Which insulins are available and when are they used? To get the most out of insulin therapy, it is important to be familiar with the profiles and modes of action of the various active substances.
First, Prof. Dr. med. Peter Wiesli from the Cantonal Hospital Frauenfeld spoke about the long-acting insulins (basal insulins), formerly called “bedtime” insulins – even today the injection is normally recommended in the evening (dinner until bedtime). This when blood glucose rises overnight and there is a high morning reading. If blood glucose rises throughout the day and the morning value is good, but nighttime hypoglycemia is imminent, an injection of basal insulin in the morning may be appropriate. Generally, long-acting insulins are started when HbA1c is not within the target range in type 2 diabetics on two to three oral antidiabetic agents.
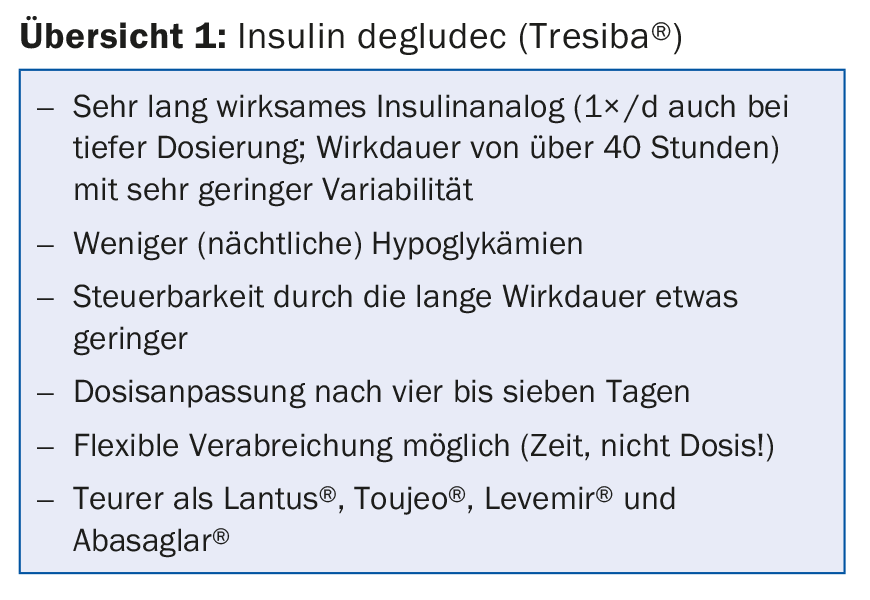
An important representative is insulin degludec, which has a very long duration of action of over 42 hours. This allows very stable, uniform insulin levels to be achieved in the steady state. Compared with insulin glargine, the variability in glucose lowering is much lower [1], HbA1c can be lowered equally (“non-inferior”) in type 2 diabetics with baseline values of 8.2% under oral antidiabetics, and the risk of nocturnal hypoglycemia is reduced due to the lower variability [2]. A new study [3] showed a 40% lower rate of severe hypoglycemia and a 53% lower rate of severe nocturnal hypoglycemia. Compared to the gold standard Lantus®, Degludec also proved to be at least as safe with regard to cardiovascular endpoints. The benefit in the area of hypoglycemia was also confirmed in patients with a correspondingly increased risk (SWITCH 2 study) [4]. Here, unusually low NNTs (Number Needed to Treat) for medicine were found of 1 at 1 year for severe or confirmed hypoglycemia (i.e., every patient benefited from degludec versus glargine) and of 3 for severe or confirmed nocturnal hypoglycemia (i.e., three patients needed to be treated over 1 year for one to benefit). This in the maintenance phase – for the entire treatment period, the NNT for severe hypoglycemia was 21.
Special mention should be made of the flexibility in injection timing. The efficacy of flexibly injected Degludec (intervals of 8-40 h) is as good as glargine or Degludec always injected at the same time of day [5]. This can be advantageous for patients who have difficulty injecting insulin at regular intervals, or for diabetics cared for by Spitex. Even if the time of injection is no longer important, it is advisable to recommend a certain regularity to the patient, otherwise the injection may be forgotten altogether. Overview 1 summar izes the above.
Other basal insulins
Insulin glargine 300 is glargine 100 triple concentrated (equal units in one-third volume compared to Lantus®). Toujeo® comes in an easy-to-use pen. It acts more consistently and uniformly over 24 hours in the steady state than glargine 100 [6]. Confirmed (≤3.9 mmol/l) or severe hypoglycemia in type 2 diabetics is less frequent at night and also throughout the day (EDITION 2 study) [7]. Flexible administration of ±3 hours is possible. The switch from Lantus® is 1:1 (if 1× basal insulin), the price is roughly comparable (higher dose), there are no safety concerns regarding heart and vessels or cancer.
Abasaglar® is a biosimilar of glargine, which means that, unlike a generic drug, it is not identical but has the same function as the original product.
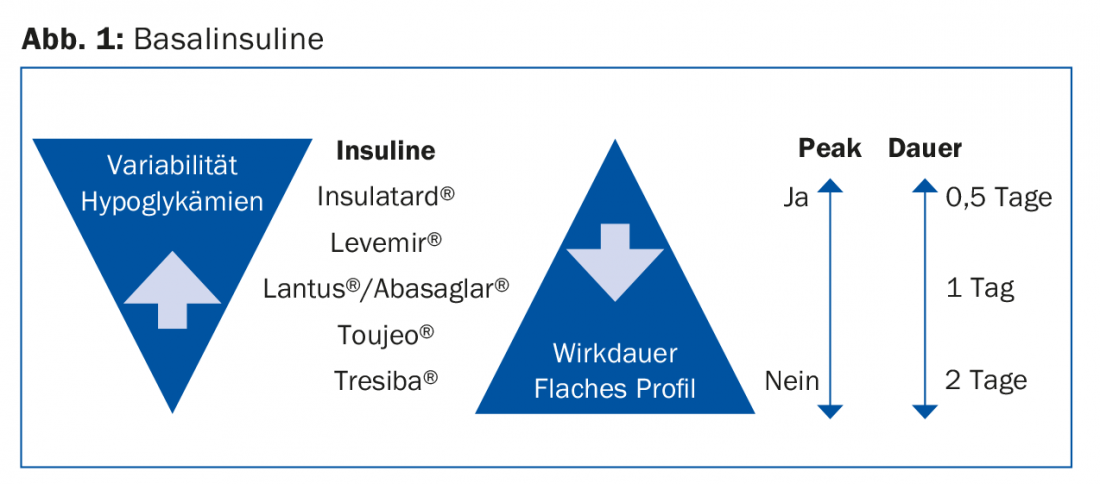
Figure 1 provides an overview of basal insulins. The higher the dose of insulin applied, the longer the duration of action.
Intensification of insulin therapy
If the blood glucose is not within the target range with the above measures, insulin therapy can be further intensified. A short-acting insulin can now be added to the previous treatment with two to three oral antidiabetic drugs plus a basal insulin at the main meal. Here, too, the principle applies: the higher the dose, the longer the duration of action. The insulin analogues Humalog®, NovoRapid® and Apidra® with an onset of action of five to ten minutes and a duration of three to four hours are suitable. In addition, Fiasp®, which acts even slightly faster than regular insulin aspart (with an earlier peak) [8].
In the basal-plus regimen, it is possible to administer a short-acting insulin before the main meal in a fixed dose (start with three to four units, continue OAD), or adjusted to the blood glucose before the meal (correction). In addition, there are mixed insulins such as Humalog Mix® or Ryzodeg®.
Finally, if this is no longer sufficient, a bolus of short-acting insulin at two or all meals may be considered.
Source: Diabetes Update Refresher, December 7-9, 2017, Zurich.
Literature:
- Heise T, et al: Ultra-long-acting insulin degludec has a flat and stable glucose-lowering effect in type 2 diabetes. Diabetes Obes Metab 2012 Oct; 14(10): 944-950.
- Zinman B, et al: Insulin degludec versus insulin glargine in insulin-naive patients with type 2 diabetes: a 1-year, randomized, treat-to-target trial (BEGIN Once Long). Diabetes Care 2012 Dec; 35(12): 2464-2471.
- Marso SP, et al: Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med 2017 Aug 24; 377(8): 723-732.
- Wysham C, et al: Effect of Insulin Degludec vs Insulin Glargine U100 on Hypoglycemia in Patients With Type 2 Diabetes: The SWITCH 2 Randomized Clinical Trial. JAMA 2017 Jul 4; 318(1): 45-56.
- Meneghini L, et al: The efficacy and safety of insulin degludec given in variable once-daily dosing intervals compared with insulin glargine and insulin degludec dosed at the same time daily: a 26-week, randomized, open-label, parallel-group, treat-to-target trial in individuals with type 2 diabetes. Diabetes Care 2013 Apr; 36(4): 858-864.
- Becker RH, et al: New insulin glargine 300 units-mL-1 provides a more even activity profile and prolonged glycemic control at steady state compared with insulin glargine 100 units-mL-1. Diabetes Care 2015 Apr; 38(4): 637-643.
- Yki-Järvinen H, et al: Glycaemic control and hypoglycaemia with new insulin glargine 300 U/ml versus insulin glargine 100 U/ml in people with type 2 diabetes using basal insulin and oral antihyperglycaemic drugs: the EDITION 2 randomized 12-month trial including 6-month extension. Diabetes Obes Metab 2015 Dec; 17(12): 1142-1149.
- Heise T, et al: Pharmacological properties of faster-acting insulin aspart vs insulin aspart in patients with type 1 diabetes receiving continuous subcutaneous insulin infusion: A randomized, double-blind, crossover trial. Diabetes Obes Metab 2017 Feb; 19(2): 208-215.
HAUSARZT PRAXIS 2018; 13(1): 38-39











