Radiological examinations are part of everyday life in dermatological practice. They are used for preliminary examination for system therapeutics, examination for system involvement, diagnosis of syndromes, investigation of causes and complications, and tumor follow-up. We must venture beyond the skin. We are currently under-aware of the usefulness of conventional radiography, MRI, and CT in detecting system involvement of diseases such as pulmonary sarcoidosis in the presence of scar sarcoidosis, malpositions leading to clavi formation, complications of ulcers and immunosuppression, and diagnosis of genodermatoses. Without the family doctor, the orthopedist and the radiologist, we are blind in one eye.
Radiologic imaging is a stepchild in dermatology, yet it is needed almost daily. Why do we need X-rays, MRI, CT and ultrasound?
- for diagnosis or exclusion of infections and tumors when using immunosuppression and biologics
- for tumor follow-up in malignant melanoma, lymphoma, Merkel cell tumor, spinalioma, dermatofibrosarcoma, etc. (exclusion of metastases and staging)
- for the search of systemic/skeletal involvement of autoimmune diseases, sarcoidosis, psoriasis, gout
- for the search of a system involvement/skeletal involvement of hereditary diseases.
- for the search of a system involvement/skeletal involvement of STD, reactive arthritis, Lyme disease, TbC
- in case of complications and infections
- for the search of structural changes leading to dermatological affections.
Immunosuppressants and biologics (targeted therapies)
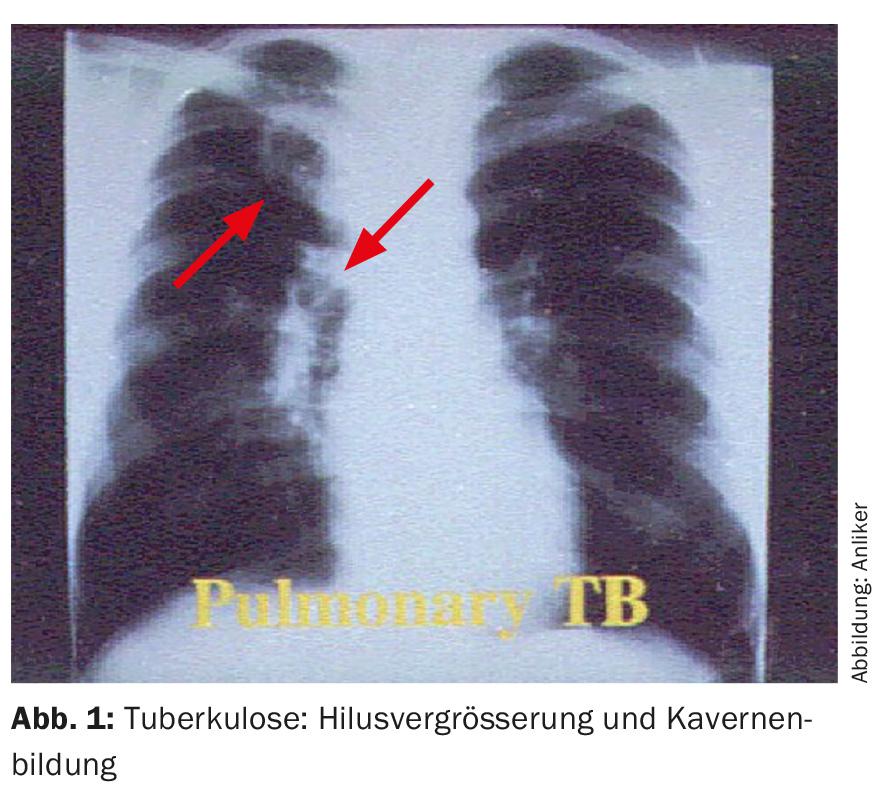
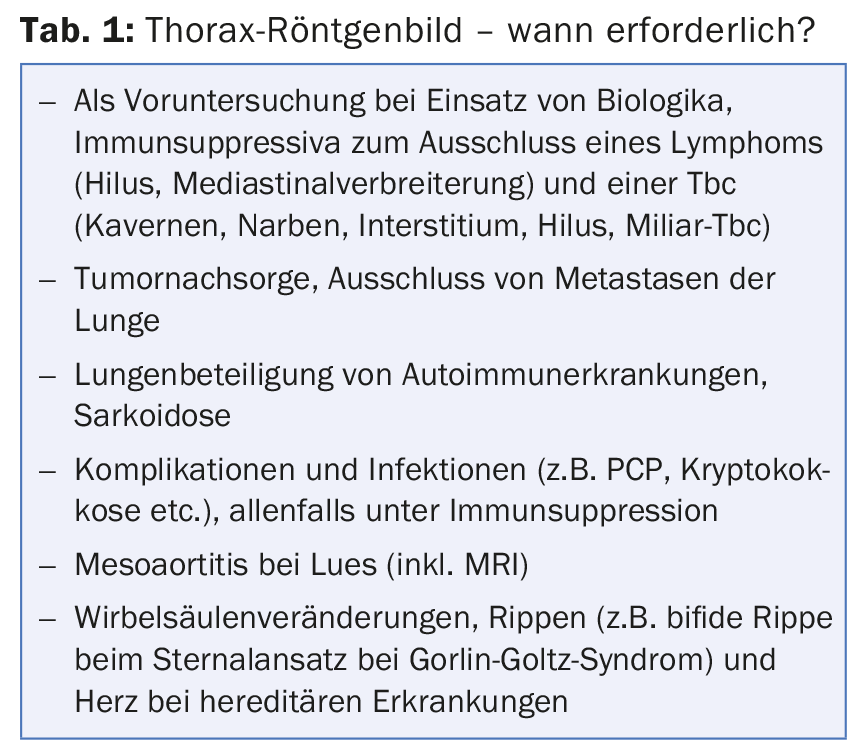
First of all, immunosuppressants and biologics, i.e. the so-called targeted therapies [1]. During screening prior to the use of immunosuppressants and biologics, the effects of which on pre-existing conditions are not fully understood, a chest X-ray (DV and lateral images) is performed. The aim is to exclude tumors, especially Hodgkin’s lymphoma, and to exclude tuberculosis (Fig. 1) [2].
This applies in particular to the use of methotrexate, mycophenolate mofetil, infliximab, adalimumab, etanercept, ustekinumab, apremilast, secukinumab, and ixekizumab. Exclusion of lymphoma is also recommended before the use of ciclosporin in the most severe atopic dermatitis and in general in the refractory dermatitides with whole-body involvement in addition to biopsy of the skin. Table 1 provides information on the other indications for thoracic imaging in dermatology.
Interstitial lung disease
Interstitial lung disease occurs in patients with dermatologic and clinical immunologic disease:
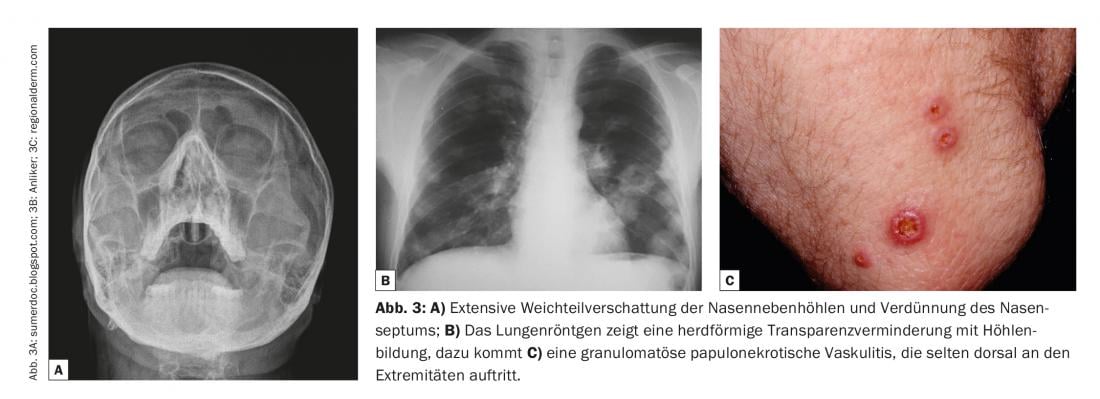
- In autoimmune diseases: Systemic sclerosis, dermatomyositis (Fig. 2), systemic lupus erythematosus, mixed connective tissue disease, rheumatoid arthritis, Wegener’s disease (Fig. 3).
- for atypical infections: Chlamydia tr., Tbc, P. carinii
- in sarcoidosis, idiopathic fibrosis, silicosis, hypersensitivity pneumonia
- when taking medication: antibiotics, chemotherapeutics, amiodarone, statins.
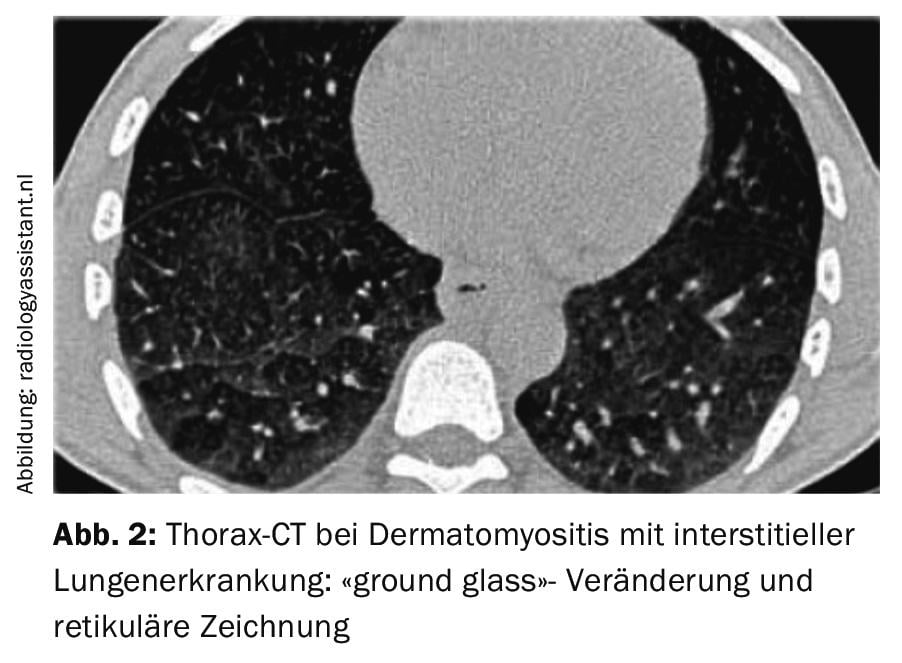
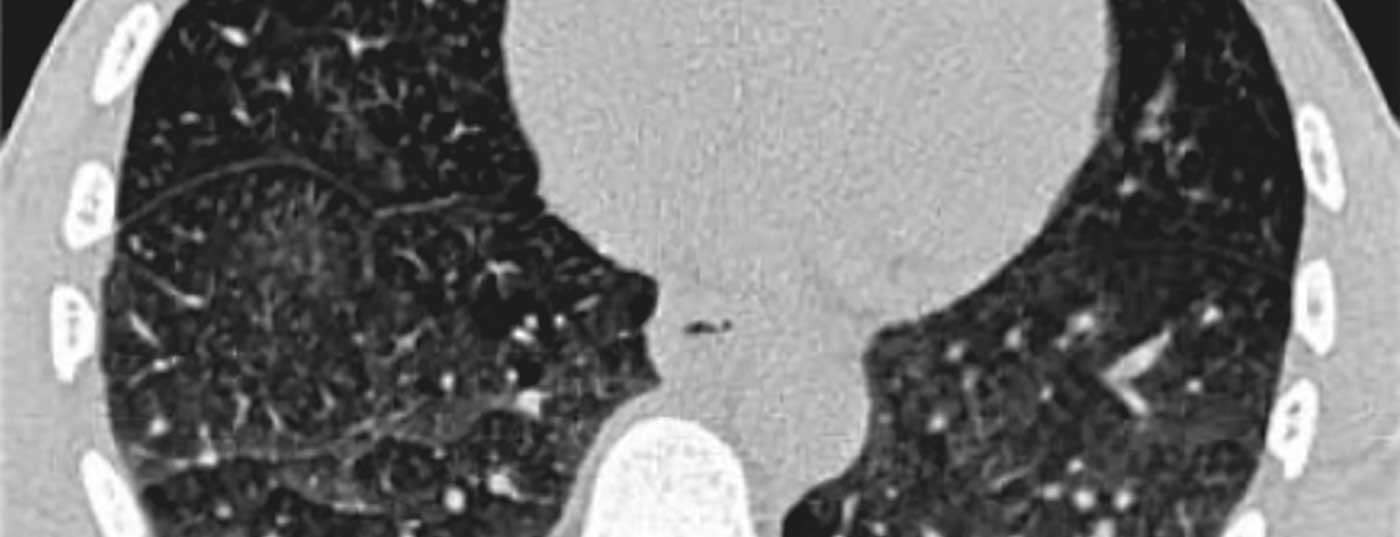
The changes often cannot be conclusively assessed by conventional chest radiography and may correspond to fibrosing pathology (sarcoidosis), alveolitis (e.g., Jo-1 antisynthetase syndrome), or granulomatous inflammation (e.g., Wegener’s disease). They can be reticular and planar (e.g., lupus erythematosus), requiring computed tomography or MRI for more accurate differentiation (Fig. 2) [3].
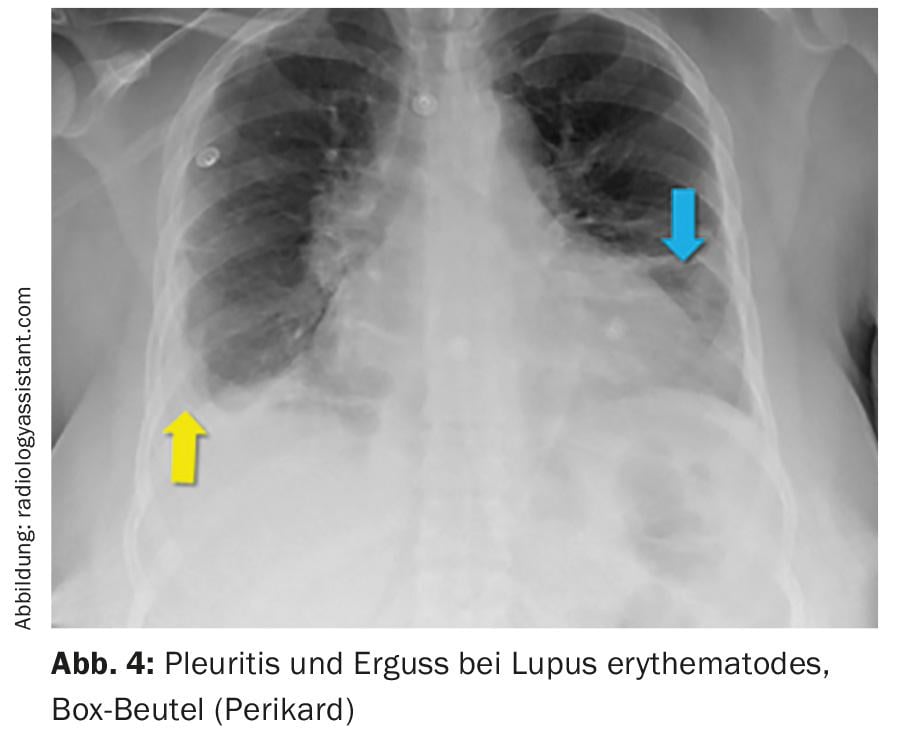
Radiological changes in lupus erythematosus.
The primary concern here is to look for systemic involvement: On chest x-ray, we look for pericarditis (Fig. 4), pulmonary involvement (pleurisy, inflammatory and fibrotic interstitial lung disease, alveolar hemorrhage, shrinking lung, pulmonary hypertension, bronchiolitis), and thromboembolic events.
Radiological changes in syphilis
Bone changes of congenital syphilis [4] mainly affect the metaphyses of the long bones with decreased mineralization. These then also lead to the formation of the saber sheaths tibiae. Radiographically, metaphyseal light bands are found, possibly due to granulomatous inflammation. More specific is lytic destruction of the medial proximal tibial metaphysis (Wimberger’s sign). Furthermore, there is a sawblade-like drawing of the metaphysis (“sawtooth metaphyses”). Mesoaortitis/aortic stenosis is the rare consequence of chronic infection/inflammation in stage III lues; however, the conventional chest radiograph is interpretable only after performing an MRI for aortitis and a cardiac echogram for any aortic stenosis. This is where we reach the limits of conventional X-ray.
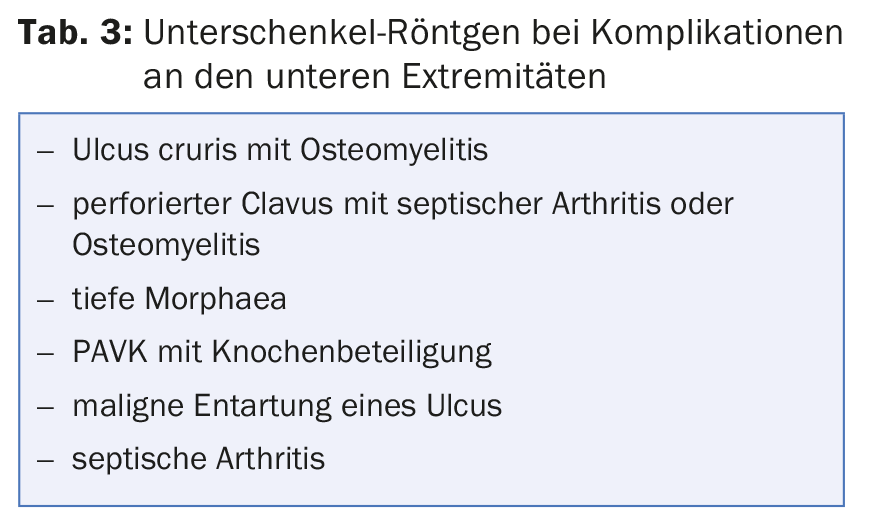
X-ray of the lower extremities
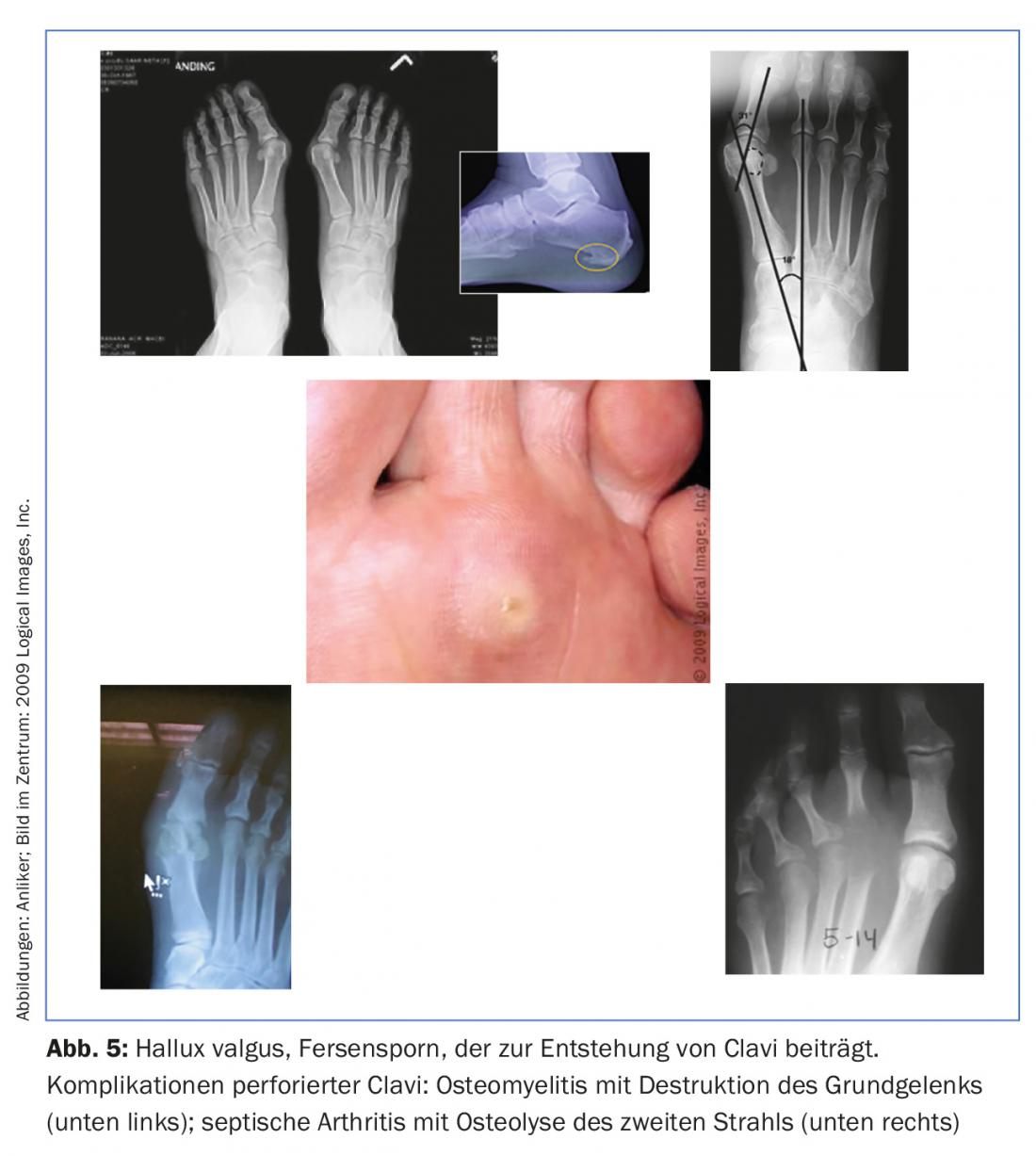
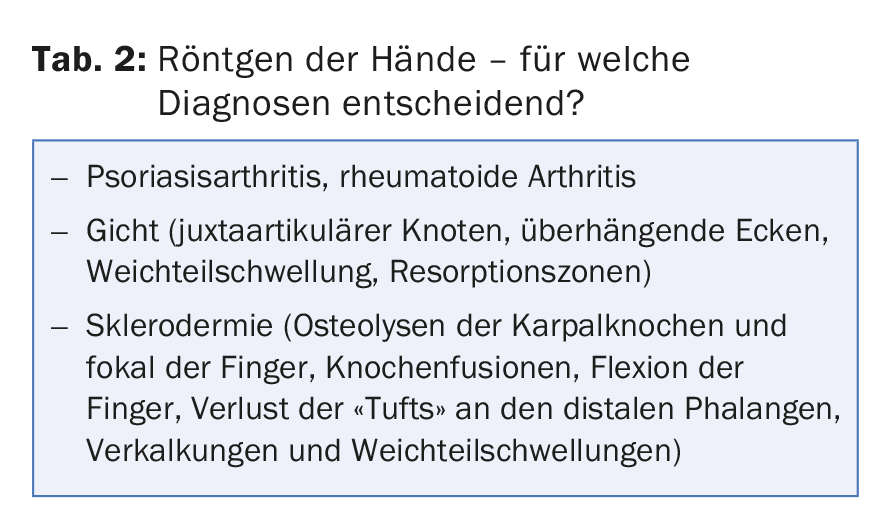
Here, we dermatologists are too inattentive, too late, or unaware of the examinations that can be useful to us in clarifying the etiology of complaints and finding complications (Tab. 2) [5,6]. Let’s take the example of a clavus. If the family doctor or orthopedist does not examine the feet radiographically, we will not find the underlying deformity of the toes, feet or overshooting osseous structures and the actual cause will not be corrected. The complications of chronic, possibly perforated clavi (Fig. 5) should also be recognized. Table 3 provides information on the complications of perforated clavi and ulcers.
Pelvis X-ray
In particular, inflammation of the ileosacral joint is sought and examined with the so-called Barsony image (ISG in a line). Here we deal with important systemic diseases and reactive arthitides, which are e.g. companions of erythema nodosum, chronic sexually transmitted diseases and dermatoses. Differential diagnoses include Reiter’s disease, rheumatoid arthritis, reactive arthritis (e.g., gastrointestinal infection), psoriatic arthritis, lupus erythematosus, Behcet’s disease, and SAPHO syndrome. Radiologically, this shows usuritus and sclerosis and diffuse shadowing in the joint space.
Iliac horns on the pelvis are found in nail-patella syndrome and candle wax-like lesions are an expression of osteopoikylosis in Buschke-Ollendorf syndrome.
X-ray for genodermatoses
In many genodermatoses, the syndromes are accompanied by sometimes characteristic skeletal changes – these must therefore be specifically sought, and under certain circumstances complications such as pathological fractures can be avoided. X-ray is crucial for diagnosis (e.g., in Gorlin syndrome, Goltz syndrome, nail-patella syndrome, Conradi-Hünermann syndrome).
SAPHO Syndrome
SAPHO syndrome (synovitis, acne, pustulosis, hyperostosis, and osteitis) [7] is an overlap of psoriatic and acneiform diseases. It is strongly activated by the innate (“inate”) immune system with neutrophil-rich inflammation, and radiologic imaging is very important. At times, hyperostosis, sclerosis, hypertrophy (especially sternoclavicular) is found in about 80% of patients Spinal involvement segmental, especially thoracic, in about 33% of patients Involvement of long bones in about 30% of patients.
The Sonozaki syndrome
Sonozaki syndrome is psoriasis-related and also shows overlap with SAPHO syndrome. It is characterized by eruptive palmoplantapustulosis and osteoarthritis with frequent involvement of the sternoclavicular joint (Fig. 7) .
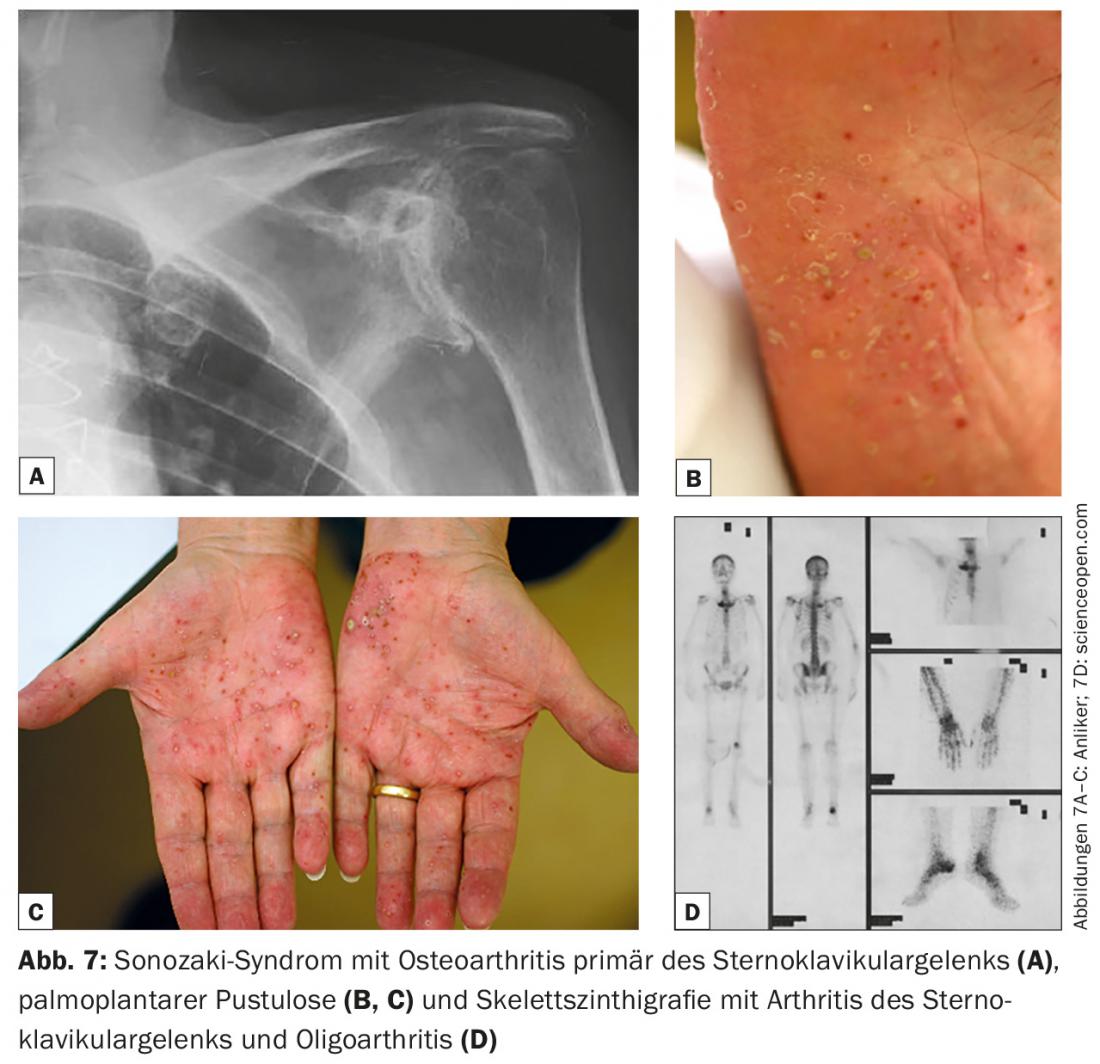
It is a subgroup of seronegative arthritis (as well as psoriatic arthritis, Reiter’s disease, ankylosing spondylitis). Increased sedimentation and leukocytosis are found. Antibodies are negative, HLA B27 is negative, and strong immunosuppressive therapy is often required. Described are the use of: CyA MTX, steroids, colchicines, sulfasalazines, and NSAIDs.
Acknowledgments: Dr. med. Thomas Kluckert, Radiology Cantonal Hospital St. Gallen, for critically reviewing and imparting important insights for a non
radiologists, Prof. Dr. med. Johannes von Kempis and Dr. med. Rüdiger Müller, Rheumatology KS St. Gallen, for their cooperation in rheumatological-dermatological patients.
Literature:
- Kolios AGA, Yawalkar N, Anliker M, et al: Swiss S1 Guidelines on the Systemic Treatment of Psoriasis Vulgaris. Dermatology 2016, June 21. doi:10.1159/000445681. [Epub ahead of print]
- Cantini F, et al: Guidance for the management of patients with latent tuberculosis infection requiring biologic therapy in rheumatology and dermatology clinical practice. Autoimmune Rev 2015 Jun; 14(6): 503-509.
- Ohno Y, et al: State-of-the-Art Imaging of the Lung for Connective Tissue Disease (CTD). Curr Rheumatol Rep 2015 Dec; 17(12): 69.
- Barbin CM, et al: Computed Tomographic and Morphologic Features of Syphilis of the Aorta. Am J Cardiol 2015 Oct 15; 116(8): 1311-1314.
- Williamson D, Sibbald RG: Chronic recurrent multifocal osteomyelitis: a rare association with pyoderma gangrenosum in adults. Br J Dermatol 2002 Sep; 147(3): 611-613.
- Bonchak JG, et al: Calciphylaxis: a case series and the role of radiology in diagnosis. Int J Dermatol 2016 May; 55(5): e275-e279.
- Li C, et al: Synovitis, acne, pustulosis, hyperostosis and osteitis syndrome: a single centre study of a cohort of 164 patients. Rheumatology 2016 Jun; 55(6): 1023-1030.
DERMATOLOGIE PRAXIS 2016; 26(4): 18-21