At Medidays Zurich 2016, the advanced training for general internal medicine in practice and hospital, Alzheimer’s dementia was a topic: its pathology is very complex and a causal therapy is currently not yet possible. In his presentation, Prof. Dr. Egemen Savaskan, Department of Psychiatric Research and Clinic for Geriatric Psychiatry PUK Zurich, addressed the current status of treatment recommendations and showed which measures are in the foreground. Pharmacological treatment continues to prove difficult in this regard.
In addition to cognitive disorders, neuropsychiatric symptoms are often observed in dementia disorders. They are behavioral disorders called behavioral and psychological symptoms of dementia (BPSD). “Treating these pharmacologically is a big challenge,” Prof. Savaskan explained at the very beginning of the presentation. This is because the neurotransmitter changes that occur are very complex: The loss of serotonergic, noradrenergic and acetylcholinergic neurons is in the foreground. The resulting neuropsychiatric symptoms are very diverse. After five years of dementia disease, almost all patients exhibit at least one symptom, with apathy leading the way, followed by depression, delusion, anxiety, motor agitation, irritability, agitation/aggression, hallucinations, and disinhibition.
Joint therapy recommendations of the professional societies
In this context, BPSD are predictors of disease progression to severe AD. According to the Cache County Dementia Progression Study [1], which included 408 patients with dementia, most affected individuals developed symptoms of psychosis, agitation, and aggressiveness during the observation period. Clinically relevant BPSD are associated with rapid dementia progression and early death. In this context, Prof. Savaskan mentions the situation of relatives and caregivers: “For them, the symptoms mean a great burden, and psychiatric illnesses such as depression are increasingly observed in them.”
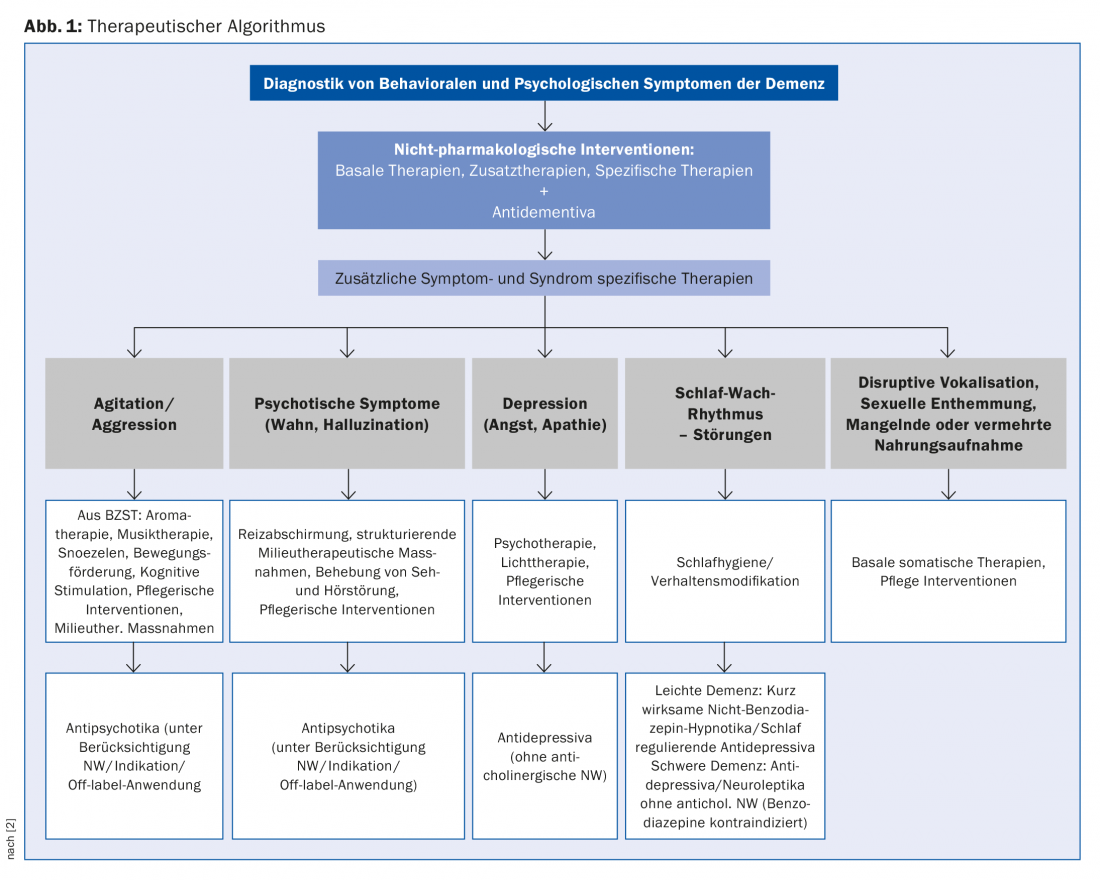
As far as the therapy of Alzheimer’s dementia is concerned, prevention is currently the most important approach, which is also successful. Therapy attempts to address the cognitive disorders, the accompanying symptoms of BPSD, and the somatic disorders. These measures are flanked by care for relatives and psychosocial measures (Fig. 1) . The Swiss professional societies have jointly developed therapy recommendations for this purpose [2]: “The aim is to show guidance for the therapy of the accompanying symptoms of dementia based on evidence and on the clinical experience of Swiss experts”. He said that consideration of clinical experience is important because most treatment options lack adequately controlled trials.
Nursing and psychosocial interventions as the first choice
Since non-pharmacological interventions, i.e. psychosocial interventions, have proven very successful in everyday clinical practice, they should be in the foreground according to the speaker and are recommended as an accompanying procedure. These include, for example, activation therapy, music therapy, light therapy, aromatherapy and physical activity. They are particularly effective in agitation, restlessness and sleep-wake rhythm disorders.
Behavioral management, structured life review, and cognitive-behavioral therapy have proven effective as psychotherapeutic procedures. A combined use of psychotherapy, psychoeducation and practical support for relatives shows the best effectiveness. In addition, for mild to moderate dementia, multicomponent programs with cognitive-behavioral interventions are more successful than single interventions.
Pharmacological therapies
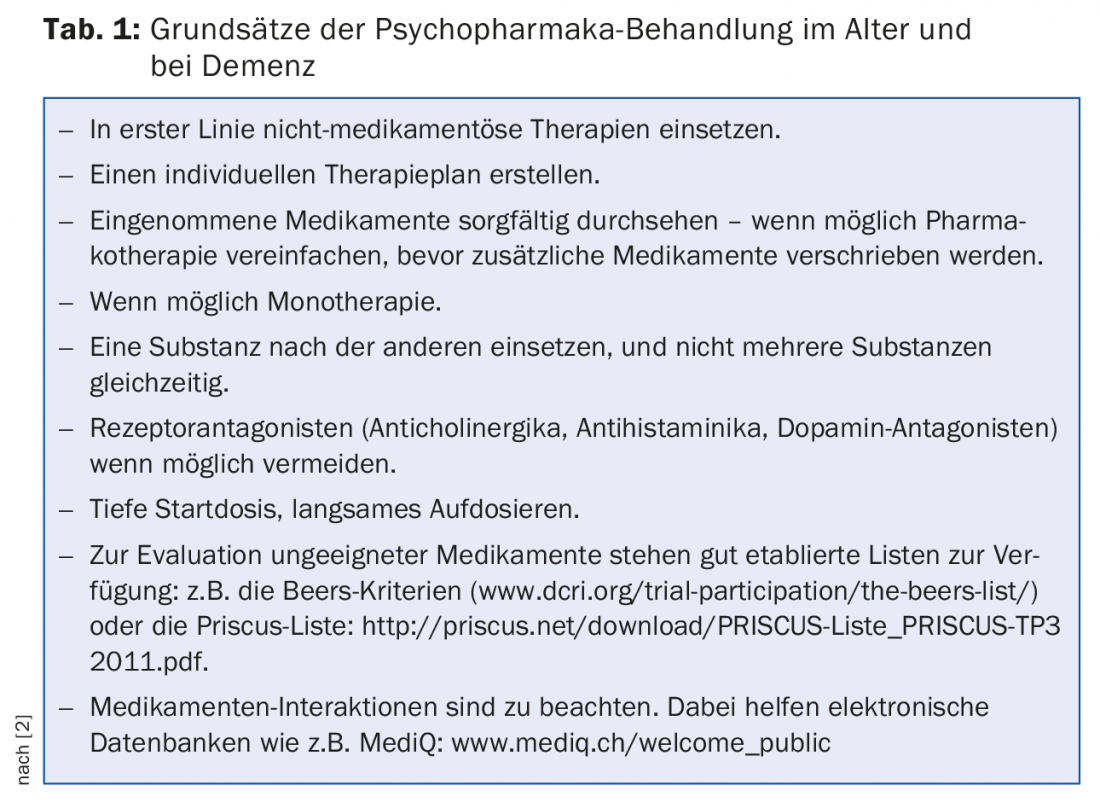
However, especially in severe dementia, pharmacological therapies are often unavoidable, and it is crucial here to adhere to certain principles (Tab. 1). In the following, the speaker explains the data for individual substance classes:
Antidementia drugs: most data are available for donepezil, with significant improvement in apathy, depression, tense, and irritability. The data situation is similar for galantamine and rivastigmine. The meta-analysis showed a medium treatment effect in mild to moderate Alzheimer’s dementia. Memantine shows positive effects on agitation, aggression, delusion, and hallucination. Cholinesterase inhibitors are most effective in apathy, depression, tension, and irritability. In this context, a study from 2009 [3] is available, according to which a combination treatment of cholinesterase inhibitors and memantine shows promising results.
Antidepressants: there are two controlled studies on tricyclic antidepressants, according to which the main side effect is severe cognitive impairment and anticholinergic side effects are a fundamental problem. Because of these side effects, the use of tricyclic antidepressants is not recommended. For serotonin reuptake inhibitors, the study situation is more favorable. When adequately indicated, improvement in depression can be observed. But the side effect profiles of the drugs must be taken into account.
Antipsychotics (typical and atypical neuroleptics): they are among the most commonly prescribed drugs, but they lead to serious side effects (extrapyramidal symptoms, sedation, cardiac symptoms, orthos. Dysregulation, falls) and increased mortality rates. An increased risk of cerebrovascular events should also be noted. Therefore, treatment should be given at the lowest possible dose, under close monitoring and for a limited period of time. The indication must be reviewed every six weeks. Haloperidol may be used only under strict indication and at low doses in the acute treatment of aggressiveness and psychotic symptomatology and in transitions to delirium. Before the use of antipsychotics, the following clarifications are necessary: Clinical history, ECG with QTc interval, electrolytes, family history (e.g., for torsades des pointes), drug interactions.
Ginkgo biloba extract EGb 761: Three studies are available here demonstrating cognitive effects in dementia (AD/VaD), effects on neuropsychiatric symptoms, and neurotransmitter effects: a double-blind study (GINDEM-NP) of 395 outpatients who had vascular or Alzheimer’s dementia with BPSD used 240 mg EGb 761 daily or placebo for a period of 22 weeks [4]. The target parameter was performance on the Syndrome Short Test (SKT). Here, there was a significant difference in favor of EGb 761 (p<0.001).
Two additional randomized, placebo-controlled, double-blind studies of dementia with neuropsychiatric symptoms, GOTADAY and GOT-IT [5,6], have been published. For both the total SKT score and the NPI composite score, both studies showed a significant benefit of EGb 761 compared with placebo at 24 weeks (p<0.001). Several studies also indicate neurotransmitter effects of EGb 761: an inhibition of MAO-A, a synaptosomal increase of serotonin and dopamine, and inhibition of dopamine reuptake at higher concentrations, and of serotonin and norepinephrine at lower concentrations. In addition, noradrenergic and serotonergic neurotransmission is enhanced, implying an antidepressant effect. A cognitive effect is provided by the enhancement of dopaminergic, cholinergic, and noradrenergic neurotransmission in the prefrontal cortex.
There are now also recent meta-analyses confirming stabilization or improvement in cognition, BPSD, activities of daily living, and quality of life under EGb 761 [7,8].
Source: Medidays, September 5-9, 2016, Zurich
Literature:
- Steinberg M, et al: Point and 5-year period prevalence of neuropsychiatric symptoms in dementia: the Cache County Study. Int J Geriatr Psychiatry; 2008: Feb;23(2): 170-7.
- Savaskan E, et al: Recommendations for diagnosis and treatment of behavioral and psychological symptoms of dementia (BPSD). Praxis 2014; 103(3): 135-148.
- Lopez O L, et al: Long-term effects of the concomitant use of memantine with cholinesterase inhibition in Alzheimer disease. J Neurol Neurosurg Psychiatry 2009 Jun; 80(6): 600-607.
- Napryeyenko O, et al.: GINDEM-NP Study Group: Ginkgo biloba special extract in dementia with neuropsychiatric features. A randomised, placebo-controlled, double-blind clinical trial. Int J Geriatr Psychiatry. 2011 Nov;26(11):1186-94.
- Ihl R, et al: Efficacy and safety of a once-daily formulation of Ginkgo biloba extract EGb 761® in dementia with neuropsychiatric features. A randomized controlled trial. Int J Geriatr Psychiatry 2011; 26(11):1186-1194.
- Herrschaft H, et al: Ginkgo biloba extract EGb 761 in dementia with neuropsychiatric features: a randomised, placebo-controlled trial to confirm the efficacy and safety of a daily dose of 240 mg. Journal of Psychiatric Research. 2012;46: 713-726.
- Meng-Chan T, et al: Efficacy and Adverse Effects of Ginkgo Biloba for Cognitive Impairment an Dementia: A Systematic Review and Meta-Analysis. Journal of Alzheimer’s Disease 43 (2015): 589-603.
- Von Gunten A, et al.: Efficacy of Ginkgo biloba extract EGb 761 in dementia with behavioral and psychological symptoms: A systematic review. The World Journal of Biological Psychiatry, 2015; Early Online: 1-12.
HAUSARZT PRAXIS 2016; 11(10): 48-50











