Primary angiitis of the central nervous system (PACNS) is one of the orphan diseases and affects the large and small vessels of the central nervous system. Misdiagnosis of this heterogeneous disease is the rule. Biomarkers should pave the way to effective therapy.
PACNS is characterized by a transmural inflammatory response with damage to the vessel walls. The heterogeneity of inflammatory vasculopathy is the reason why the disease is often not recognized. Clinical symptoms range from persistent headache to encephalopathy with cognitive and affective abnormalities to multifocal symptoms with recurrent ischemia. Also, the distinction from important differential noninflammatory vascular diseases of the brain (eg. B. Reversible cerebral vasoconstriction syndrome [RCVS], Moyamoya disease [MMD]) is difficult. State-of-the-art diagnostics are based on the visualization of structural changes in the vessels, whereas modern studies focus on the visualization of the inflammatory response as a possible marker for different subtypes of the disease with differences in course, treatment response and outcome. Therefore, intensive research was conducted into biomarkers that could support diagnostics.
One study looked at circulating endothelial cells (CSCs), which have been described as markers of endothelial damage. Because they were significantly more abundant in the active stage of small vessel vasculitis compared with patients in remission, they are considered an important biomarker for systemic vasculitis. Now, CEC levels were studied in patients with active PACNS compared to healthy controls, patients in remission, and patients with RCVS and MMD. Indeed, significantly higher CEC levels were also detected in patients with active PACNS. Accordingly, they can serve as diagnostic biomarkers. Also, CECs may be useful in delineating important differential diagnoses because they describe the extent of endothelial damage-with higher values in inflammatory and lower values in noninflammatory vasculopathies.
Exclude patients with strokes of non-inflammatory etiology using IL-17.
Another study determined the potential of the cytokine IL-17 as a biomarker, especially in differentiating it from patients with strokes of noninflammatory origin. Here, a small case series has already shown that IL-17 differentiates the two patient groups. Cytokine production of expanded T helper cells from CSF was determined in 39 patients by intracellular staining followed by FACS analysis. Of these, four patients had strokes due to primary CNS vasculitis, five patients due to secondary CNS vasculitis, and 30 patients had strokes of noninflammatory origin. Statistical significance was determined by t-test. Significantly more IL-17-producing T helper cells were found in the CSF of patients with primary or secondary CNS vasculitis. Elevated IL-17 indicated secondary or primary CNS vasculitis with a sensitivity of 80% (CI 45-93) and specificity of 94% (CI 78-98).
Specific inflammatory patterns for confirming the diagnosis
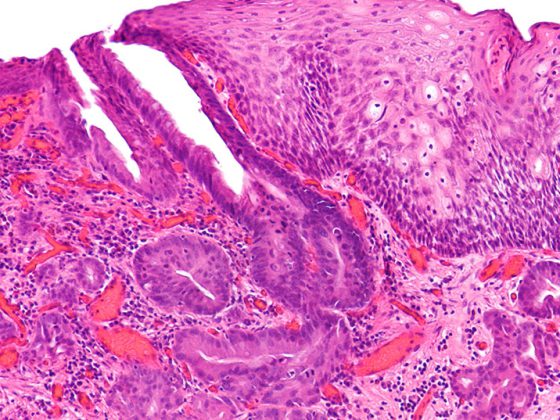
In order to establish new diagnostic methods by means of innovative techniques, the question was raised whether there are PACNS-specific inflammatory patterns that allow an unambiguous diagnosis and allow conclusions to be drawn about different subtypes as well as their clinical courses and response to therapy. For this purpose, all existing studies were examined in a meta-analysis and, in addition, a retrospective flow cytometric analysis of 18 PACNS patients was performed. A total of 28 cohort studies involving 635 patients were identified. There were differences in clinical symptoms, CSF findings, and imaging findings between angiographically and bioptically confirmed cases. These results suggest that angiographically or biopsy confirmed PACNS are distinct subtypes. Retrospective analysis of flow cytometric findings from 18 PACNS patients revealed differences in immune cell composition. This also suggests different subtypes of the disease, which should be detected more precisely in the future.
Source: 92nd Congress of the German Society of Neurology (DGN)
InFo NEUROLOGY & PSYCHIATRY 2019; 17(6): 30 (published 11/24/19, ahead of print).