There are recent developments in the treatment of individual gastroenterological diseases. In addition to new therapeutic options with excellent efficacy and good healing prospects for those affected, tried-and-tested groups of substances are experiencing a revival.
Esophagus and gastric reflux: Gaviscon®.
Proton pump inhibitors (PPIs) are the most commonly prescribed drugs of all worldwide. Nonetheless, they can have relevant side effects if used unjustifiably on a long-term basis [1].
With unnecessary long-term therapy, acid deficiency leads to enteric bacterial overgrowth and Clostridium difficile-associated diarrhea. Pharmacokinetic interactions may further occur with simultaneous metabolism via cytochrome P450-dependent enzymes. Thus, attenuation of the effect of clopidogrel may increase cardiovascular risk. If gastroprotective agents are needed, H2 blockers or antacids should be used here.
In addition, the absorption of individual minerals is disturbed. In the case of magnesium, this can lead to tachycardia and neurological symptoms, especially with concomitant administration of diuretics and/or digoxin. Reduced calcium intake leads to increased fracture risk with long-term PPI use [2]. In addition, there is reduced absorption of vitamin B12 because too little gastric acid produces too little “intrinsic factor”. Numerous studies exist on potential side effects of long-term PPI therapy. Due to inhomogeneous collectives, they are not comparable without restriction.
The American Society of Gastroenterology (AGA) clears long-term PPI therapy only for patients with GERD (gastroesophageal reflux disease) and reflux-related complications, Barrett’s esophagus with or without reflux symptoms, and patients at high risk for bleeding on NSAID treatment. In all other patients, acid blockers should be discontinued promptly or switched to other agents such as H2 antagonists or antacids. The recommended alternative is Gaviscon®, which has been on the market since 1965 and has fallen into oblivion due to excessive PPI use. It is made of alginate. This floats on the stomach contents like a raft (“alginate raft”) by forming gel foam and protects against acid reflux more effectively than antacids [3,4].
Current therapy of hepatitis C
Previously, hepatitis C was treated with interferon and ribavirin for 24 to 72 weeks with side effects and a maximum 80 percent chance of cure. Since the introduction of the new “direct acting antivirals” (DAA), this has been reduced to 12 weeks – over 90% are cured. One drawback is the very high cost of therapy. One treats with combinations of two or three. In the case of concomitant liver cirrhosis, ribavirin is also given. With large treatment dynamics, the Swiss Society of Gastroenterology issued expert recommendations [5,6]. The European Association for the Study of the Liver (EASL) also designed a free APP (www.hcvadvisor.com) that prescribes the correct therapeutic path after entering the appropriate patient data.
Treatment for irritable bowel syndrome with constipation: Linaclotid/Constella®.
In irritable bowel syndrome, a distinction is made between subtypes with a tendency to constipation, diarrhea, or both. Linaclotide (Constella®) can be used for moderate to severe constipation. It increases the secretion of chloride and bicarbonate into the small intestinal lumen, thus enhancing intestinal transit [7].
Inflammatory bowel disease CED (ulcerative colitis, Crohn’s disease)
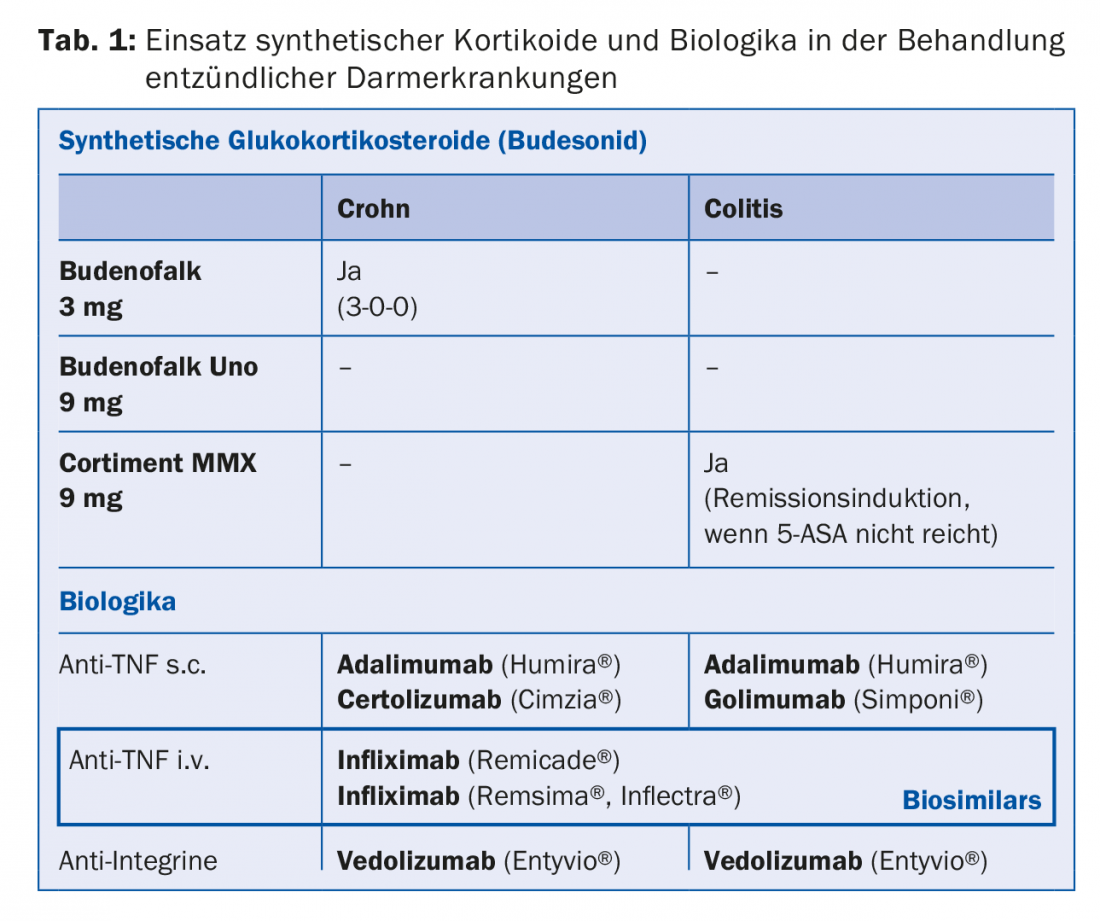
In ulcerative colitis, systemic corticosteroids used to be used if 5-ASA administration was unsuccessful. Today, Cortiment MMX® is administered with budesonide as a synthetic corticosteroid, the side effect profile of which is said to correspond to that of a placebo. The situation is similar for Crohn’s disease. Here, budesonide is successfully used as Budenofalk® with a single dose of 3 mg/d.
Biologics are also used in severe courses of ulcerative colitis and Crohn’s disease. In the course of inflammation, the organism produces large amounts of tumor necrosis factor-α as a natural mediator of inflammation. This is the point at which the TNF blockers attack. The substances used in Switzerland are adalimumab (Humira®), certolizumab pegol (Cimzia®), golimumab (Simponi®) and infliximab (Remicade®) (Tab. 1).
Planned gastroenterological procedures under ongoing anticoagulation.
The 2016 guidelines of the Swiss Society of Gastroenterology (SGG/SSG) provide a differentiated decision-making aid [9]. Procedures without bleeding risk (endoscopy without biopsy), with low bleeding risk (endoscopy with biopsy), and with high bleeding risk (endoscopy plus polypectomy) are distinguished.
Source: General Internal Medicine Update Refresher, November 15-18, 2017, Zurich.
Literature:
- Freedberg DE, Kim LS, Yang YX: The Risks and Benefits of Long-Term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice From The American Gastroenterological Association. Gastroenterology 2017; 152(4): 706-715.
- Fox M, Vavricka St, Halama M: Gastroesophageal reflux disease. Diagnostic and therapeutic options. HAUSARZT PRAXIS 2017; 12(6): 24-31.
- Tran T, Lowry AM, El-Serag HB: Meta-analysis: the efficacy of over-the-counter gastroesophageal reflux disease therapies. Alimentary Pharmacology and Therapeutics 2007; 25(2): 143-153.
- Chatfield S: A comparison of the efficacy of the alginate preparation. Gavicson Advance, with placebo in the treatment of gastro-esophageal reflux diease. Curr Med Res Opin 1999; 15(3): 152-159.
- Müllhaupt B, Fehr J, Moradpour D, et al: Treatment of Chronic Hepatitis C – November 2017 Update SASL-SSI Expert Opinion Statement. 2017;%20Word%
- Moradpour D, Müllhaupt B: Hepatitis C: current therapy; directly acting ativirals. Swiss Medical Forum 2015; 15(17): 366-370.
- Rao S, et al: A 12-week, randomized, controlled trial with a 4-week randomized withdrawal period to evaluate the efficacy and safety of linaclotide in irritable bowel syndrome with constipation. Am J Gastroenterol 2012; 107(11): 1714-1724.
- SMCCV Inflammatory Bowel Disease: Therapy of CED today and tomorrow. A small guide for those affected. (https://gesundheit-heute.ch2017/01)
- SGG: Antiplatelet agents, oral anticoagulants, and assessment for bleeding diathesis in elective gastrointestinal procedures (endoscopy, liver biopsy and FNA). Practical Management 2016. (www.sggssg.ch/richtlinien-empfehlungen/oral-anticoagulants-practical-management-2016/)
For further information on the use of PPI and Gaviscon®, see reference [2].
HAUSARZT PRAXIS 2018; 13(1): 35-36











