 24 hours after surgical intervention, size of keloids >5cm before skin grafting. No radiation-induced malignancies were observed after a median follow-up of 40 months and only a low rate of adverse events (9.38%).
Massage therapy resulted in reduction of pain (VAS), improvement of flexibility, reduction of vascularization (Vancouver scar scale), and reduction of depressive symptoms (CES-D) [1]. The speaker pointed out that the results were not based on fully standardized study protocols and that there were differences with regard to various scar characteristics as well as with regard to the massage technique used.
Source: EADV 2019, Madrid
Literature:
- Zavorins A: Scar and keloid prevention. Aleksejs Zavorins, MD. Scar and keloid prevention. Slide presentation, EADV Madrid, 10/10/2019.
- Lawrence JW, Mason ST, Schomer K: Epidemiology and impact of scarring after burn injury: a systematic review of the literature. J Burn Care Res 2012; 33(1): 136-146.
- Seifert AW, et al: Skin shedding and tissue regeneration in African spiny mice (Acomys). Nature 2012; 489 (7417): 561-565.
- Willyard C: Unlocking the secrets of scar-free healing. Nature 2018; 563 (7732): S86-S88.
- Yales CC, et al: Multipotent stromal cells/mesenchymal stem cells and fibroblasts combine to minimize skin hypertrophic scarring. Stem Cell Res Ther 2017; 8(1): 193.
- Holmes Iv JH, et al: A comparative study of the ReCell® device and autologous spit-thickness meshed skin graft in the treatment of acute burn injuries. J Burn Care Res 2018; 39(5): 694-702.
- Rahmani Del Bakhshayesh A, et al: Recent advantages on biomedical applications of scaffolds in wound healing and dermal tissue engineering. Artif Cells Nanomed Biotechnol 2018; 46(4): 691-705.
- Wang L, et al: Small Molecular TGF-β1-Inhibitor-Loaded Electrospun Fibrous Scaffolds for Preventing Hypertrophic Scars. ACS Appl Mater Interfaces 2017; 9(38): 32545-32553.
- Kuo YR, et al: Suppressed TGF-beta1 expression is correlated with up-regulation of matrix metalloproteinase-13 in keloid regression after flashlamp pulsed-dye laser treatment. Laser Surg Med 2005; 36(1): 38-42.
- Brewin MP, Lister TS: Prevention or treatment of hypertrophic burn scarring: a review of when and how to treat with the pulsed dye laser. Burns 2014; 40(5): 797-804.
- De las Alas JM, Siripunvarapon AH, Dofitas BL: Pulsed dye laser for the treatment of keloid and hypertrophic scars: a systematic review. Expert Rev Med Devices 2012; 9(6): 641-650.
- Prodromidou A, et al: Botulinum toxin for the prevention and healing of wound scars: a systematic review of the literature. Plast Surg (Oakv) 2015; 23(4): 260-264.
- Kasyanju Carrero LM, Ma WW, Liu HF: Botulinum toxin type A for the treatment and prevention of hypertrophic scars and keloids: Updated review. J Cosmet Dermatol 2019; 18(1): 10-15.
- Shojaei F, et al: A review on different methods to increase the efficiency of mesenchymal stem cell-based wound therapy. Wound Repair Regen 2019 Jul 12. doi: 10.1111/wrr.12749.
- Volarevic V, et al: Ethical and safety issues of stem cell-based therapy. Int J Med Sci 2018; 15(1): 36-45.
- Fong C-Y, et al: Human Wharton’s jelly stem cells and its conditioned medium enhance healing of excisional and diabetic wounds. J Cell Biochem 2014; 115(2): 290-302.
- Tam K, et al: A nanoscaffold impregnated with human wharton’s jelly stem cells or its secretions improves healing of wounds. J Cell Biochem 2014; 115(4): 794-803.
- Shen J, Lian X, Sun Y: Hypofractionated electron-beam radiation therapy for keloids: retrospective study of 568 cases with 834 lesions. J Radiat Res 2015; 56(5): 811-817.
- Cheraghi N, Cognetta A Jr, Goldberg D: Radiation therapy for the adjunctive treatment of surgically excised keloids: a review. J Clin Aesthet Dermatol 2017; 10(8): 12-15.
DERMATOLOGIE PRAXIS 2019; 29(6): 41-42 (published 9/12/19, ahead of print).