Peripheral vascular injuries, although rare, present significant challenges. In addition to hemorrhage control, limb preservation is the primary concern.
Peripheral vascular injuries are relatively rare in our latitudes and account for <1% of all trauma procedures. For sharp injuries, the focus is on hemorrhage control. Blunt vascular trauma is often accompanied by concomitant injuries, making it easy to miss the presence of peripheral ischemia. However, timely recognition and treatment of ischemia is critical for survival and limb preservation. Open surgery using vascular surgical principles remains the mainstay in the treatment of peripheral vascular injuries. Endovascular procedures are also becoming increasingly important in this area and are a very good alternative in selected cases.
Epidemiology
Data from the US National Trauma Data Bank from 2002 to 2006 show that peripheral vascular injury is present in 0.64% of all trauma procedures [1]. In 2/3 of the cases the upper extremity is affected, in 1/3 the lower extremity. 4 of 5 patients are male; mean age is 36 years. Vascular injuries of the upper extremity were more frequently due to sharp trauma (62.6%), whereas vascular injuries of the lower extremity were more frequently due to blunt trauma (56.2%). The four most common causes of trauma are traffic accidents, followed by gunshot and stab wounds and falls from heights.
The rate of major amputations is 1.3% for upper extremity vascular injuries. At the lower extremity, this is significantly higher at 7.8%. Mortality also shows a striking difference. While vascular injuries in the upper extremity have a mortality of 2.2%, this is 7.7% in the lower extremity. Patients >65 years are twice as likely to die compared with the younger collective; however, the amputation rate is the same in both groups [2].
In a Swedish registry study from 1987 to 2005, 50% of all peripheral vascular injuries were iatrogenic [3]. Data from England seem to confirm the assumption that in our circles especially iatrogenic trauma is mainly responsible for peripheral vascular injuries [4]. Patients with iatrogenic vascular injuries are older and have more comorbidities. Accordingly, the peri- and postoperative risk also increases.
Diagnostics/procedure
Sharp trauma may be associated with acute life-threatening bleeding. Here, bleeding control is the top priority. If safe hemostasis cannot be achieved by compression bandaging or manual compression, a tourniquet should be applied if anatomically possible. Experience from the Iraq and Afghanistan wars shows that tourniquet placement clearly saves lives without causing relevant damage in cases of severe limb hemorrhage (<2% nerve lesions with 2 hours of permanent tourniquet placement) [5].
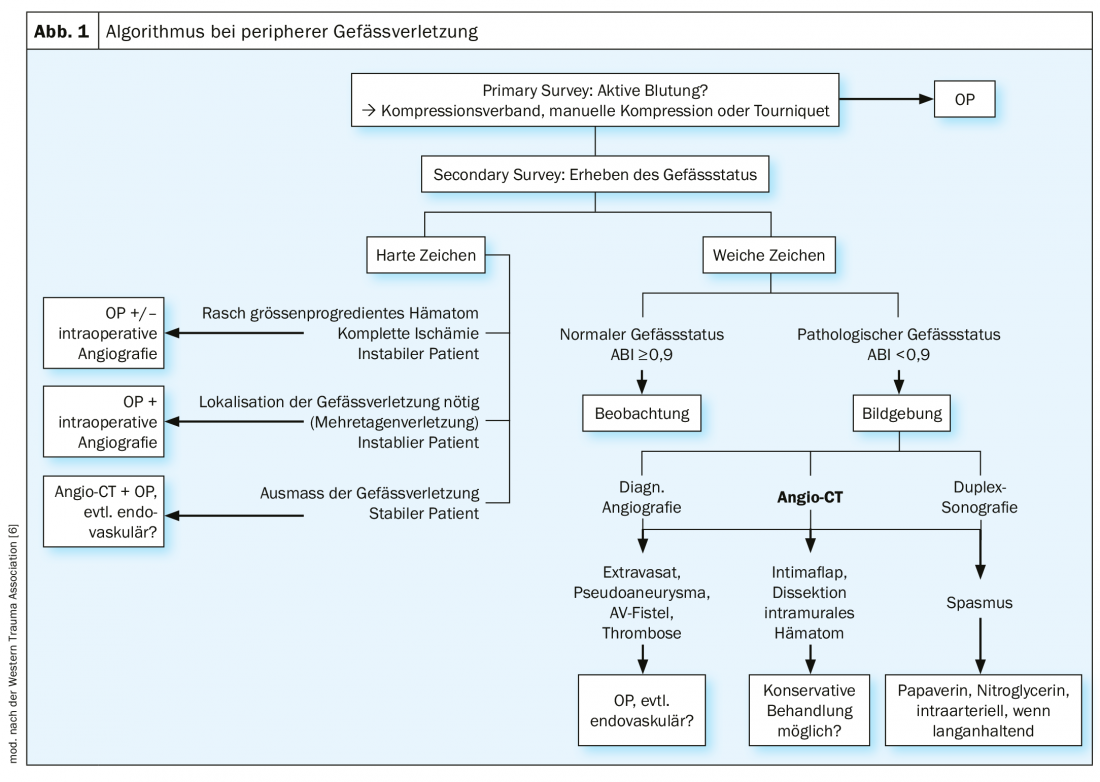
Blunt vascular trauma often results from traffic accidents or falls. The initial focus here is on the treatment of life-threatening concomitant injuries. One is guided by the ATLS scheme. A clean vessel status must be obtained in the Secondary Survey. Absence of palpable pulses, especially in young patients without circulatory shock or hypothermia, must raise suspicion. It is also helpful in the emergency setting to determine an ABI index, as this can be objectified. For values <0.9, further clarification should be carried out generously. The most important thing to think about is possible vascular injury. In the clinical examination, a distinction is made between hard and soft signs that are indicative of vascular injury. Hard signs include obvious hemorrhage, a rapidly size-progressive hematoma, a flow murmur or buzz over the injured vessel, and signs of acute ischemia (pulselessness, pallor, pain, sensory disturbances, motor deficit, shock). Soft signs include finding blood at the scene, wounds in the extremity with unclear hemorrhagic shock, existing peripheral nerve damage, high-risk fractures or dislocations (e.g., injury to the popliteal artery in knee dislocation), and trauma near an extremity artery [6].
In the trauma setting, contrast-enhanced computed tomography is imaging of 1st choice. This is almost ubiquitous, readily available, and reliably maps relevant concomitant injuries in addition to the vascular injury. Alternatively, duplex sonography or diagnostic angiography may be performed. The latter, although invasive, offers the possibility of direct therapeutic intervention, depending on the case.
If bleeding is obvious, the patient can be taken to the operating room without further diagnostics and detours, especially if the patient is hemodynamically unstable. The same is true for complete limb ischemia, depending on the case. There is then the possibility of intraoperative angiography. Figure 1 shows a possible algorithm in the procedure for peripheral vascular injury.
Sharp vascular injuries
Sharp vascular injuries damage the vessel from the outside in. Three degrees of severity are distinguished. Grade I involves extraluminal vascular injury (limited to the adventitia +/-media) and does not result in hemorrhage or ischemia. An intramural hematoma may result. Secondary rupture or aneurysm formation may occur due to wall weakness. A grade II injury opens the lumen and accordingly causes bleeding. The formation of a pseudoaneurysm or an AV fistula with additional vein penetration is also possible. The grade III injury completely severed the vessel, leading to hemorrhage and peripheral ischemia. In smaller arteries, hemorrhage may spontaneously arrest by retraction and curling of the intima [7].
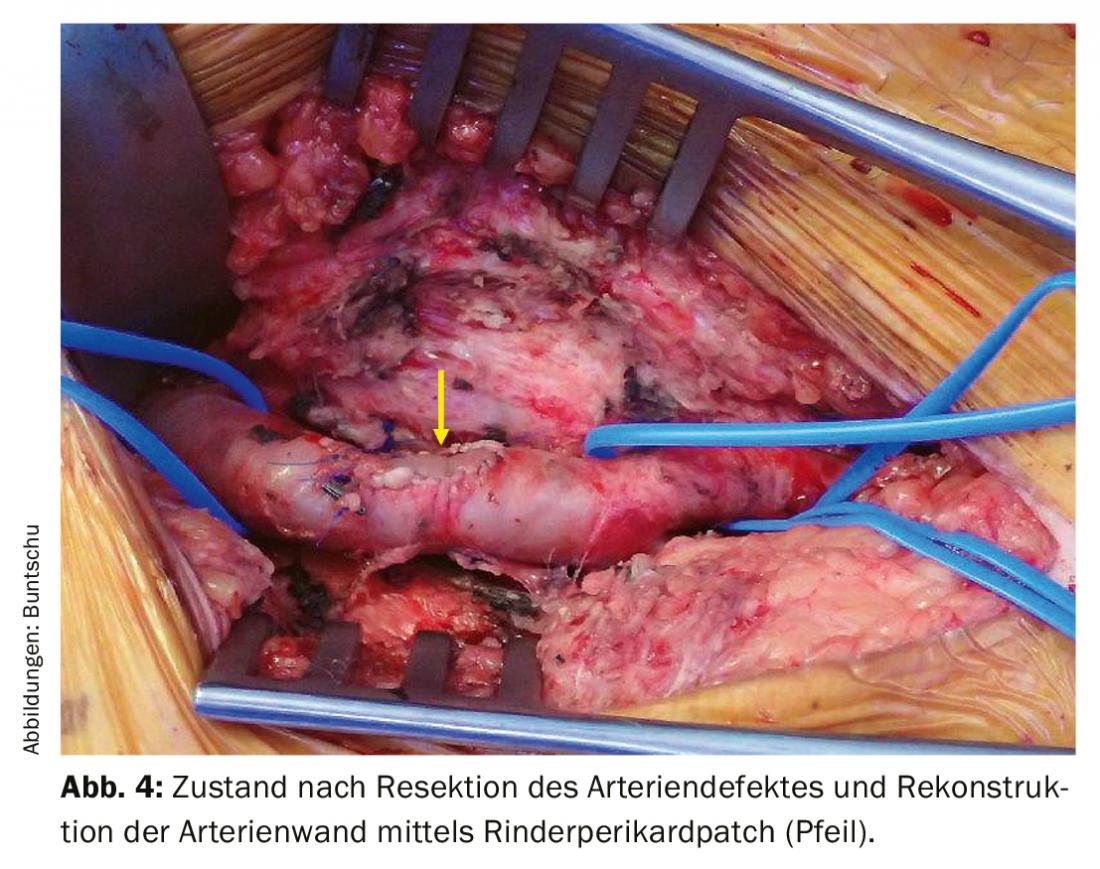
Transverse arterial injuries can usually be sutured directly. Injuries in the longitudinal direction of the vessel should be closed with a patch (autologous vein or bovine pericardium) (risk of iatrogenic stenosis with direct suture). In the case of larger arterial defects, such as those present in gunshot wounds, the affected arterial segment must be resected until the arterial wall is intact again. If tension-free is possible, a direct end-to-end anastomosis can be performed. If the artery diameter is <8 mm, the ends should be beveled. If a tension-free suture is not possible, an interposition device must be sewn in. Priority is given to the great saphenous vein because it has the best long-term openness rates and is resistant to infection [8].
Since the surgical site is usually contaminated by the penetrating trauma, plastic prostheses (PTFE, Dacron) should only be used in the absence of autologous vein material or if the diameter mismatch is too large. Alternatively, biosynthetic grafts are also available.
Blunt vascular injuries
Blunt vascular injuries damage the vessel from the inside out [7]. Analogous to the sharp injury, three degrees of severity are distinguished. Grade I represents an intimal flap, which is usually asymptomatic and can be treated conservatively provided it attaches to the vessel in the direction of flow. If it lifts off in the direction of flow, there is a risk of dissection. In this case, open or endovascular treatment should be discussed depending on the location. Grade II means a tear of the intima and media, often resulting in thrombotic occlusion of the artery. In a grade III injury, the entire arterial wall is destroyed and the artery is held together only by a fine adventitial fringe. Grade II and III injuries both entail peripheral ischemia. A special form of blunt vascular trauma is the abrupt overstretching of an artery, such as occurs in knee dislocation. This can result in a tear of the intimal tube with consecutive arterial occlusion. Surgical treatment of long-stretch occlusions is performed by bypass or interposition. The great saphenous vein is again the graft material of choice.
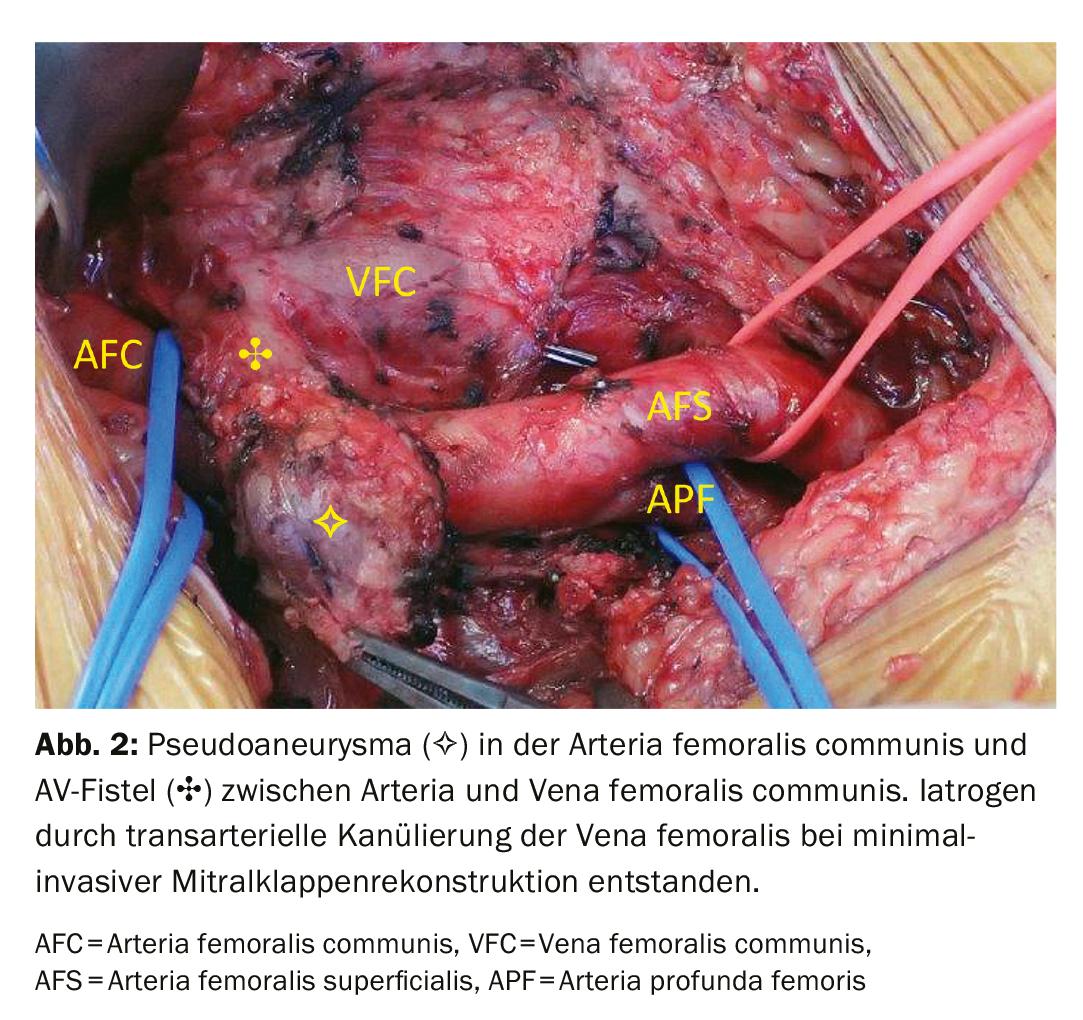
Vascular injuries of the lower extremity
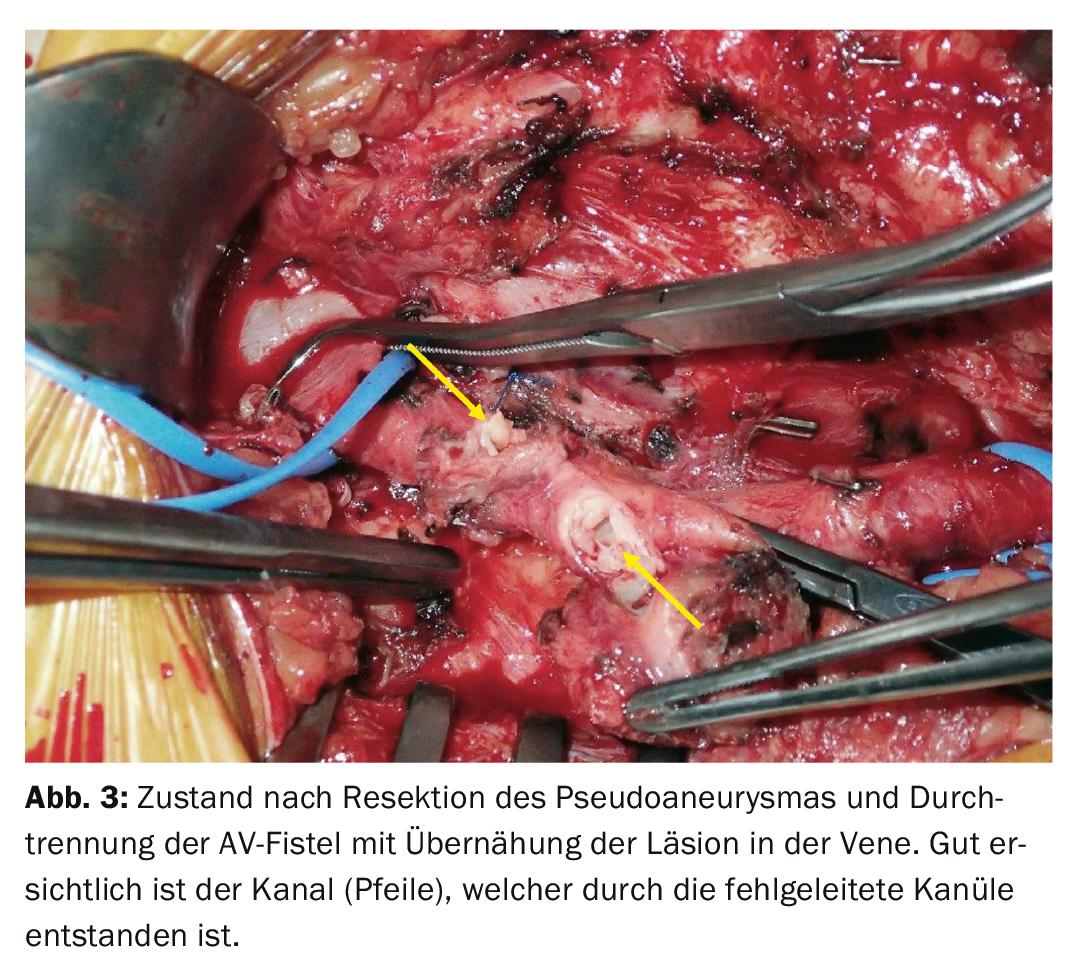
The femoral artery is by far the most commonly affected by injury in our culture. Iatrogenic trauma is frighteningly common at 50-70%. Pseudoaneurysms often form, and occasionally AV fistulas are seen (Figs. 2-4) . Pseudoaneurysms can be closed either by manual compression or thrombin injection, depending on the size and aneurysm neck. If unsuccessful, endovascular elimination using a stent graft or open repair using direct suturing can be performed. AV fistulas can be well treated endovascularly with a stent graft, depending on the location. If the anatomy is unfavorable, only open treatment can be considered here as well. Knife or gunshot injuries to the groin region are treated with open surgery. For inflow control, the external iliac artery can be visualized and clamped via a small suprainguinal approach. Reconstruction of the profunda femoris artery is of particular importance in the groin, as its collateral system may be crucial for distal leg perfusion. Especially in young patients, the superficial femoral artery should of course also be reconstructed optimally.
The common femoral vein should be reconstructed whenever possible to ensure venous outflow from the leg [9]. Depending on the defect, a direct suture or the insertion of a vein patch may be used. Only rarely does an interposition device have to be sewn in. The superficial femoral vein or profundal femoral vein can be ligated if they cannot be reconstructed via a simple suture. But one of them should be open. Additional nerve injury is present in approximately 20% of cases.
The popliteal artery is the second most commonly affected by injury. The cause in >70% of cases is blunt trauma, especially knee joint dislocation. After reduction, rapid restoration of blood circulation is the top priority. For this purpose, an interposition or bypass is created with the ipsi- or contralateral saphenous vein removed. A final angiogram confirms the success of the operation. Sharp injuries in the popliteal fossa are rare. Inflow control can be performed here by means of an Esmarch cuff applied to the thigh. In this way, any additional venous bleeding can also be better controlled. Analogous to the common femoral vein, the popliteal vein should also be reconstructed if possible. However, the openness rate is much worse than in the common femoral vein, so complex reconstructions are rather out of the question [9]. Injuries to the arteries of the lower leg are associated with fractures in the vast majority of cases. A single injured tibial artery can be ligated if the other two are open to distal on the intraoperative angiogram [10]. Lower leg arteries are reconstructed either by suturing a venous patch or by creating a popliteo-crural venous bypass.
Vascular injuries of the upper extremity
Injuries to the subclavian and axillary arteries are rare but are associated with high mortality and are difficult to treat surgically because of the protective bony wall. Depending on the trauma mechanism, severe thoracic trauma may also be present. Clavicle fracture with fracture of the 1st and 2nd ribs and consecutive hematopneumothorax are then not uncommon. Adequate access to the subclavian artery is gained through a long incision that continues from the sternoclavicular joint across the medial half of the clavicle laterally into the Mohrenheim fossa. The medial half of the clavicle is detached and resected from the attachments of the sternocleidomastoid muscle, pectoralis major muscle, and subclavius muscle. Alternatively, the clavicle can be luxated cranially from the sternoclavicular joint. Proximal injuries to the subclavian artery may require additional sternotomy or thoracotomy. The vascular injury is treated according to the principles already described. The subclavian/axillary vein should be reconstructed if simply possible. Special attention must be paid to brachial plexus injuries. The clavicle is osteosynthetically reconstructed at the end of surgery [11].
Endovascular stent grafting for active hemorrhage, pseudoaneurysm or AV fistula formation is a superior alternative in the subclavian artery [12]. However, the anatomical conditions must be right. The vertebral artery and internal thoracic artery (especially if mammary bypass is present) should be preserved whenever possible. In the arm, the brachial artery is most commonly affected by injury. Again, iatrogenic injuries are on the rise. Supracondylar humerus fractures or elbow dislocations may result in intimal avulsion with subsequent vascular occlusion. For the reconstruction of longer-stretch occlusions, only a vein interposition device can be considered.
Injury to a single forearm artery does not necessarily require reconstruction if the hand supply via the noninjured artery is adequate. An intraoperative angiogram can provide information in case of doubt. Since the ulnar artery often supplies the hand, it is more important in reconstruction than the radial artery. Analogous to the transtibial arteries, an injury should be treated with a patch. Bypass facilities are rare.
Outcome
The duration of ischemia largely determines the neuromuscular outcome of the limb. After five hours of ischemia time, the risk for irreversible damage increases continuously. If there is also relevant blood loss, ischemia tolerance is again drastically shortened. As little as three hours of ischemia time can lead to a much worse neuromuscular outcome in this situation. With the duration of ischemia, the reperfusion damage after restoration of blood circulation also increases. The associated tissue swelling can eventually lead to compartment syndrome. Missed compartment syndrome is associated with a threefold increase in mortality and a twofold increase in amputation rate, which is why the threshold for prophylactic fasciotomy should be kept low. An ischemia time >4 hours, ligation of a guiding vein, hemorrhagic shock with mass transfusion, and combined arterio-venous injury are independent risk factors for the development of compartment syndrome [13].
Deciding when a limb can no longer be saved and should be primarily amputated presents every surgeon with a dilemma. Decision support should be provided by the Mangled Extremity Severity Score (MESS), which takes into account the associated tissue damage, degree of ischemia, degree of shock, and age of the patient and assigns different scores depending on the extent. In the original 1990 publication, a MESS ≥7 points was reported with a 100% probability of amputation [14]. Today, 30 years later, this score does not appear to be entirely accurate, as even a MESS = 8 can be associated with 60% limb preservation [15]. However, little is reported about the functionality of the preserved limb. Ultimately, it should be a team decision between the traumatologist/orthopedist, vascular surgeon, and plastic surgeon as to when a limb cannot be primarily saved.
Even secondary to initially successful vascular reconstruction, major amputation may be unavoidable. Prognostically significant factors for this include associated soft tissue damage, postoperative compartment syndrome, ischemia time >6 hours, arterial multilevel injury, blunt trauma mechanism, and patient age >55 years. Shock and additional nerve or vein injury are not factors [16].
An injured vessel does not have to be reconstructed immediately in every case. If the patient is hemodynamically unstable and the vascular injury requires extensive reconstruction, an intravascular shunt can be temporarily inserted in the sense of “damage control”. After appropriate circulatory stabilization, reconstruction is secondary. Other shunt indications may include urgent surgical repair of concomitant injuries, simultaneous injury to multiple vascular systems in the body, or evaluation of limb preservation for prolonged ischemia [17].
Take-Home Messages
- Peripheral vascular injuries are rare and more and more often iatrogenic in our country
- Blunt vascular trauma is associated with a higher risk of concomitant injuries and associated tissue damage, and the amputation rate is higher
- The threshold for prophylactic fasciotomy after prolonged limb ischemia should be kept low
- The great saphenous vein is the most important graft in the treatment of peripheral vascular injuries
- Endovascular stent implantation is a good alternative to surgery in selected cases
Literature:
- Tan T-W, et al: Limb outcome and mortality in lower and upper extremity arterial injury: a comparison using the National Trauma Data Bank. Vasc Endovascular Surg. 2011; 45 (7): 592-597.
- Barmparas G, et al: Pediatric vs adult vascular trauma: a National Trauma Databank review. J Pediatr Surg. 2010; 45: 1404-1412.
- Rudstrom H, et al: Iatrogenic vascular injuries in Sweden. A nationwide study 1987-2005. Eur J Vasc Endovasc Surg. 2008; 35: 131-138.
- De’Ath HD, Galland RB: Iatrogenic and non-iatrogenic vascular trauma in a district general hospital: a 21-year review. World J Surg. 2010; 34(10): 2363-2367.
- Kragh JF Jr, et al: Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009; 249: 1-7.
- Feliciano DV, et al: Evaluation and management of peripheral vascular injury. Part 1. Western Trauma Association/critical decisions in trauma. J Trauma. 2011; 70(6): 1551-1556.
- Vollmar J: Reconstructive surgery of the arteries. 4th ed. Thieme.1996: 70-95.
- Feliciano DV: Pitfalls in the management of peripheral vascular injuries. Trauma Surg Acute Care Open. 2017; 2: 1-8.
- Kuralay E, et al: A quantitative approach to lower extremity vein repair. J Vasc Surg. 2002; 36(6): 1213-1218.
- Burkhardt GE, et al: Outcomes of selective tibial artery repair following combat-related extremity injury. J Vasc Surg. 2010; 52(1): 91-96.
- Demetriades D, et al: Penetrating Injuries to the Subclavian and Axillary Vessels. J Am Coll Surg. 1999; 188(3): 290-295.
- DuBose JJ, et al: Endovascular management of axillo-subclavian arterial injury: a review of published experience. Injury. 2012; 43(11): 1785-1792.
- Ritenour AE, et al: Complications after fasciotomy revision and delayed compartment release in combat patients. J Trauma. 2008; 64: S153-S162.
- Johansen K, et al: Objective Criteria Accurately Predict Amputation following lower extremity trauma. J Trauma. 1990; 30(5): 568-572.
- Loja MN, et al: The Mangled Extremity Score and amputation: time for a revision. J Trauma Acute Care Surg. 2017; 82(3): 518-523.
- Perkins ZB, et al: Meta-analysis of prognostic factors for amputation following surgical repair of lower extremity vascular trauma. Br J Surg. 2015; 102(5): 436-450.
- Gifford SM, et al: Effect of temporary shunting on extremity vascular injury: an outcome analysis from the Global War on Terror vascular injury initiative. J Vasc Surg. 2009; 50: 549-555.
CARDIOVASC 2019; 18(6): 6-10