The benefit of lung cancer screening in defined risk groups has been demonstrated in two large studies. In the early stages of the disease, limited resection with lymphadenectomy is the therapy of choice.
Primary bronchial carcinoma is one of the most common malignancies worldwide. In Switzerland, it is the second most common malignancy in men with an incidence of 11.9%. In women, the incidence is 8.7%, making it the third most common tumor. At 21.9%, bronchial carcinoma has the highest tumor-associated mortality in men and, at 15.4%, the second highest in women after breast carcinoma [1].
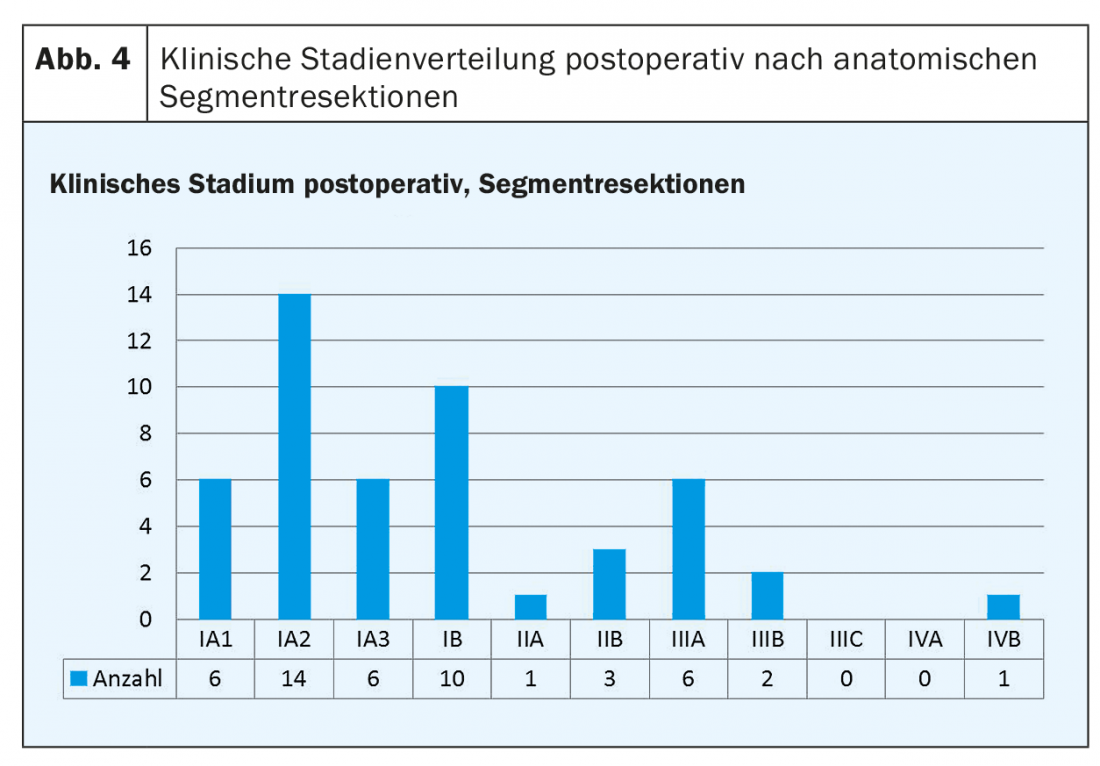
The longer-term prognosis depends on the clinical stage of the tumor disease at the time of diagnosis. Accordingly, the 5-year survival rate is 80-90% in stage IA1-IA3, 73% in stage IB, 65% in IIA, 56% in IIB, 41% in IIIA, 24% in IIIB, and 12% in IIIC. Based on these survival data, the recommendations for the eighth edition of the TNM classification for NSCLC with the corresponding changes in clinical stages were published in the same study [2].
Early detection in NSCLC – recent results of new studies.
The fact of a relatively good prognosis at an early stage of the disease and the fact that bronchial carcinoma is one of the leading malignancies in women and men have led to several international studies on bronchial carcinoma screening in recent years.
The largest study, the National Lung Screening Trial (NLST) from North America, published in 2011, randomized 53 454 patients at defined risk. One group received “low-dose” computed tomography (LDCT) for three consecutive years, while the other group received only conventional chest X-ray. In the LDCT group, the primary endpoint of a 20% reduction in lung cancer mortality was met and the study was terminated. How much lung cancer mortality would have been reduced if the study had continued is unknown. Overall mortality was reduced by 6.7%. The Number Needed to Screen was 320 patients at risk to prevent death [3].
The largest randomized trial in Europe and second largest worldwide is the Dutch-Belgian “Lung Cancer Screening Trial” (NELSON), which started in 2003. The full data are expected in December 2018, but the main content was presented in September 2018 at the “World Conference on Lung Cancer” in Toronto [4,5]. Current smokers or former smokers with ten years or less of abstinence, more than 15 cigarettes/day over 25 years, or more than ten cigarettes/day over 30 years were included. The study concluded that 50% of carcinomas were diagnosed at an early stage, 65-70% at stage IA-II. 70% of the carcinomas in the control group were stage III-IV. All-cause mortality was reduced by 26% over a 10-year period in high-risk male patients and by as much as 61% in women.
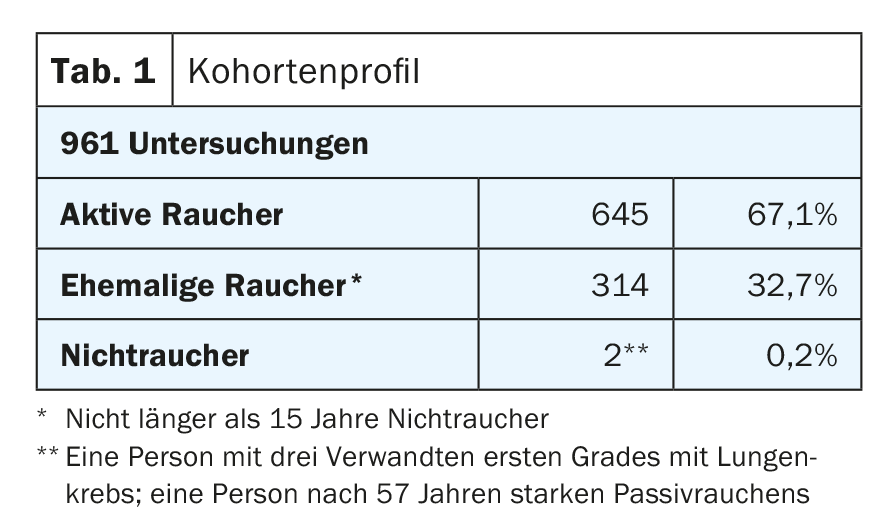
Between January 2016 and November 2018, current data from the Foundation for Pulmonary Diagnostics are available in this country: 961 examinations were performed. The distribution of the risk groups can be found in table 1. Among those examined, five bronchial carcinomas were newly diagnosed, two in stage IA and one person each in stage IIA, IIIA and IV. 102 persons underwent tobacco cessation.
Data on limited (sublobar) resections for NSCLC.
The results of the screening studies are also noteworthy with respect to surgical treatment options. The NELSON trial demonstrated that 65-70% of carcinomas correspond to stage IA-II [4]. What do these results mean in terms of surgical therapy?
In recent years, intensive research has been conducted to determine whether a limited resection in the sense of a segmentectomy or an extra-anatomic resection (wedge) represents a reasonable alternative to the classic lobectomy – both oncosurgically and in general. The intention for performing a segmentectomy is to preserve as much healthy lung tissue as possible, which is especially beneficial in patients with limited pulmonary reserve.
The data on segmental resection initially seem controversial. Various studies from the period 1990 to about 2012 show a clear advantage in terms of overall as well as recurrence-free survival in favor of lobectomy in all surgically treatable stages, especially in stages I and II [6,7]. Wolf et al. however, showed that in segmentectomies with mediastinal lymphadenectomy, the rate of local recurrence and recurrence-free survival were identical. This was remarkable and prompted more detailed studies focusing on respecting segmental anatomy and systematic lymphadenectomy [8]. The development of minimally invasive surgical technique toward true anatomic segment resection (not simply wedge resection) was crucial. This automatically respects the anatomically predetermined lymphatic drainage and radical surgical removal despite limited parenchyma-sparing resection [9].
Altorki et al. 2014 and Tsutani et al. 2013 showed equal ten-year survival rates in stage IA and 3-year recurrence-free survival in adenocarcinoma. Similarly, the retrospective survey by Kodama et al. 2016 (312 patients with clinical stage cT1 N0 M0) no increased rate of local recurrence or differences in overall survival in the segmental resection group [10–12].
The positive impact on postoperative lung function after limited resection has been demonstrated in some studies [13,14].
Importance of mediastinal lymphadenectomy.
As mentioned above, the impact of consistent and sufficient mediastinal lymphadenectomy in terms of recurrence-free survival is an important consideration. Ludwig et al. and Gulack et al. showed that increasing numbers of resected lymph nodes are associated with a survival benefit [15,16].
Also examined was the work of Stiles et al. The impact of lymphadenectomy in stage IA NSCLC. A clear advantage in terms of long-term survival as well as recurrence-free survival was shown for sublobar resection with lymphadenectomy compared with sublobar resection without lymphadenectomy [17].
Impact of this development in the daily routine of thoracic surgery.
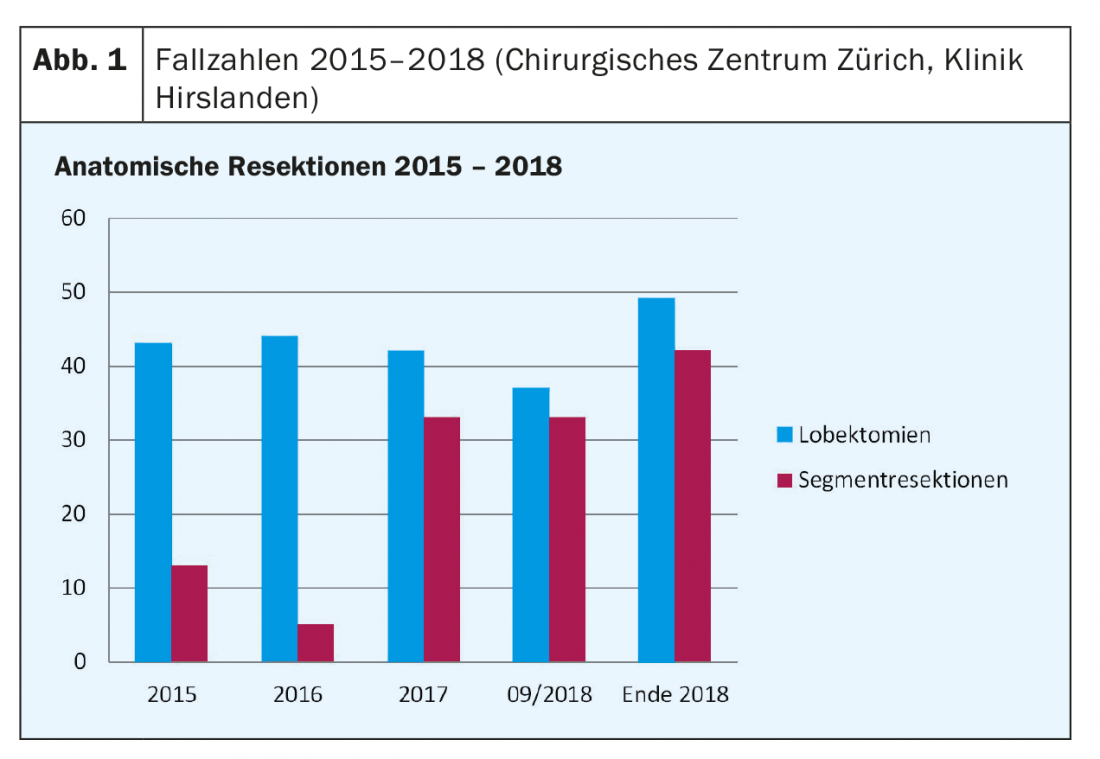
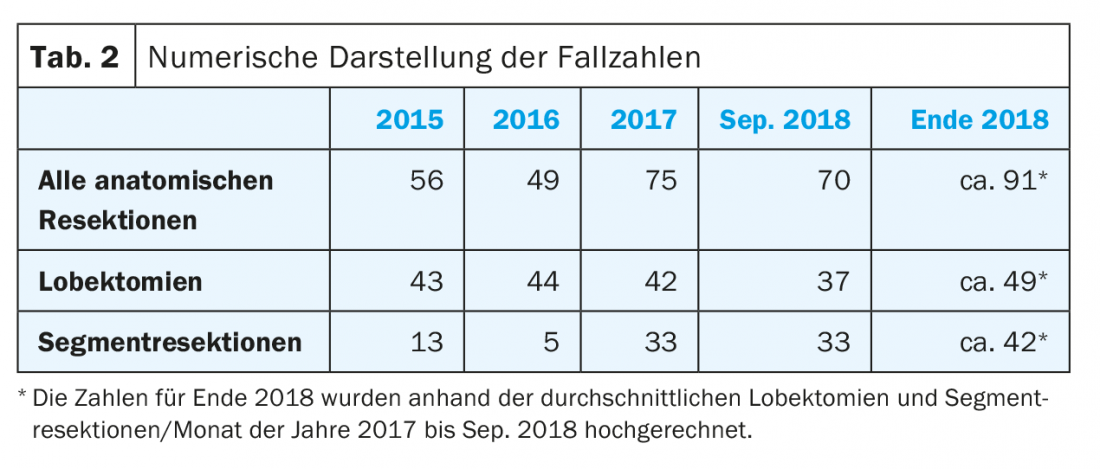
At the Surgical Center Zurich of the Hirslanden Clinic, we are indeed seeing a steady increase in the proportion of anatomical segment resections. In addition, there has been an overall increase in the number of all anatomic resections since the beginning of 2015 (Fig. 1 and Table 2).
Results of the last period in detail
Between January 2016 and September 2018, 194 anatomic resections were performed at our institution, of which 123 (63%) were lobectomies. The number of anatomical segment resections was 71 patients (37%), up from 13 patients (23%) in 2015, and already increased to 33 patients (44%) in 2017. Approximately 42 patients (46%) are expected at the end of 2018.
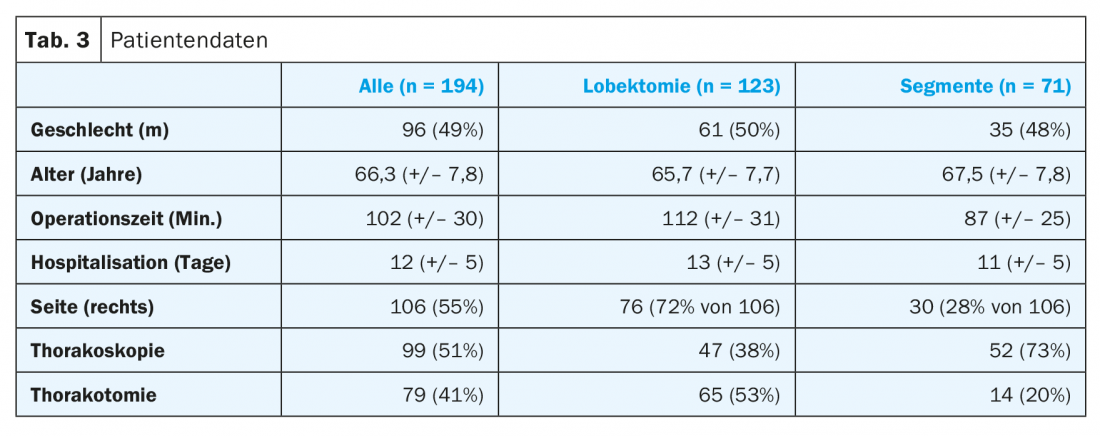
Surgical time was a mean of 25 minutes longer for lobectomies at 112 minutes (+/- 31) than for segmental resections at 87 minutes (+/- 25). Hospitalization duration tended to be two days longer for lobectomies, at 13 days (+/- 5). More than 70% of segmental resection surgeries were performed thoracoscopically, with nearly half of lobectomies performed minimally invasively (Table 3).
In almost three quarters of all patients, the postoperative diagnosis was non-small cell lung cancer (Fig. 2).
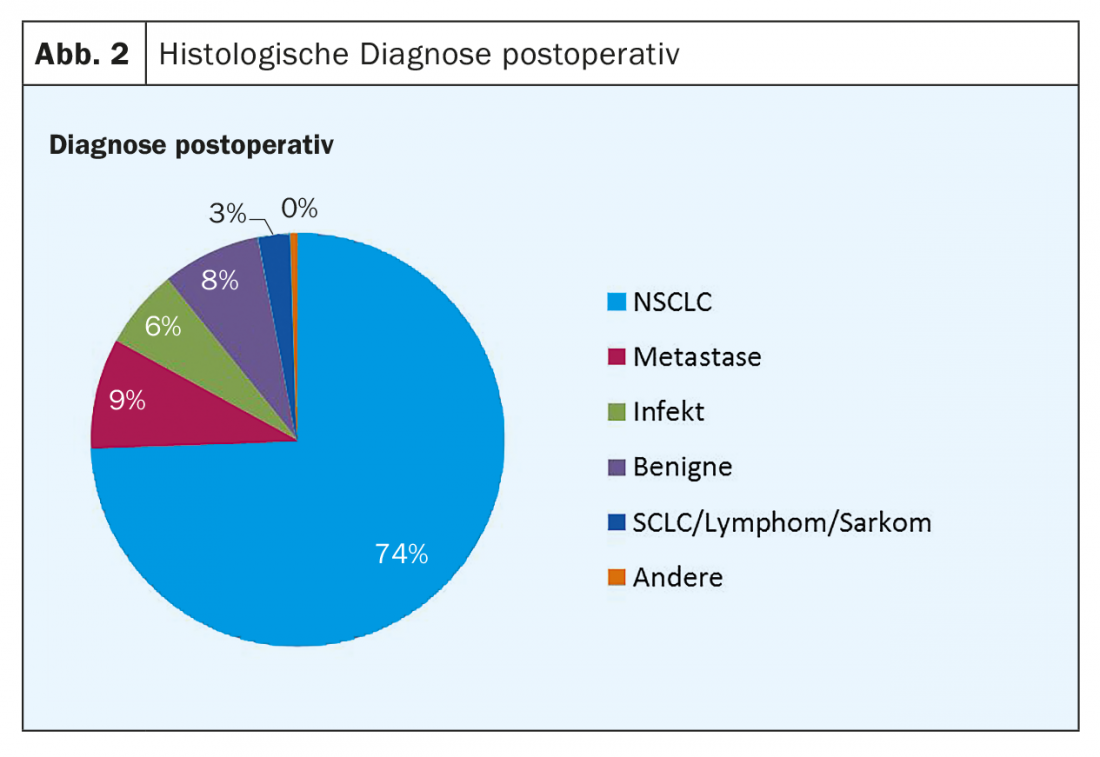
Among lobectomies, NSCLC accounted for 94 patients (76%), followed by benign or infectious findings at 14% and metastases at 6%. For segmental resections, the proportion of NSCLC was 50 patients (70%), as well as 15% for benign and infectious findings and 14% metastases.

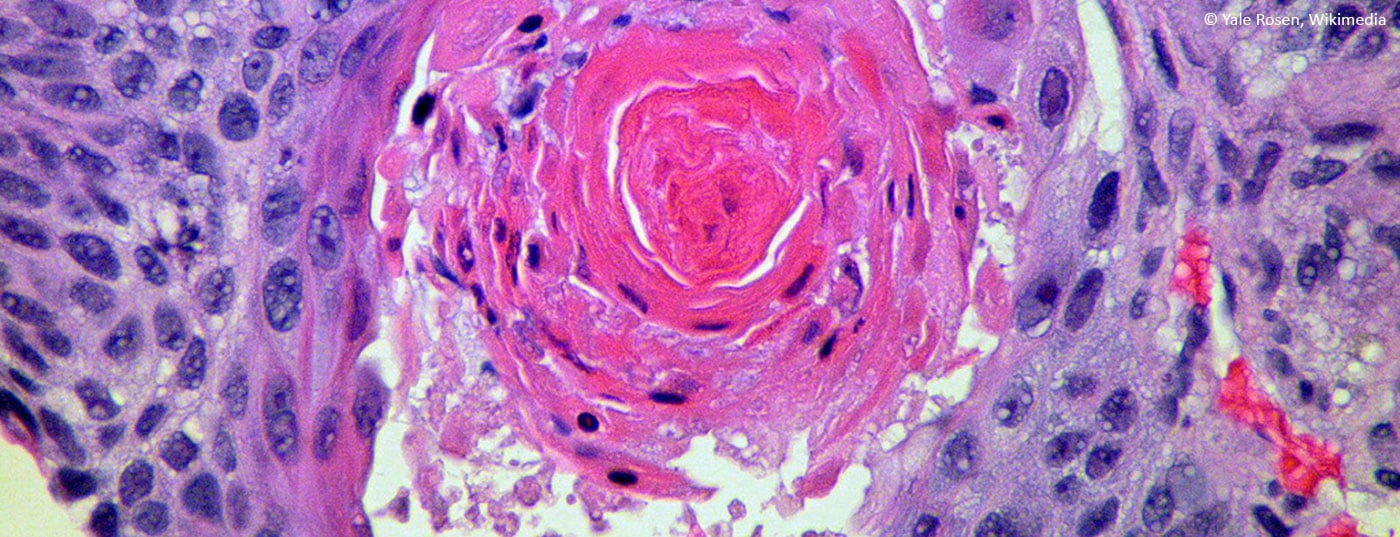
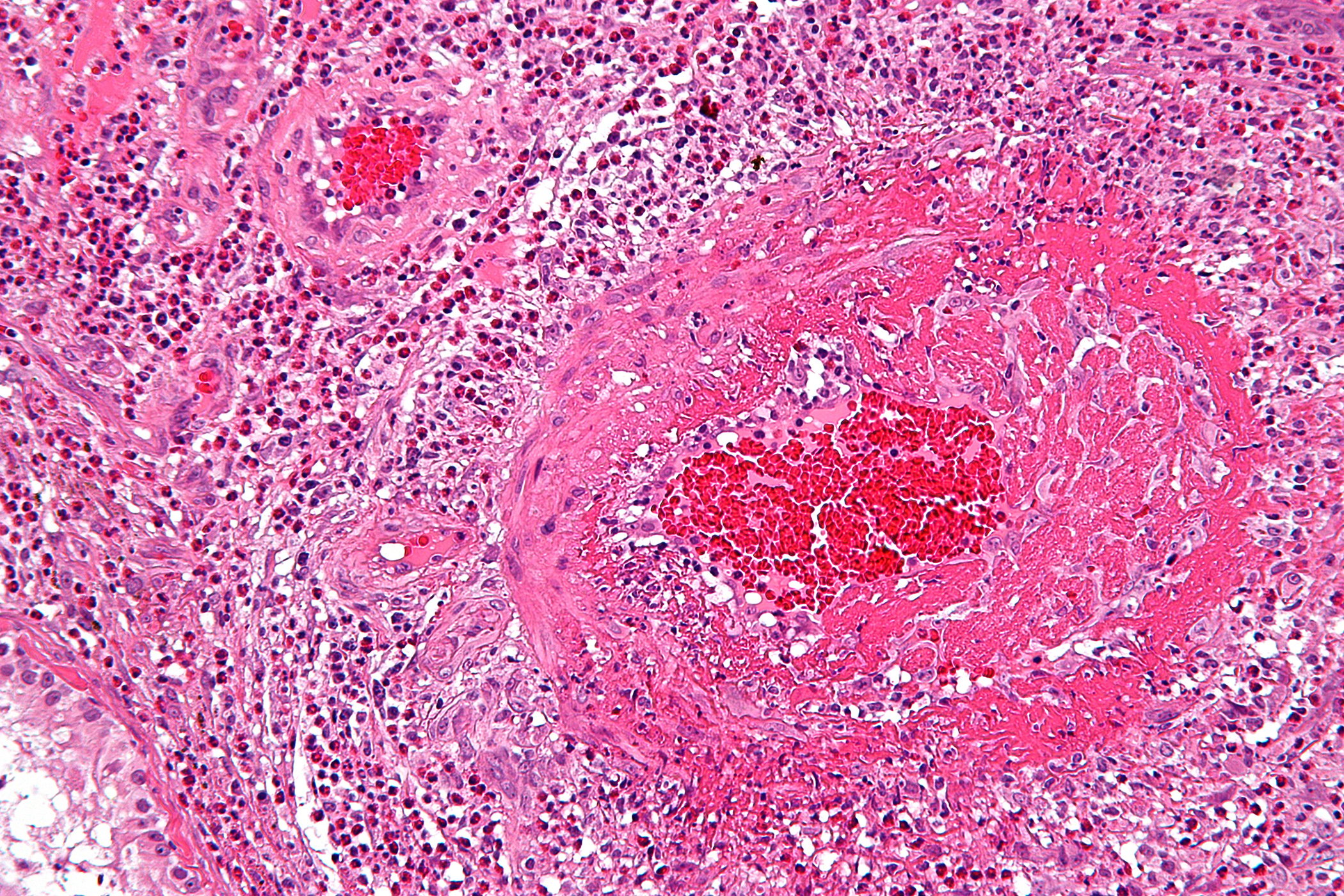
Histologically, 66% of NSCLC were adenocarcinoma type, 23% squamous cell carcinoma, 7% carcinoid, 3% pleomorphic carcinoma, and 1% large cell carcinoma (Fig. 2).
Figures 3 and 4 show, respectively, the distribution of postoperative clinical stages in lobectomies (Fig. 3) and segmental resections (Fig. 4).
Morbidity and mortality
The 30-day mortality of all anatomic resections (n=194) was three deaths (1.5%).
Overall morbidity was 9.5%, with no difference noted in either group. The most common complication was persistent air leak (defined >7 days), followed by pneumonia, postoperative empyema, cardiac complications such as atrial fibrillation, and postoperative hematoma/postoperative hemorrhage.
Discussion
The trend toward modern, increasingly lung-sparing, oncologic resections has been clear at our institution since 2015. This shows that an increasingly tailored approach is being applied not only in the drug treatment of lung cancer, but also in surgery. There was no change in terms of morbidity and mortality. However, the proportion of minimally invasive surgeries is increasing and the length of hospital stays is trending shorter.
Of great importance is the correct technical execution of a segmental resection (along the anatomical structures) in order to ultimately proceed oncosurgically radical despite limited resection. Only in this way will recurrence-free survival be as good as in the past, when lobectomy was the gold standard. Interestingly, 80% of segmental resections performed in our institution showed postoperative stage I-IIB. In the remaining ten patients, a majority of cases showed an occult N2 situation. It is precisely these “understagings”, some of which have already been detected intraoperatively, that will always enliven the discussion as to whether the trend can prevail. Dyas et al. were able to show in 2018, based on a prospective study of 1444 patients, that despite computed tomography of the thorax, PET-CT and other investigations, an occult N2 situation was present in 10% of patients with NSCLC classified as stage I and 21% of patients classified as stage II [18]. The positive impact of lymphadenectomy on recurrence-free survival has been demonstrated in several studies [15–17]. Based on these data, all of our patients with NSCLC undergo radical mediastinal lymphadenectomy. Intraoperative rapid diagnosis, also at the lymph node stations, is of utmost importance and is a very important source of information to set the right course from the beginning, especially in limited resections.
Take-Home Messages
- Two major international studies demonstrate the benefit of lung cancer screening in defined risk groups.
- Therapy of choice in the early stages is limited resection (anatomic segment resection) with lymphadenectomy, preferably minimally invasive or robot-assisted.
Literature:
- Krebsliga: Cancer in Switzerland: important figures. 2016.
- Goldstraw P, et al: The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 2016 Jan; 11(1): 39-51.
- Aberle DR, et al: Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 2011; 365: 395-409.
- De Koning H, et al: Effects of volume CT lung cancer screening: mortality results of the NELSON randomized-controlled population based trial. World Conference on Lung Cancer 2018; Abstract PL02.05.
- Zhao YR, et al: NELSON lung cancer screening study. Cancer Imaging 2011; 11(1A): S79-S84.
- Lung cancer study group: Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. The Annals of Thoracic surgery 1995; 60(3): 615-623.
- Whitson A, et al: Survival After Lobectomy Versus Segmentectomy for Stage I Non-Small Cell Lung Cancer: A Population-Based Analysis. The Annals of Thoracic surgery 2011; 92(6): 1943-1950.
- Wolf AS, et al: Lobectomy Versus Sublobar Resection for Small (2 cm or Less) Non-Small Cell Lung Cancers. The Annals of Thoracic surgery 2011; 92(5): 1819-1825.
- Koike T, et al: Risk factor analysis of locoregional recurrence after sublobar resection in patients with clinical stage IA non-small cell lung cancer. The Journal of Thoracic and cardiovascular surgery 2013; 146 (2): 372-378.
- Altorki NK, et al: Sublobar resection is equivalent to lobectomy for clinical stage 1A lung cancer in solid nodules. The Journal of Thoracic and cardiovascular surgery 2014; 147(2): 754-764.
- Tsutani Y, et al. Oncologic outcomes of segmentectomy compared with lobectomy for clinical stage IA lung adenocarcinoma: Propensity score-matched analysis in a multicenter study. The Journal of Thoracic and cardiovascular surgery 2013; 146(2): 358-364.
- Kodama K, et al: Oncologic Outcomes of Segmentectomy Versus Lobectomy for Clinical T1a N0 M0 Non-Small Cell Lung Cancer. The Annals of Thoracic surgery 2016; 101(2): 504-511.
- Macke RA, et al: Parenchymal preserving anatomic resections result in less pulmonary function loss in patients with Stage I non-small cell lung cancer. J Cardiothorac Surg 2015; 10: 49.
- Saito H, et al: Pulmonary Function After Lobectomy Versus Segmentectomy in Patients with Stage I Non-Small Cell Lung Cancer. World Journal of Surgery August 2014; 38(8): 2025-2031.
- Ludwig MS, et al: Postoperative survival and the number of lymph nodes sampled during resection of node-negative non-small cell lung cancer. Chest 2005; 128(3): 1545-1550.
- Gulack BC, et al: The Impact of Tumor Size on the Association of the Extent of Lymph Node Resection and Survival in Clinical Stage I Non-Small Cell Lung Cancer. Lung Cancer 2015; 90(3): 554-560.
- Stiles BM, et al: The importance of lymph node dissection accompanying wedge resection for clinical stage IA lung cancer. Eur J Cardiothorac Surg 2017; 51(3): 511-517.
- Dyas AR, et al: Clinical Misstagings and Risk Factors of Occult Nodal Disease in Non-Small Cell Lung Cancer. The Annals of Thoracic surgery 2018; 106(5): 1492-1498.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(6): 4-7.