40-year-old patient sees gastroenterologist with heartburn and fluid regurgitation. The otherwise healthy patient suffers increasingly from the discomfort.
Background: A 40-year-old patient came to the gastroenterologist with increasing heartburn and fluid regurgitation. The symptoms occurred in each case after sumptuous meals and during travel stress. The otherwise healthy patient was previously untreated.
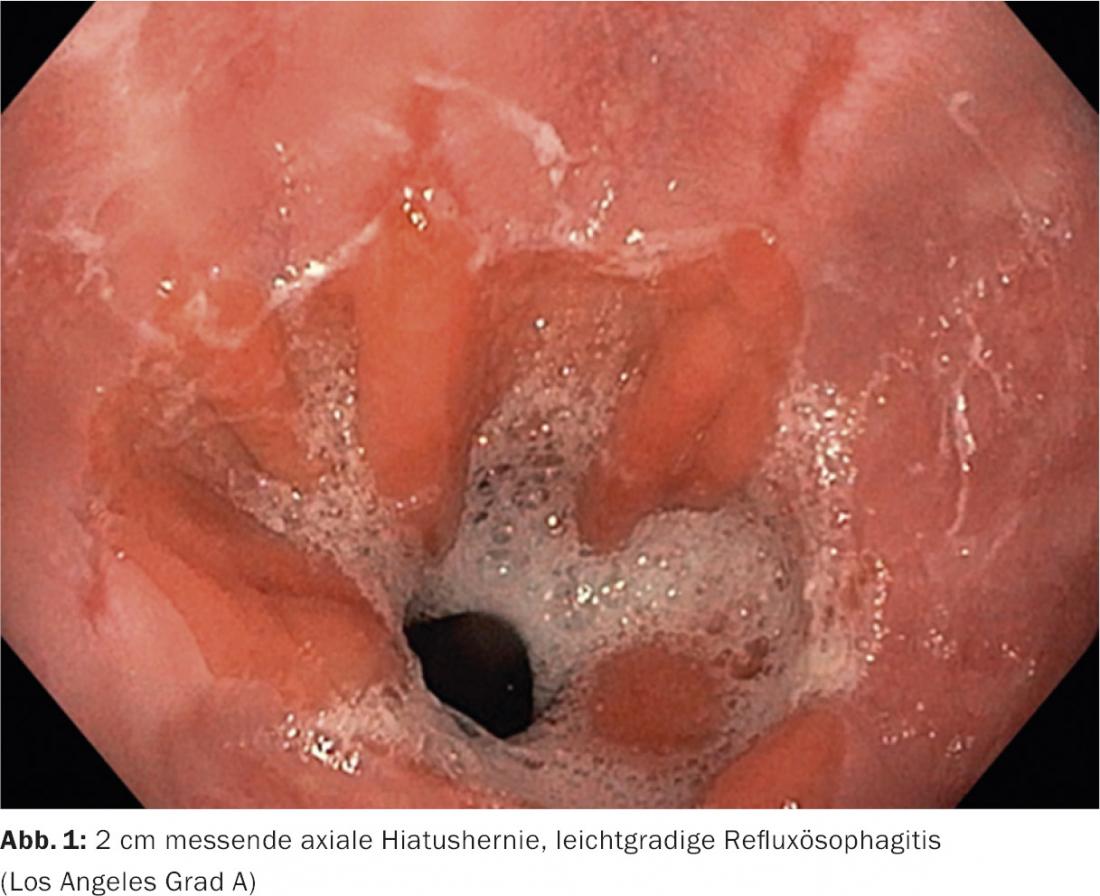
History and Diagnosis: Further history revealed that the patient had a risk factor for reflux with a BMI of 30, but was otherwise not taking any medications and had no additional comorbidities. An endoscopy was performed for further clarification of the complaints. Mild reflux esophagitis (Los-Angeles classification of grade A), with a small axial hiatal hernia could be diagnosed.
Therapy/Progress: The patient was prescribed combination therapy with a proton pump inhibitor and alginate (40mg esomeprazole plus alginate, once daily). Under this treatment, the patient was symptom-free after four weeks. Subsequently, the patient stopped taking the proton pump inhibitor and has not taken any proton pump inhibitors since. Instead, treatment is with alginate as needed, to which the patient responds well subjectively.
 Comment by Marcel Halama, MD: The present case demonstrates mild reflux esophagitis that was favored by the two risk factors of axial hiatal hernia and obesity. For patients with mild reflux esophagitis, after initial therapy with proton pump inhibitors, as-needed use of alginate offers a good treatment option.
Comment by Marcel Halama, MD: The present case demonstrates mild reflux esophagitis that was favored by the two risk factors of axial hiatal hernia and obesity. For patients with mild reflux esophagitis, after initial therapy with proton pump inhibitors, as-needed use of alginate offers a good treatment option.