The annual meeting of the Swiss Neurological Society was held in Bern at the end of October 2015. In a series of lectures, various causes of headaches were presented and explained. This showed that headaches in some patients can have complex backgrounds – for example, the overuse of painkillers or hormonal fluctuations. The care and treatment of affected patients is correspondingly complex and often protracted.
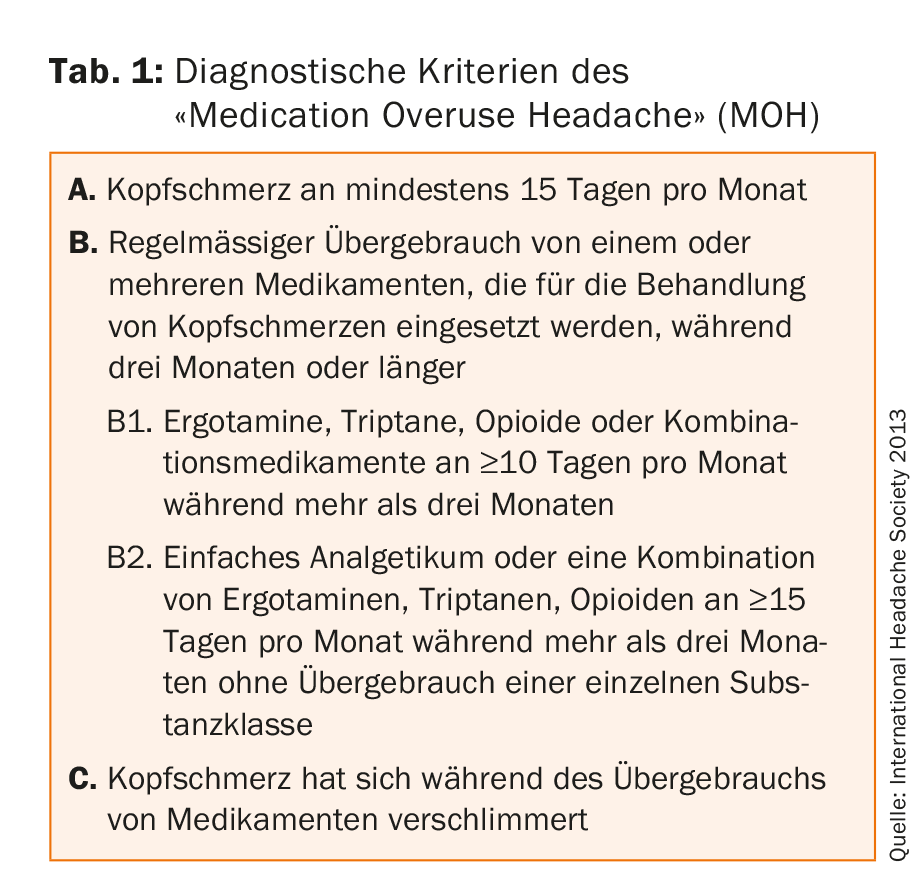
Prof. Dr. med. Peter Sandor, RehaClinic Zurzach, gave an overview of headaches that occur as a result of overuse of headache medication (Medication Overuse Headache, MOH). Compared to other headache types such as tension headache (60% of the population) and migraine (15%), MOH is rare with a prevalence of 2%. However, around 160,000 people in Switzerland are affected – a considerable number.
Chronic headaches change the brain
MOH is a so-called “transformation headache”: frequent headache attacks turn into chronic headaches if the patient takes medication too frequently (tab. 1). Virtually all common headache medications can trigger an MOH. MOH is strongly associated with psychiatric disorders (depression in over 20%, anxiety disorders in 3.5%), and the personality structure of patients often resembles that of drug addicts (reduced impulse control). Pathophysiologically, patients also demonstrate changes in the frontal gray matter and brainstem that regress after successful withdrawal.
A first attempt at withdrawal can be performed on an outpatient basis if the MOH has not been present for more than two years, if the patient does not have relevant psychiatric comorbidities, and if the patient is not dependent on sedatives or opioids. If these conditions are not met, inpatient withdrawal is necessary.
During inpatient withdrawal, the patient stops taking medication for acute headache and receives 100 mg/d prednisone (along with a PPI) for five days. During this time, attempts should be made to establish prophylactic headache therapy based on the type of headache. The patient should also keep a headache diary.
Rehabilitation after withdrawal
Inpatient withdrawal is too short for comprehensive patient education and additional measures such as exercise or behavioral therapy to be established. For this reason, subsequent rehabilitation may be useful. This is particularly appropriate for patients who have already undergone repeated, failed therapies or for patients with relevant psychosocial problems (partnership, workplace, psychiatric illness). During rehabilitation, which lasts two to three weeks, various therapy components are applied (tab. 2) . In Zurzach, there is a rehabilitation group with exclusively headache patients.

The frequency of headache attacks after withdrawal depends on the substance abused: when triptans are overused, the pain disappears more quickly than when other classes of substances are overused. After withdrawal, patients are not prohibited from using headache medications. However, these are to be used selectively, and no more often than ten days per month. Or as the speaker put it, “Hit hard or don’t hit at all.”
Hormonal aspects in migraine patients
Information on menstrual migraine and menstrual attacks was provided by Prof. Anne MacGregor, MD, London, UK. These two types of headache are not the same: in menstrual migraine, headache attacks occur predominantly (if not exclusively) during menstruation; menstrual attacks affect patients who experience headache attacks throughout the menstrual cycle, including during menstruation. This distinction is important for therapeutic consequences. For menstrual migraine, prophylaxis is perimenstrual; for menstrual attacks, it is according to standard prophylaxis for migraine. For this reason, patients should first keep an accurate headache diary so that one can be clear about the pattern of migraine attacks.
Menstrual attacks: painkillers sufficiently high dose
In menstrual attacks, therapy should be optimized. Many women are undertreated because they are reluctant to take pain medication for several days in a row. However, this is often necessary. Patients should therefore be informed that it is not the individual doses that matter, but the number of days per month that they swallow painkillers. Prof. MacGregor recommended a combination of a long-acting triptan and an NSAID for medication, which should possibly be used shortly before the onset of menstruation. It is also important to elicit possible seizure triggers – for example, dehydration, skipped meals, long trips, alcohol, or too little sleep.
Prophylaxis for menstrual migraine
Several options are available for perimenstrual prophylaxis in menstrual migraine. Triptans during 5-7 days have evidence levels A and B. The medication should be taken about two days before the onset of menstruation. In women who do not have a regular cycle – that is, most! – but this is difficult. The same problem exists with the use of an estrogen gel for seven days, because here, too, treatment should be started about five days before menstruation. The administration of estrogen also prolongs the menstrual cycle, and estrogen withdrawal increases the risk of migraine. Taking NSAID during menstruation is the most viable solution for many women.
For women without a current desire to have children, hormonal contraception with the pill, patch or vaginal ring is also an option. However, there is also estrogen withdrawal after 21 days for abortion bleeding to occur. Studies have shown that hormonal contraceptives work best against migraine attacks when patients become amenorrheic. Amenorrhea can be achieved with an IUD, depot injections, or continuous use of contraceptives (without abortion bleeding). In patients suffering from migraine with aura, hormonal contraceptives are contraindicated with the indication of contraception, but not with the indication of migraine prophylaxis. However, patients must be informed about the increased risk of stroke – which is, however, very low even under contraception.
Source: Annual Meeting of the Swiss Neurological Society, October 29-30, 2015, Bern.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(1): 40-41.