The number of patients with clinically advanced cardiacinsufficiency is increasing worldwide. If conventional therapeutic options have been exhausted, it is necessary to evaluate whether the criteria for heart transplantation are met. Artificial heart support systems (“artificial hearts”) can bridge the time until heart transplantation, but they are also increasingly used as a definitive solution. Total artificial hearts (“TAH”) replace the no longer functioning heart; in ventricular assist devices (“VAD”), the no longer functioning biological heart is left in place and a pump usually supports the left ventricle. With current generation cardiac assist devices, more than 80% of patients survive the first year after implantation, and 75% are still alive after three years.
Ludwig Rehn (1849-1930) first documented treating a stab wound to the right ventricle with three sutures on September 9 1896. At the 26th Congress of the German Society of Surgery, he concluded his case presentation with the words: “The feasibility of cardiac suturing should now probably not be doubted.” He hopes that his case will stimulate further work in the field of cardiac surgery. This statement must be seen in the context of a quote by Theodor Billroth (1829-1894): “The surgeon who would ever attempt to suture a wound of the heart can be sure that he would lose the respect of his colleagues forever.” Whether Billroth really said this sentence is doubted in expert circles, but it cannot be ruled out. For parallels are many to be found in medical history when pioneering work is done and colleagues are rebuked due to lack of understanding or even ill will.
Very similar reactions accompanied the rapid development of mechanical circulatory support, which is now indispensable. On 21. March 1986, the weekly newspaper “Die Zeit” published the following paragraph under the title “Deadly sensation – the macabre game with the artificial heart”: “As far as artificial hearts are concerned, however, the professor had to know how problematic this technique is judged by experts. Only two patients have survived in America with artificial hearts. Their condition is reported to be appalling and inhumane. Even assuming that the Berlin surgeon had chosen a ‘hopeless case’ for his premiere, it must have crossed his mind that the law protects human dignity even and especially in dying.” 20 years later, long-term mechanical circulatory support embodies a therapeutic option that is in part equal to heart transplantation and in some situations even superior.
More and more patients with heart failure
It is estimated that about 200,000 people in Switzerland live with heart failure. 5%, or approximately 10,000 patients, are in a clinically advanced stage with dyspnea corresponding to the functional class NYHA III to IV. As a reflection of the progress of successful medical care, mortality from cardiovascular disease has decreased in the last two decades, while the incidence and prevalence of heart failure have increased markedly [1]. The therapy of heart failure recommended by the professional societies follows a specific step-by-step scheme. Once therapeutic options with medications, pacemakers, and conventional surgical interventions have been exhausted, it is necessary to evaluate whether the criteria for performing heart transplantation (HTx) are met [1].
Total artificial heart and heart support pump
Due to the long-standing and recently increasing discrepancy between the number of donor organs needed and the number of patients on the waiting lists, work on artificial heart support systems (“artificial hearts”) has been ongoing for several decades. On the one hand, these are intended to bridge the time until a heart transplant can save the patient, and on the other hand, with the help of sophisticated systems, the dependence on donor hearts will become history in the future. In fact, several artificial hearts have already been developed, and others are undergoing technical trials.

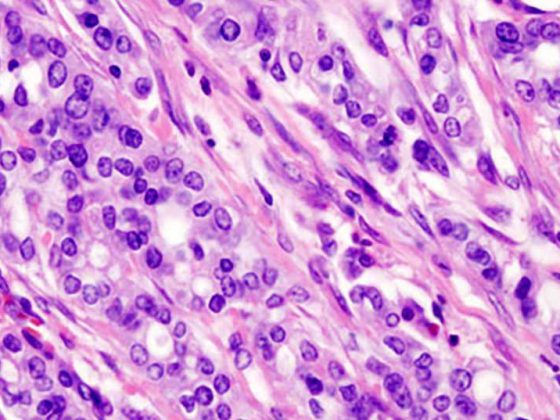
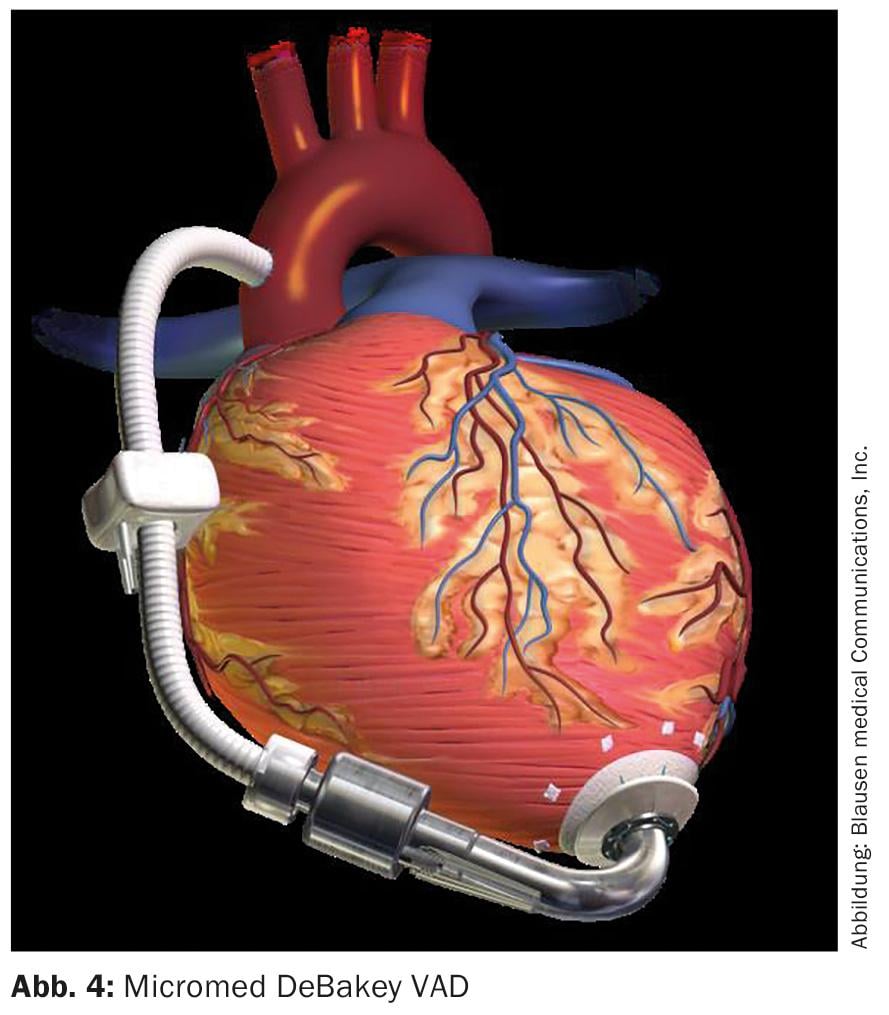
In total artificial hearts, the no longer functioning heart is replaced by two interconnected mechanical pumps (Fig. 1) . These take over the function of the removed left and right ventricle (“total artificial heart”, TAH). Today, total artificial hearts are rarely used in clinical practice. This is in contrast to the routinely used ventricular assist device (VAD). With these devices, the biological heart that is no longer functioning is left in place (Fig. 2). A pump usually supports the left ventricle. However, the right ventricle must still be strong enough for this. The distinction between total artificial heart and heart assist pump is important, even though both concepts are popularly referred to as “artificial heart”.
Jarvik-7: the first permanent artificial heart
At the beginning of the story is the total artificial heart. Shortly after the first heart transplant, the first artificial heart implantation is performed by U.S. surgeon Denton Cooley at the Texas Heart Institute in Houston on April 4, 1969. The 47-year-old patient received an artificial heart designed by Domingo Liotta, which was replaced with a natural heart after 65 hours. Shortly after the heart transplantation, the patient died as a result of immunological tissue rejection.

The first permanent heart implant is considered to be Robert Jarvik’s Jarvik-7 (Fig. 3), which was implanted in retired dentist Barney Clark on December 2, 1982, in a seven-hour operation in Utah by William DeVries. Clark survived 112 days and suffered multiple thromboses before dying. On November 25, 1984, American William J. Schroeder was also implanted with a Jarvik-7. He survived 620 days and died of a stroke on August 6, 1986. After various modifications, the Jarvik heart is now used under the name CardioWest, mainly in the USA. To date, over 1250 CardioWest hearts have been implanted. The system consists of two pneumatically driven, separable mechanical artificial heart chambers and two mechanical valves each. The system was approved by the FDA in 2004 as the first and so far only artificial heart for temporary bridging (until transplantation) and in 2012 as a permanent artificial heart.
From artificial heart to VAD
In Europe, the heart surgeon Emil Bücherl has also been working on an artificial heart since the 1960s in Berlin. After animal experiments, the first implantation of this Berlin system took place in 1986 in a patient who was, however, extremely seriously ill – without success. Just one year later, the time until heart transplantation was successfully bridged in another patient.
From a technical point of view, the “Bücherl artificial heart” was designed similarly to the CardioWest artificial heart. Nevertheless, its further development was not pursued because the “total artificial heart” concept was abandoned in Berlin in favor of cardiac support by means of VAD. The more flexible and smaller support pumps would deliver the same, if not better, clinical success rates. According to those responsible, the possibility of a “biological backup” by the heart remaining in the body would also be advantageous, which is of course ruled out in the case of total artificial hearts. Also, heart recovery would still be possible this way.
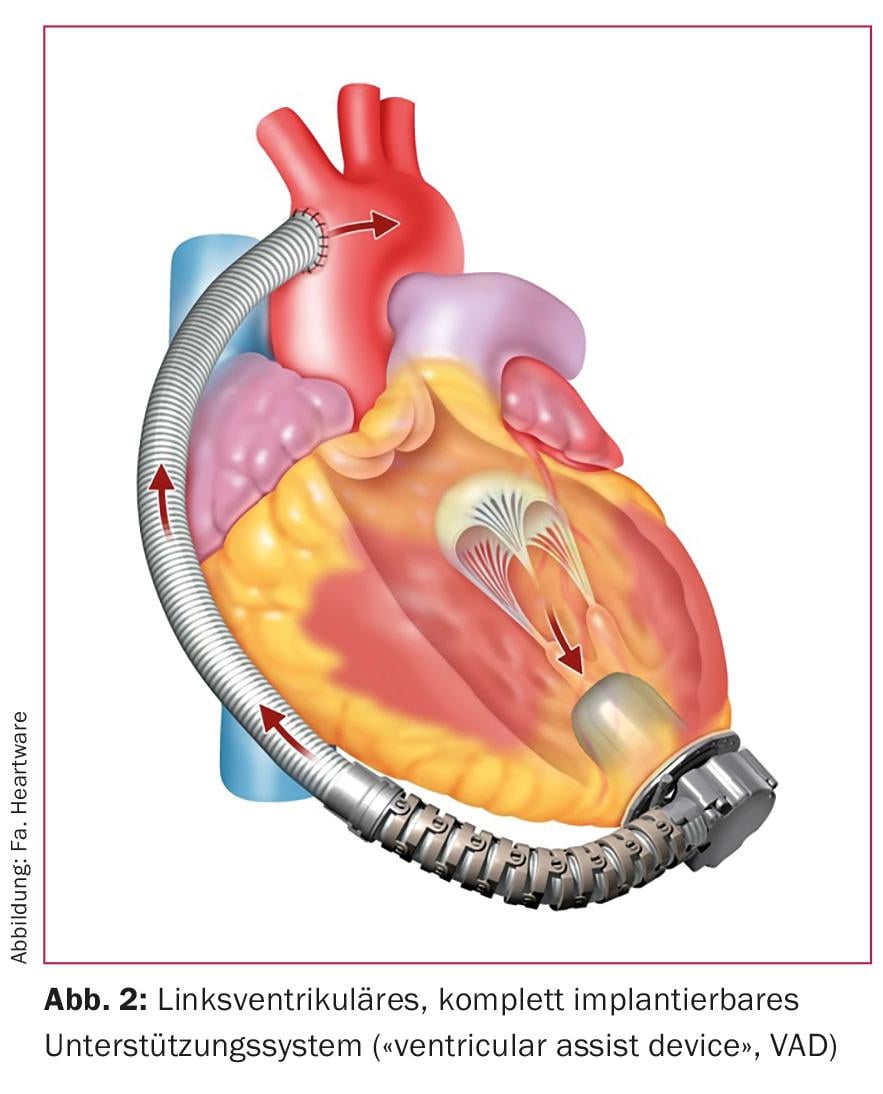
The world’s first implantation of a non-pulsatile axial VAD system at the German Heart Center in Berlin on November 13 1998 can be seen as a breakthrough in modern mechanical cardiac support. The “Micromed DeBakey VAD” (Fig. 4), the result of a collaboration between Michael DeBakey and NASA, paved the way for a completely new concept in cardiac support. It made possible a reduction in mortality and morbidity that had previously seemed impossible, as well as a miniaturization of systems. These could be connected directly to the cardiac apex of the left ventricle and were located intrathoracically in the pericardium. A transcutaneously routed cable allowed power supply and control via a handy control device.
Clinical success was primarily reflected in the long-term discharge of patients home. Several VAD systems have been approved for destination therapy, i.e. as the final solution for the patient – this in contrast to bridge-to-transplant therapy as a bridging measure until a suitable organ is obtained.
Modern VAD systems: fully implantable
Complete replacement of cardiac function was historically at the beginning of organ replacement concepts, but TAH failed to gain acceptance due to technical difficulties. Earlier VADs were extracorporeal simply because of their size and therefore had an increased complication rate because of the percutaneous cannulae. VAD therapy of the so-called second and third generation is performed exclusively by means of aggregates that generate a continuous flow (not pulsatile) and are fully implantable except for the control cable.
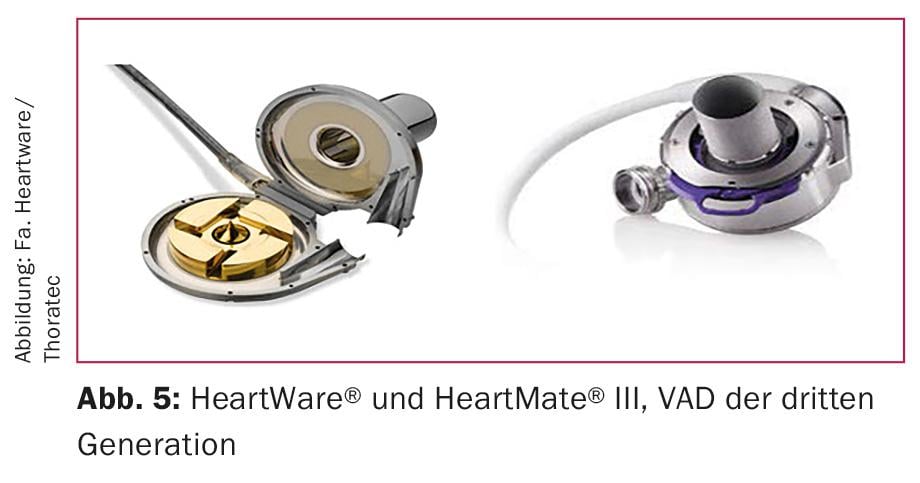
Another step was the miniaturization of the systems. Today’s centrifugal pumps are combined electromagnetic and hydrodynamic impellers that achieve flow rates of up to 8-10 l/min, depending on upstream and downstream loads. These pumps can also produce some pulsatility, which is thought to protect against bleeding complications and valve leakage, especially during very long periods of support. The main representatives are the HeartWare® system and now also the Thoratec HeartMate® III (Fig. 5).
In the majority of patients, left ventricular assist device (LVAD) alone is sufficient. However, due to the progressive system miniaturization, complete implantability is now also possible without any problems in the case of biventricular support.
Heart transplant results
If we look at epidemiology, waiting times on transplant lists and organ supply, we see that in the future only a very circumscribed group of people will be able to receive a heart transplant. Since transplant outcomes will suffer from the proportion of patients in high-urgent status, the question arises to what extent current and upcoming generations of support systems will compete with transplantation in the coming years. A 1-year survival of more than 80% of patients after heart transplantation is considered a minimum goal to strive for, which has been consistently achieved in international statistics in recent years [2]. It must be emphasized here that the statistics of the USA – with a large donor pool and short waiting times – have a significant positive influence on the results. In contrast, when looking at German data, one sees an alarming deterioration in outcomes with less than 80% survivors in the first year after transplantation. This deterioration is due, on the one hand, to the poorer general condition of the patients (disproportionately high share in the high urgency state) and, on the other hand, to the increasing percentage of older and, in some cases, no longer completely undamaged donor hearts.
Swiss transplantation results are exactly at the “magic” limit of 80% and thus also start to lag behind the international comparison [3]. We have to ask ourselves how and with what we can stop this trend. How do patients with modern third-generation artificial hearts compare to heart transplantation? Here it is useful to highlight long-term results, but also impressive short-term results.
VAD: survival rate of over 80%
In patients with first- and early second-generation artificial hearts, surgical trauma including bleeding complications resulted in quite high morbidity and mortality. Current studies show that implantation is now problem-free, at least for third-generation devices. An example is the recently completed pivotal study of HeartMate® III: Of 50 patients who received this last-generation artificial heart as bridging or destination therapy, 92% survived the first six months. Minimally invasive implantation options via anterolateral thoracotomy with partial sternotomy, which can extremely reduce surgical trauma, are partly responsible for this.
The 1-, 3-, and 5-year results with younger second- and early third-generation systems are also promising. Well over 80% of patients are alive after one year, 75% after three years, and 61% after five years. In order to be able to speak of real competitiveness, current generations of devices will have to measure themselves against long-term survival, since these patients naturally belong to the older and sicker ones already due to their exclusion from heart transplantation [5,6].

New goals: better batteries, wireless operation
With the last generation of artificial hearts, a level of implantability has been reached that can hardly be surpassed. Further miniaturization is planned, but is also viewed critically. The current generation (Fig. 6) is certainly seductively small. However, due to extremely high speeds and technical complexity, these devices also carry a risk of greater susceptibility to error in long-term use – an area where it will become apparent whether modern artificial heart therapy can become an alternative to the gold standard of heart transplantation. Improvements are needed primarily in the development of batteries to increase patient autonomy and in the elimination of the drive cable as a significant source of infection. Here, wireless data and power transmission is an important goal.
Literature:
- McMurray J, et al: ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012. Eur Heart J 2012; 33: 1787-1847.
- ISHLT Transplant Registry Quarterly Reports for Heart: Survival Rates for Transplants performed between April 1, 2010 and March 31, 2014, based on UNOS/ISHLT data as of March 27, 2015.
- Annual Swiss Transplant Cohort Study report (May 2008- Dec 2012), August 2013.
- Netuka I, et al: Fully Magnetically Levitated Left Ventricular Assist System for Treating Advanced HF: A Multicenter Study. Am Coll Cardiol 2015 Dec; 66(23): 2579-2589.
- Takeda K, et al: Long-term outcome of patients on continuous-flow left ventricular assist device support. J Thorac Cardiovasc Surg 2014; 148: 1606-1614.
- Sabashnikov A, et al: Outcomes after implantation of 139 full-support continuous-flow left ventricular assist devices as a bridge to transplantation. Eur J Cardiothorac Surg 2014; 46: e59-66.
CARDIOVASC 2016; 15(3): 19-21