Tenosynovial giant cell tumor is a rare benign disease of the synovium in which there is marked tissue proliferation. Diffuse joint destruction with subsequent disability may result. The future may belong to therapy with tyrosine kinase inhibitors.
Tenosynovial giant cell tumor (TGCT) is a rare benign tumor of the extremities arising from the synovium of the joints, bursae, or tendon sheaths. A distinction is made between the localized form, which is often located extraarticularly and is usually found in the tendon sheaths of the hand and foot, and the diffuse growing form, which affects larger joints and grows intraarticularly. While the former forms are generally considered benign, the diffuse forms are much more aggressive and may show signs of malignancy in rare cases. Approximately 1.8 new cases per 100,000 population occur annually. Most patients develop the disease between the ages of 20 and 40 .
Great clinical diversity
Clinically, there are usually nonspecific symptoms. Therefore, there is a risk of both under- and over-therapy. A slow-growing mass is often found, leading to swelling with correspondingly taut skin. In intra-articular forms, effusions, reduced range of motion, and blockages with pseudomeniscal symptoms occur. Especially in young adults with soft tissue swelling in the hands or larger joints, TGCT should be considered if symptoms in a single joint with slow progression make other synovial causes, such as polyarthritis or gout, unlikely.
The causes lie in an overexpression of CFS1 (colony-stimulating factor 1) with an activation of the corresponding receptor. However, translocation and concomitant overexpression of the ligand is found in only a small fraction of cells. Predominantly, the cells within the tumors consist of non-neoplastic cells that show strong expression of the CSF1 receptor.
Diagnostics by means of imaging
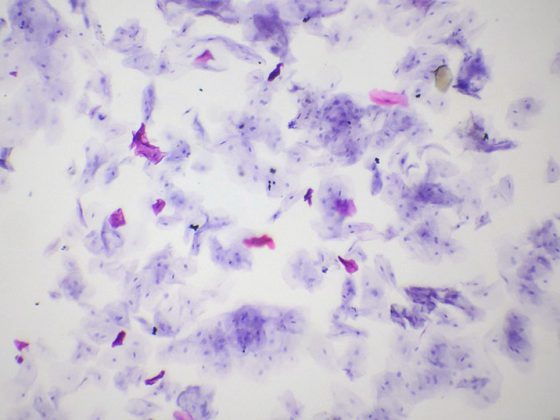
Radiography and MRI with contrast are indicated to rule out frequent bony involvement. In early stages, often only indirect signs of swelling or joint effusion can be detected. In advanced stages, cystic loss of substance may develop on the adjacent bone, typically stringing together like pearls. However, only a fine tissue examination after biopsy is conclusive.
Therapeutically no agony of choice
In the localized form, surgical intervention is the therapy of choice. Usually, macroscopic resection is sufficient and also associated with recurrence in only a few patients. In the diffuse form, however, the recurrence rate is approximately 50%. TGCT rarely has a clear demarcation, which means that a definition of the boundary to healthy tissue cannot always be clearly made. The possibility of radiotherapy is controversial. Retrospective studies showed good disease control with doses of 30-50 Gy. However, given the mostly benign nature of the disease and the often young patient age, it is rarely used.
Future: drug treatment?
A new era of treatment could be ushered in with the administration of tyrosine kinase inhibitors. According to case reports and prospective studies, complete remissions can be achieved for the first time with the causal mechanism-based therapy regimen. In it, disease controls of over 90% are reported.
Data from a Phase I study show objective remission rates of 52%. On this basis, the first conducted randomized trial of drug therapy in TGCT was set up. 120 patients were randomized. In terms of tumor volume shrinkage, a remission rate of 56% vs. no remission was achieved with placebo. However, tumor regrowth is observed in many patients after discontinuation of therapy. Currently, several compounds are being developed that specifically inhibit the CSF1R axis. How the development will continue remains to be seen.
Further reading:
- Myers BW, Masi AT: Pigmented villonodular synovitis and tenosynovitis: A clinical epidemiologic study of 166 cases and literature review. Medicine (Baltimore) 1980; 59: 223-238.
- Byers PD, et al: The diagnosis and treatment of pigmented villonodular synovitis. J Bone Joint Surg Br 1968; 50: 290-305.
- Gounder MM, et al: Locally aggressive connective tissue tumors. J Clin Oncol 2018; 36: 202-209.
- Cannarile MA, et al: Colony-stimulating facor 1 receptor (CSF1) inhibitors in cancer therapy. J Immunother Cancer 2017; 5: 53.
InFo ONCOLOGY & HEMATOLOGY 2019; 7(6): 20