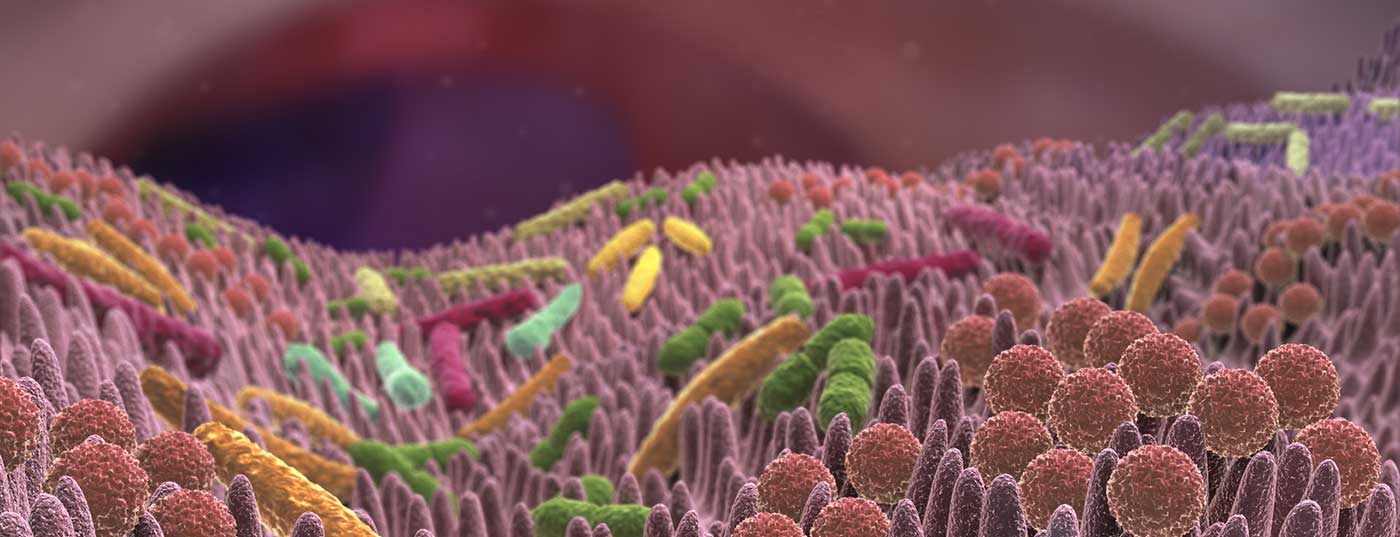
The complexity of the human intestinal flora is increasingly better understood. The gut even seems to have an impact on who responds to cancer immunotherapy and who doesn’t.
Checkpoint inhibitors, which activate the immune system, are extremely successful in some patients. Their application is based on the premise that the tumor is recognized by the immune system, but that this immune response is blocked, at least in part, by the checkpoints (e.g. PD-1/PDL-1).
For other patients, however, the response remains absent. Are other immunosuppressive mechanisms active here or does the immune system simply not recognize the tumors – so no immune response can be “deblocked” at all? Currently, a feverish search is underway for satisfactory assays that reliably predict response to PD-1/PD-L1 blockade. Three recent studies point to the role of the gut in this.
Study 1 – Antibiotics worsen response
A French team [1] found that primary resistance to checkpoint inhibitors was due to a specific gut microbiome composition. When stool from responders was transplanted into germ-free or antibiotic-treated mice, the antitumor effect of PD-1 blockade improved. Conversely, nothing happened when stool from non-responders was used. Studies of human stool from lung and kidney cancer patients at diagnosis showed a correlation between frequent occurrence of the bacterium A. muciniphila and later clinical response. Oral supplementation with this bacterium was able to “compensate” for failed stool transplantation (i.e., stool from non-responders), i.e., re-induce PD-1 blockade efficacy in mice.
The effect is also seen in humans: Individuals who had taken antibiotics to treat infections alongside cancer therapy had a poorer response to PD-1 inhibition than the overall cohort (their progression-free and overall survival was significantly shorter).
Study 2 – Significant differences in the human intestine
A US team [2] demonstrated significant differences in the diversity and composition of the gut microbiome of responders and non-responders in 112 melanoma patients treated with PD-1 immunotherapy. In the total of 30 vs. 13 stool samples, there was a higher diversity and increased occurrence of Clostridiales bacteria such as Ruminococcaceae. Patients with a “favorable” gut microbiome had better systemic and antitumor immunity (strong positive correlation between killer T cells in the tumor and presence of the mentioned bacteria). The same was true for germ-free mice that received transplanted stool from responders. Compared with patients who had intermediate and low diversity, progression-free survival was longest with high diversity.
Study 3 – Association between microbiome and response.
Last but not least, another US team [3] demonstrated a significant association between a commensal bowel composition prior to immunotherapy and subsequent clinical response – this in 42 patients with metastatic melanoma. In responders to PD-1 or CTLA-4 therapy, bacterial species that were common included Bifidobacterium longum, Collinsella aerofaciens, and Enterococcus faecium, whereas in non-responders, Ruminococcus obeum and Roseburia intestinalis were dominant.
The researchers assigned points for intestinal flora (“favorable”/”not favorable”); a ratio greater than 1.5 correlated with a response.
Can the knowledge be used?
A “healthy” intestinal flora seems to help patients in their fight against cancer. In contrast, a poorly balanced intestinal composition negatively affects immune cell activity and could prevent therapy response. There is much evidence to suggest that the gut microbiome should be considered when assessing therapeutic intervention, as it exerts a strong influence on the immune system.
All still very experimental, say some now. That’s right. The intestine is also only one of many possible reasons for a non-response. Numerous other biomarkers are being explored and some are already considerably further along in their therapeutic use (e.g., PD-L1 expression levels in tumors). The University of Zurich also reported possible new biomarkers in blood earlier this year [4]. Whether it will ever be possible to use the gut as a biomarker remains questionable due to the immense complexity of the microbiome. The three studies also suggest different bacteria play a role in the response. Standardization efforts are likely to prove difficult; many processes are simply still unclear.
Nevertheless, research activity in this area is high, and the three new studies strike a chord that has long been entertained by scientific reports. And they address an important clinical issue, that of manipulation. Can non-responders be “converted” to responders? A stool transplant as in the studies mentioned above would be conceivable, but it can also be simpler. The human microbiome is definitely a modifiable risk factor. Even diet or taking anti/robiotics can make a weighty difference. The first clinical studies are now in preparation.
An attempt to combine, for example, bifidobacteria in capsule form and PD-1 inhibitors to observe the response after colonization with “beneficial” bacteria seems quite feasible for now. It may be possible to assemble additional synthetic microbial communities in the future to optimize patient response to immunotherapy.
Literature:
- Routy B, et al: Science 2018; 359(6371): 91-97.
- Gopalakrishnan V, et al: Science 2018; 359(6371): 97-103.
- Matson V, et al: Science 2018; 359(6371): 104-108.
- Krieg C, et al: Nature Medicine 2018. DOI: 10.1038/nm.4466.
InFo ONCOLOGY & HEMATOLOGY 2018; 6(2): 5.