Jochen Rosenfeld, MD, Head of the Department of Hearing, Speech and Voice Medicine at the Ear, Nose and Throat Clinic, Cantonal Hospital St. Gallen, answers questions about dysphagia in an interview with HAUSARZT PRAXIS. How often and especially when do they occur? Which age groups are particularly affected and what is the diagnosis and treatment process?
Dr. Rosenfeld, how often are neurological disorders responsible for dysphagia and what are the most significant clinical pictures to be aware of in this context?
Dr. Rosenfeld:
Neurological disorders are among the most common causes of dysphagia. The most common neurogenic cause is stroke, which is associated with dysphagia in over 50% of cases in the acute phase. Dysphagia may be among the symptoms of traumatic brain injury and many neurodegenerative diseases such as multiple sclerosis, amyotrophic lateral sclerosis, or Parkinson’s disease. Dementia, which has increased significantly in recent years, is also associated with swallowing disorders.
Which age groups are most affected by swallowing disorders in terms of numbers?
Dysphagia is primarily a disease of old age and is relatively common overall. In neonates, rare malformations or neurological disorders may cause dysphagia in the context of various disabilities. However, they are much less common in newborns and infants overall.
Are swallowing disorders common after tumor surgery and radiation in the area of the swallowing tract (mouth, throat/pharynx, larynx, esophagus)?
Tumor therapy-related dysphagia is the most common dysphagia after neurologically related dysphagia. The severity of dysphagia depends, among other things, on the location of the tumor, the extent of the surgical intervention, the surgical method and any reconstructive measures. A major cause of dysphagia in these patients is the effects of radiation and chemotherapy.
Are psychological conditions such as depression also associated with dysphagia?
A foreign body sensation in the throat in the sense of a so-called globus pharyngeus is relatively common, but is not accompanied by an actual dysphagia. Psychogenic dysphagia is rather rare and mostly occurs in the context of eating disorders. Many antidepressant medications have a side effect of dry mouth, which in turn can lead to dysphagia.
What complications are particularly important to keep in mind in direct relation to dysphagia (e.g., aspiration pneumonia)?
Aspiration is the most threatening complication of dysphagia, in which fluid or food passes through the vocal fold plane into the deep airway. This can result in bronchial or pulmonary changes and even life-threatening pneumonia. For example, after stroke, aspiration-related pneumonia is the most common cause of death. Overall, however, dysphagia in particular, which develops insidiously, can lead to malnutrition or malnutrition with significant weight and strength loss. A larger bolus of food swallowed directly into the deeper airways can cause shortness of breath and choking, especially in children.
Because of the concomitant diseases and the variety of possible causes, a multidisciplinary approach must be taken in the diagnosis. Which specialists usually work together diagnostically?
At a minimum, a multidisciplinary dysphagia team includes otolaryngologists, neurologists, gastroenterologists, radiologists, speech therapists, and dietitians.
What role do apparative methods such as Functional Endoscopic Evaluation of Swallowing (FEES) or video fluoroscopy play in diagnostics?
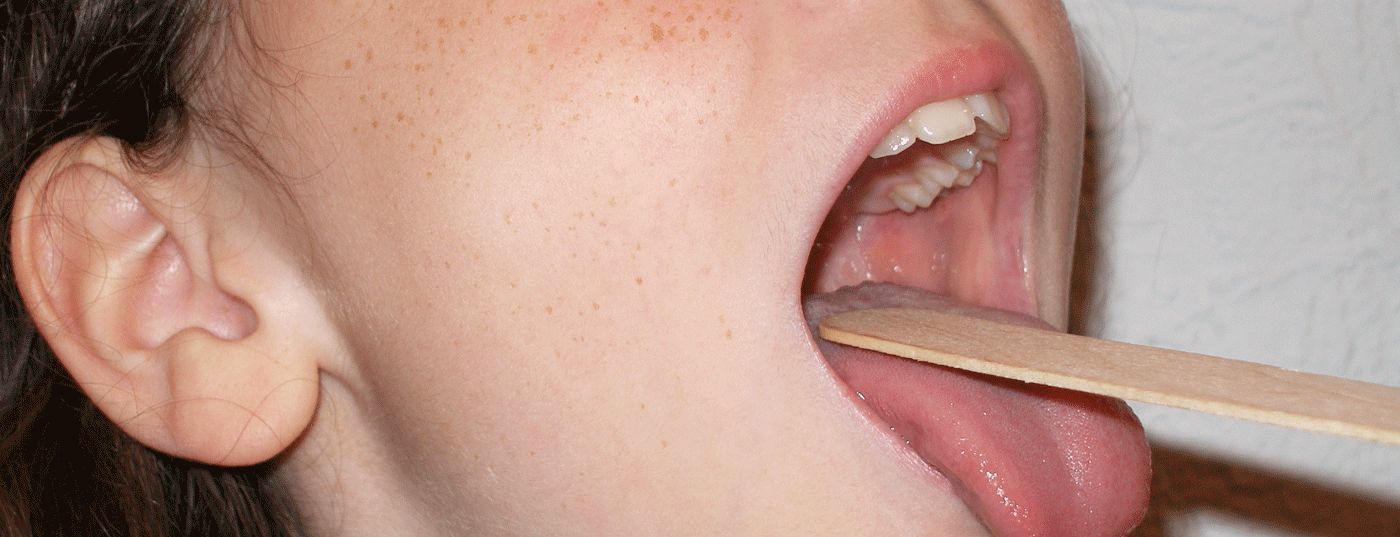
Functional Endoscopic Evaluation of Swallowing (FEES) has established itself as a standard method for diagnosis and therapy evaluation. It is now part of the basic examination of every patient with suspected dysphagia. Video fluoroscopy supplements swallowing diagnostics with the lower esophageal tract, but is not available everywhere, is technically complex, and involves radiation exposure.
Regarding therapy: What behavioral therapy, surgical and medicinal measures are currently available, especially in connection with the various causes and manifestations of dysphagia?
Functional dysphagia therapy (FDT) is the preferred method of treatment for dysphagia. Their implementation is primarily subject to speech therapy or speech therapy professions. Surgical measures are used, for example, to treat the underlying disease, to treat structural changes (e.g. tumors or diverticula in the area of the esophageal tract), or to ensure breathing and nutrition through tracheostomy and percutaneous tube placement (PEG). Medications are usually used to treat the often underlying neurological conditions and thus have a positive effect on swallowing.
What about the scientific evidence for each treatment intervention?
FDT is oriented towards a function- and problem-oriented approach. It is largely based on methods whose effectiveness has been proven or is at least probable according to pathophysiological considerations. The efficacy of drugs must first be proven in clinical trials before they can be approved or financed on the open market.
Interview: Andreas Grossmann
HAUSARZT PRAXIS 2014; 9(6): 8