Adverse drug reactions are divided into type A and type B reactions. Type A reactions are based on the mechanism of action of the drug. Type B reactions (drug allergies) are less common but potentially dangerous and are caused by an immune response to the drug.
Drug allergies (MA) usually occur unpredictably. The manifestations are clinically very variable and potentially dangerous. The underlying mechanisms are heterogeneous and finding the cause is difficult. Recent data have shown that immune stimulation in MA is triggered by three distinct mechanisms that differ in speed of manifestation, dose dependence, clarification options, and genetics [3]. Attribution of a response is complicated by the fact that many patients receive multiple medications simultaneously. If MA is suspected, a careful workup is required. If it is a MA, the affected patient should be adequately informed about his or her condition. An allergy passport from the SGAI (Swiss Society of Allergology and Immunology) is recommended; it contains information on the severity of the allergy, tolerated alternative medications, and background on allergy diagnosis. The allergy passport is available from the Allergy Center Switzerland (www.aha.ch).
“Adverse Drug Reaction.
Adverse drug reactions (ADRs) are divided into type A and type B reactions [1,2]. Type A reactions are common (85%) and are due to pharmacological reactions (e.g., fatigue after high-dose anti-H1 blockers, erosive gastritis after NSAID, etc). Type B reactions (about 15%) are those hypersensitivity reactions whose symptoms do not correspond to the mechanism of action of the drug, but are caused by immune reactions: an exanthema after amoxicillin has nothing to do with the mechanism of action of the antibiotic, but is caused by an immune reaction to amoxicillin.
Hypersensitivity reactions: Type B reaction
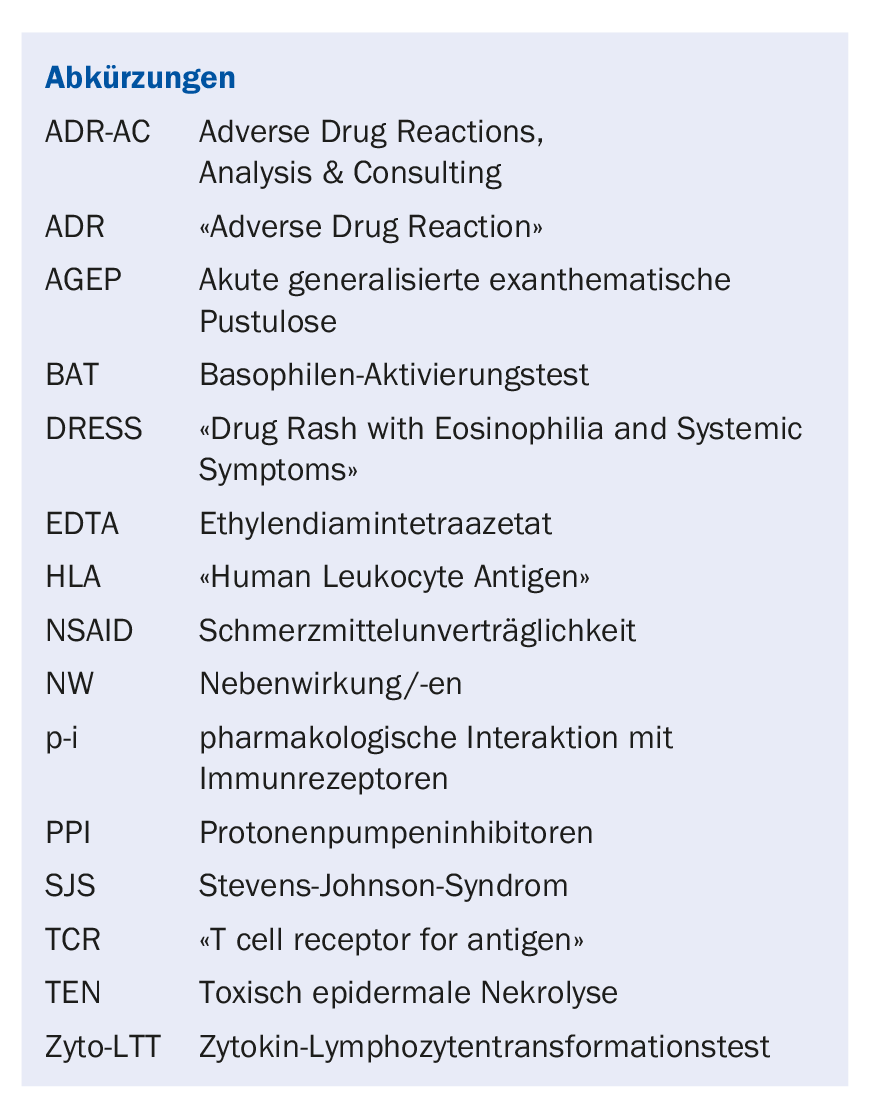
Formation of a new antigen/allergen (hapten model): A chemically reactive drug (e.g. penicillin) binds to a protein by means of covalent bonding (hapten mechanism): the hapten-protein complex is recognized as a new antigen by the immune system, against which a complex immune reaction develops based on different B- or T-cell simulations. Clinically, depending on the type of immunostimulation, there are different symptoms such as rapid onset anaphylaxis (IgE-mediated), eczema and exanthema (both T-cell-mediated) manifesting only after days, or hemolysis (IgG/IgM). This immune-allergic reaction follows the principles of immune stimulation to proteins and can be detected by skin tests and in vitro tests. The number of drugs that clearly stimulate via the hapten mechanism is manageable. Some drugs become reactive drugs (e.g. sulfanilamides) only after metabolization (Table 1).
p-i (pharmacological interaction with immune receptors): This concept, developed in the drug allergy research group at Inselspital, combines pharmacology with immunology [4]. Drugs have a tendency to attach to proteins via hydrogen bonding, electrostatic interactions, and van der Waals forces, as is the case with normal ligand-receptor interactions. In part, these non-covalent interactions lead to blockade or stimulation of receptors important for activation of T cells. In the p-i mechanism, these “pharmacological” interactions involve the immune receptors HLA and TCR. In contrast to the hapten model, only selective stimulation of T cells occurs in p-i. There are a number of drugs that stimulate mainly via the p-i mechanism, and these responses are often clinically problematic (hepatitis, DRESS, SJS/TEN) (Table 1).
In the drugs abacavir, carbamazepine, or allopurinol, relative affinity binding occurs primarily or exclusively to specific HLA alleles: e.g., the major metabolite of allopurinol (oxypurinol) can bind strongly to the allele HLA-B*58:01, abacavir to B*57:01, and carbamazepine to B*15:01 or A*31:01. Individuals who have these HLA alleles are particularly susceptible to severe NW such as SJS or DRESS: HLA typing can be used to capture the risk of severe NW, which is often done for abacavir and carbamazepine in people from Southeast Asia because HLA-B*15:02 is relatively common in this region. Alternatively, the drug may bind directly to the TCR, which recognizes peptides in the HLA: this is the case, for example, in allergies to sulfamethoxazole, where different binding sites on the TCR have been identified [4]. Diagnosis is based on the detection of T-cell responses in skin or in vitro assays (cyto-LTT).
Pseudoallergic side effects: These are due to direct stimulation of the effector cells of the immune system. The best studied is the stimulation of mast cells via the MRGPRX2 receptor by binding quinolones or muscle relaxants [5]. It explains the occurrence of urticaria and anaphylaxis under these drugs. Most important are the pseudoallergic reactions to NSAID, and part of these NW can be attributed to increased leukotriene production [6]. Activation of eosinophils and basophils occurs, as well as mast cell stimulation. Symptoms include rhinosinusitis and bronchospasm in the sense of aspirin-sensitive asthma, and/or urticaria and anaphylaxis. Pseudoallergic NW are common. Since there is no involvement of the specific immune system (B and T cells), immune tests (skin tests, BAT, cyto-LTT) are negative (Tab. 1) . The diagnosis is based on provocation tests as well as anamnesis and follow-up regarding the question which drugs are tolerated or trigger symptoms.
Immediate type or late type reactions?
The following questions are important for the clinician: Could it be a drug allergy? Distinction between immediate and late type reactions? Danger signals? Which drug is the trigger? Often, MA is not thought of until late in the differential diagnosis because the clinical manifestations of MA mimic various other viral or bacterial immune or autoimmune diseases. In cases of unexplained disease, MA should always be included in the differential diagnosis. Indications of MA as a symptom cause are: Association with a newly prescribed drug (since <1-45 days) or typical symptoms of an itchy rash (exanthema), urticaria, anaphylaxis or eosinophilia.
It is important to distinguish immediate-type from late-type reactions. Reactions that occur within an hour of drug administration (sometimes peracute, within minutes) are either IgE- or pseudoallergic-mediated. They manifest as flash, pruritus (typically palmar, plantar, scalp, axillary, genital), urticaria and, if internal organs are also affected, additionally as anaphylaxis (bronchospasm, vomiting, diarrhea, hypotension, cardiogenic shock). Most reactions do not occur until after six hours (usually after four days). With amoxicillin, the most common trigger of MA in Switzerland (2-8% of those treated), exanthema often occurs after a treatment period of 7-12 days, sometimes only after discontinuation of the drug. Exanthema is clinically relatively heterogeneous and usually due to drug-stimulated T cells.
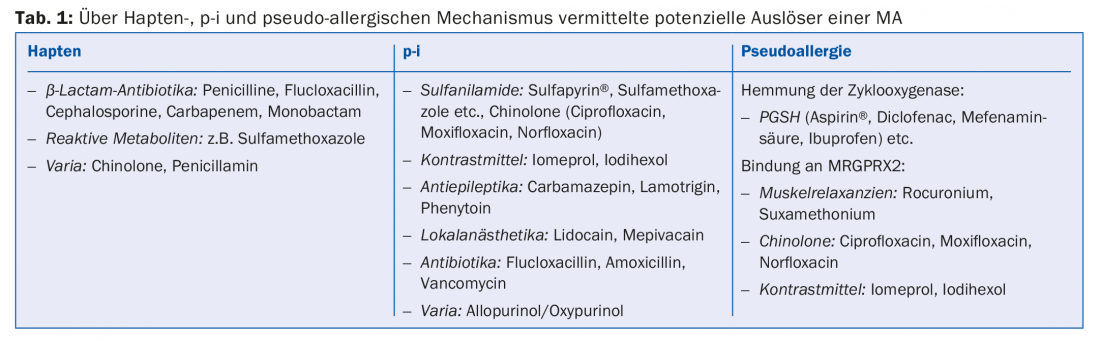
Late type reactions are dominated by macular, urticarial and maculopapular exanthema. Mild to moderate hepatitis is not uncommon, and pleurisy, pancreatitis, etc. are rare. Bullous skin reactions and mucosal reactions (conjunctivitis, oral or genital ulcers/aphtae), which characterize SJS/TEN and have a lethality of 10-30%, must always be classified as dangerous. Typical and thus indicative are massive elevations of eosinophilia (often >1 G/l) and lymphoblasts (as in Epstein-Barr virus infection), which are often ignored: If MA is suspected, always obtain a differential blood count or look for lymphoblasts and, in the case of generalized exanthema, always determine liver values (SGOT/SGPT, LDH, AP, γGT) to detect liver involvement; informed of danger signs. Table 2. Rarely, hematologic NW (thrombocytopenia, hemolytic anemia, agranulocytosis) may occur. These are largely mediated by IgG.
Which drug is the trigger?
Identifying triggers of MA is very complex. Documentation of medication as accurately as possible with regard to duration, dose, and the time of the first symptoms of MA are central to the clarification; in particular, whether and what type of MA are known with the corresponding medications. Sometimes this already succeeds in demarcation and assignment. Because many patients are on combination therapy, the history is often difficult and inconclusive. The diagnosis of a drug allergy should be made with as low a probability of error as possible, since associated consequences can include withholding an important group of drugs and increasing the cost/worse treatment.
Skin and in vitro tests: In in vivo clarification, concentrations, solubility, availability of sterile drugs as well as simultaneous ingestion of drugs during testing and much more must be taken into account, so that clarification is carried out by an allergist. Also to be considered are the possible immune mechanisms, i.e., whether the reaction could be IgE- or T-cell-related. If an IgE-mediated mechanism is suspected, prick skin tests can be performed with soluble substances and intradermal tests with sterile soluble drugs. For a few drugs, there is a laboratory-based test for the detection of drug-specific IgE by serology (ImmunoCap method). T-cell reactions against the drug can be detected by skin tests (intradermal test and epicutaneous test). The possibilities of in vitro clarification have been improved recently: If an IgE-mediated reaction is suspected, the BAT is used. For late reactions, cyto-LTT in vitro is best suited to detect sensitization.
Immediate type reactions: basophil activation test: The BAT is suitable for the diagnostic clarification of an immediate-type reaction (usually a few minutes/hours after drug intake). In BAT, the reaction occurring in the body is “recreated” in the laboratory. The blood is incubated with the presumptive triggering drug in pure substance and in ascending concentration, whereby the basophils present in the blood are activated in case of sensitization. In addition to the release of mediators (histamine, heparin), various activation markers are also expressed on the surface of the basophils, which can be quantified using flow cytometry. Since the assay requires living cells, a fast sample transport time (<24h) is essential. Also, the test must be registered in the laboratory. The required test material is at least 4 ml EDTA blood.
The following groups of drugs have been shown to be appropriate for the workup of immediate-type MA with the BAT (ADR-AC experience): penicillins, cephalosporins, muscle relaxants, PPI, fluoroquinolones, and various disinfectants. If other drugs are tested, the test must still be considered experimental. As with the skin test, the sensitivity of the BAT decreases with distance from the event. Optimally, the BAT is thus performed within one year of the allergic reaction.
Late type reactions: Cytokine lymphocyte transformation test (cyto-LTT): For the diagnostic clarification of allergic late type reactions by means of in vitro laboratory diagnostics, the cyto-LTT proves to be helpful and – based on previous data – superior to the skin test and the normal LTT: In a 7-day cell culture of patient cells with the drug, specific T cells are stimulated, which secrete cytokines: Analysis of certain mediators in cell culture supernatants, namely IL-5, IL-13, IFN-y, granzyme B and granulysin is suitable to detect the different types of reactions. Depending on the distribution pattern of the cytokines, one can even draw conclusions about the disease pattern. Thus, patients with maculopapular exanthema tend to show increased IL-5 and IL-13 levels, whereas cytotoxic response mechanisms such as AGEP or DRESS show an increase in cytotoxic cytokines. Cyto-LTT requires 4050 ml of heparin blood, with the optimal collection time being two weeks to 1-2 years after the response has resolved, except in SJS/TEN, where the test should be performed as soon as possible. A broad spectrum of drugs can be tested in cyto-LTT. This includes the most important typical triggers of drug-mediated late-type reactions (details at www.adr-ac.ch).
Symptom progression and measures
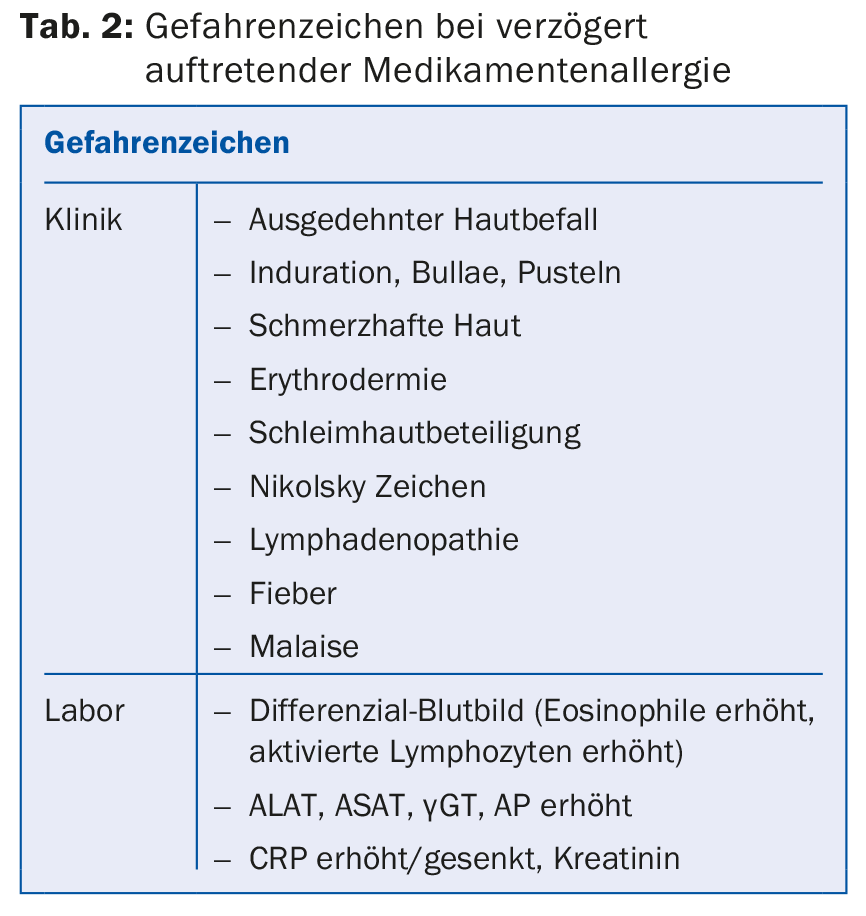
As a first measure, the medication that has only recently been administered should be discontinued. This is because it is unlikely that a drug that has already been taken for a long time (e.g. one year) will trigger an allergy. Depending on the symptom severity (Tab. 2), further measures are necessary. DRESS refers to a clinically severe systemic reaction (massive exanthema, malaise, facial swelling, hepatitis, and often eosinophilia) and is predominantly triggered by some specific drugs (Tab. 3). DRESS often occurs after several weeks of therapy and can cause lethal organ failure (carditis, hepatitis). Patients with severe exanthema and DRESS may continue to develop a new MA for years against new drugs (“multiple drug hypersensitivity”, MDH) [7]. In mild MA, short-term therapy with anti-H1 blockers is sufficient, supplemented by topical steroids. Systemic steroids are used for severe MA. Hospitalization and consultation of specialists are necessary and useful in bullous skin diseases (SJS/TEN), in DRESS and mostly in AGEP, because the courses are often surprising and experience with these severe MA is important. Follow-up of patients with DRESS is complicated because many patients have “flare up” reactions despite silencing of triggers and some patients develop MDH.
The duration of sensitization after MA has not been sufficiently studied. Cases were observed that still reacted strongly positive to the drug in the skin test or LTT after more than 12-20 years, so that a permanent MA must be assumed: This is especially true for severe MA such as DRESS, SJS/TEN and hepatitis. In anaphylaxis, evidence of allergy is higher in the first year after the event than later, because a spontaneous decrease in drug-specific IgE has been repeatedly observed. However, this decrease is not certain, so that – if the same drug is to be used again – a trial dose is administered first: The drug is administered at 1/100 to 1/10 of the daily dose and then rapidly increased to the normal dose within 3-6 hours (“graded challenge”). Re-exposure (“challenge”/provocation testing) to the full dose is contraindicated in severe reactions. In the case of the frequent, initially mild late reactions (exanthema), re-exposure after >2 years would be possible if it is an important drug class.
Take-Home Messages
- Adverse drug reactions are divided into type A and type B reactions [1,2]. Type A reactions are based on the mechanism of action of the drug. Type B reactions (drug allergies) are less common but potentially dangerous and are caused by an immune response to the drug.
- Drug allergies can be classified into immune-allergic, p-i, and pseudoallergic forms based on the mechanism of action of the drug with immune and inflammatory cells. Distinguishing features relate to rate of manifestation, dose dependence, clarification options, and genetics.
- Furthermore, immediate type reactions must be distinguished from late type reactions. In addition to history and follow-up, a differential blood count can provide diagnostic clues. Eliciting the triggering drugs is complicated. New in vitro tests facilitate the detection of the trigger both for immediate reactions (basophil activation test, BAT) and for late reactions (cyto-LTT).
Literature:
- Rawlins MD, Thompson JW: Pathogenesis of adverse drug reactions. In: Davies DM, ed. Textbook of adverse drug reactions. Oxford: Oxford University Press, 1977: 10-17.
- Rawlins MD: Clinical pharmacology: adverse reactions to drugs. BMJ 1981; 282: 974-976.
- Pichler WJ, Hausmann O: Classification of Drug Hypersensitivity into Allergic, p-i, and Pseudo-Allergic Forms. Int Arch Allergy Immunol 2016; 171 (3-4): 166-179.
- Pichler WJ, et al: Drug hypersensitivity: how drugs stimulate T cells via pharmacological interaction with immune receptors. Intern Arch Allerg Clin Immunol 2015; 168(1): 13-24.
- McNeil BD, et al: Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature 2015; 519 (7542): 237-241. doi: 10.1038/nature14022.
- Kowalski ML, et al: Classification and practical approach to the diagnosis and management of hypersensitivity to nonsteroidal anti-inflammatory drugs. Allergy 2013; 68(10): 1219-1232.
- Pichler WJ, Srinoulprasert Y, Yun J, Hausmann O: Multiple drug hypersensitivity. Int Arch Allergy Immunol 2017; 172(3): 129-138.
HAUSARZT PRAXIS 2018; 13(10): 12-16