According to current evidence, there is no statistical benefit of general routine screening. However, this does not apply in the presence of cardiovascular risk factors.
Peripheral arterial occlusive disease (pAVD) refers to narrowed blood vessels due to arteriosclerosis, primarily in the arteries of the lower extremities. Risk factors include age, nicotine abuse, diabetes, hypercholesterolemia, and hypertension. The main symptoms include pain in the calf or thigh during movement, which subsides at rest. Possible clinical indications of pAVD include weakened peripheral pulse, stenosis sounds in the pelvis/groin, trophic changes in the skin, increased risk of ulceration.
In which cases is screening worthwhile?
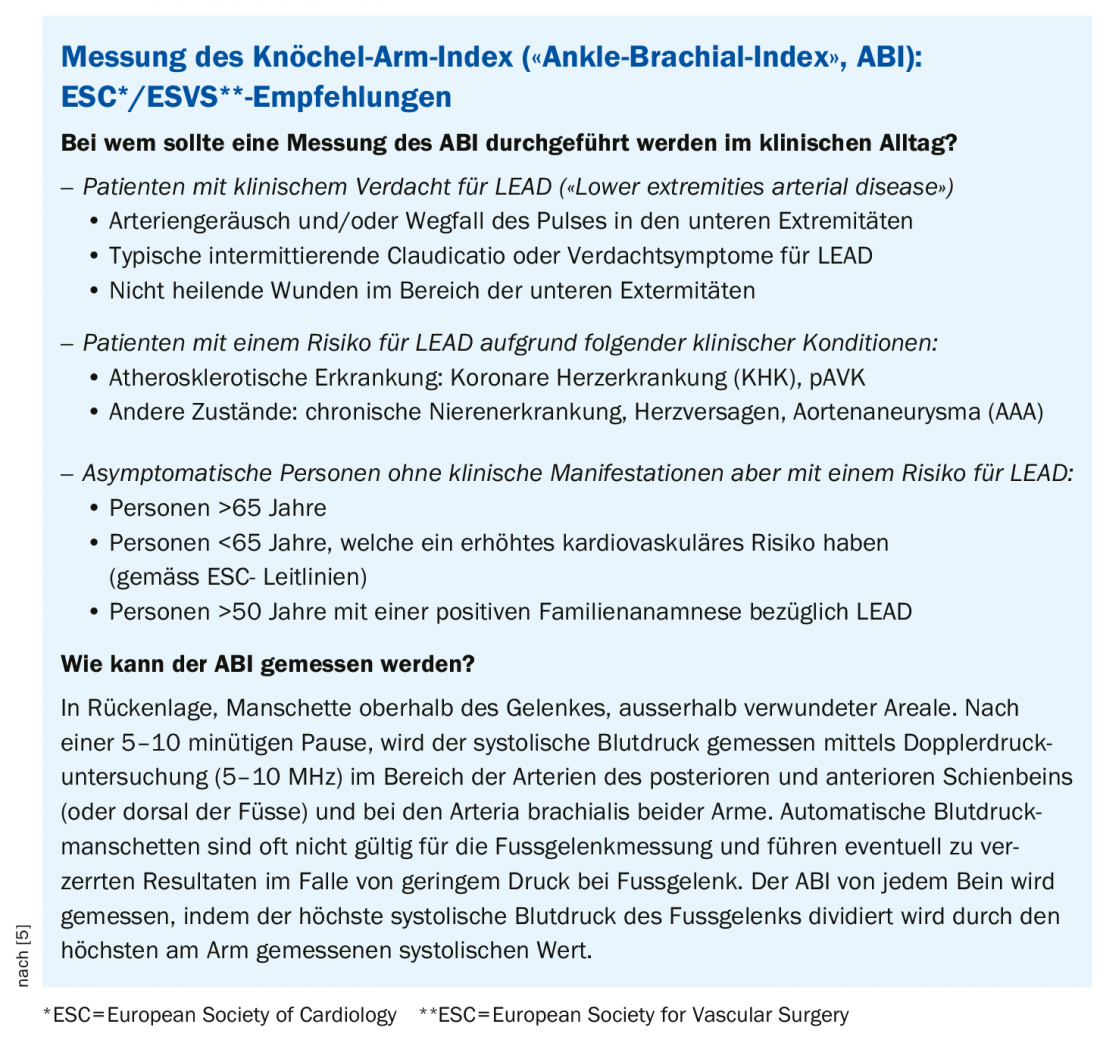
The ankle-brachial index (ABI) can be used as a clinical tool to assess cardiovascular risk and the progression of PAOD (box ). It is a measure that can be obtained by Doppler ultrasonography and blood pressure measurement. The index is a quotient of blood pressure at the lower leg and blood pressure at the upper arm. Routine screening using this method in all patients, including those without cardiovascular risk factors, is not advocated according to current evidence. Statistically, the number of theoretically preventable strokes through routine screening is small in relation to the total population, explained Prof. Martin Storck, MD, Karlsruhe, Germany [1]. A systematic review published in 2015 found that pAVD is common in individuals with multiple cardiovascular risk factors and is associated with morbidity and mortality, but did not suggest that routine screening in the general population was indicated [2]. Prophylactic screening, on the other hand, may be appropriate when cardiovascular coincidences are present (e.g., aneurysm, pAVD), the speaker said. The recommendations for ABI screening according to the 2017 Guidelines for Diagnosis and Therapy in PAD developed by the European Societies of Cardiologists and Vascular Surgeons are summarized in the box.
Smoking is a major risk factor that can be influenced
If history and clinical examination lead to the diagnosis of pAVD, a general cardiovascular risk reduction is crucial in addition to therapy of the arterial circulatory disorder. In this context, conservative therapy and nicotine abstinence are considered important measures. Suitable pharmacological therapies include antiplatelet agents and lipid lowering with statins/ezetimibe [3]. Smoking cessation has been shown to be a very important factor in all phases of vascular disease prevention, which correlates positively with life expectancy, the speaker said (Overview 1).
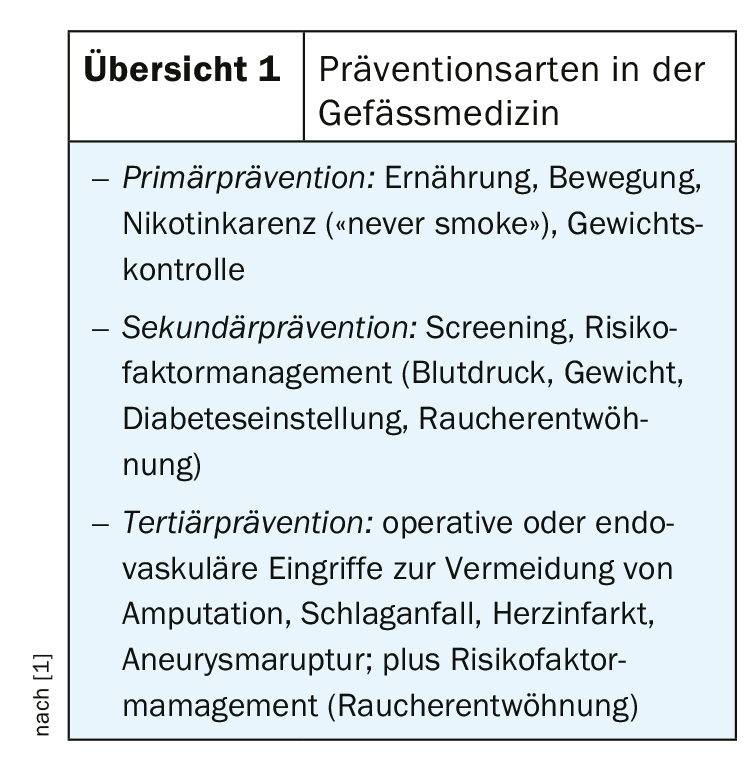
Furthermore, weight control, regular exercise, Mediterranean diet and moderate alcohol consumption have a positive effect on the risk of MACE. Blood pressure control and glucose levels in the normal range are other risk factors that can be influenced. The benefits of lifestyle measures to reduce risk are often underestimated. A longitudinal-design cohort study published in 2019 investigated a possible association of single nucleotide polymorphisms (SNPs), smoking, and diabetes with pAVD and MACE [4]. Annual physical examinations and laboratory analyses were performed over a five-year period in 742 subjects with pAVk and 713 age- and sex-controlled controls. It was found that there were no differences in the distribution of specific SNPs between patients with pAVD and control subjects and between subjects with vs. without MACE. In contrast, diabetes and smoking affected both overall survival probability and MACE-free time. In patients with pAVD, diabetes doubled the hazard ratio for cardiovascular death, and smoking doubled the hazard ratio for death or MACE.
Literature:
- Storck M: Vascular protection. Slide presentation Prof. Dr. med. M. Storck, Karlsruhe (D). Special session, DGIM May 4, 2019.
- Alahdab F, et al: A systematic review for the screening for peripheral arterial disease in asymptomatic patients. J Vasc Surg 2015; 61(3 Suppl): 42S-53S. doi: 10.1016/j.jvs.2014.12.008. epub 2015 Feb 23.
- Paraskevas KI, et al: Definition of Best Medical Treatment in Asymptomatic and Symptomatic Carotid Artery Stenosis. Angiology 2016; 67(5): 411-419.
- Boc V, et al: Diabetes and smoking are more important for prognosis of patients with peripheral arterial disease than some genetic polymorphisms. Vasa 2019; 48(3): 229-235.
- Aboyans V, et al: 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS), https://academic.oup.com/eurheartj/article/39/9/763/4095038
HAUSARZT PRAXIS 2019; 14(12): 32-33