Depression is probably no more common in older people than in younger people. However, there are differences in terms of symptomatology, diagnosis and treatment of depression. Often depressive symptoms are misjudged as normal accompanying symptoms in old age and therefore often remain untreated. Depression in the elderly is a condition that can be successfully treated with the help of psychotropic drugs and psychotherapy.
Along with dementia, depressive disorders are among the most common mental illnesses in older people. Stress factors in advancing age, such as the decline in performance, the loss of social roles and competencies, and the loss of a partner, often form the starting point for depressive disorders in older people. It is characteristic of depression in old age that several predisposing and triggering factors accumulate and at the same time compensatory possibilities such as occupation and leisure activities are missing.
Symptomatology of depression in old age
The main symptoms of depression according to ICD-10 (depressed mood, loss of interest and pleasure, reduced drive/fatigability) occur in older people as well as in younger people, regardless of etiological classification. However, the psychological, physical, and social conditions of the aging individual usually result in a different clinical presentation of depression compared with younger, depressed patients (Table 1).
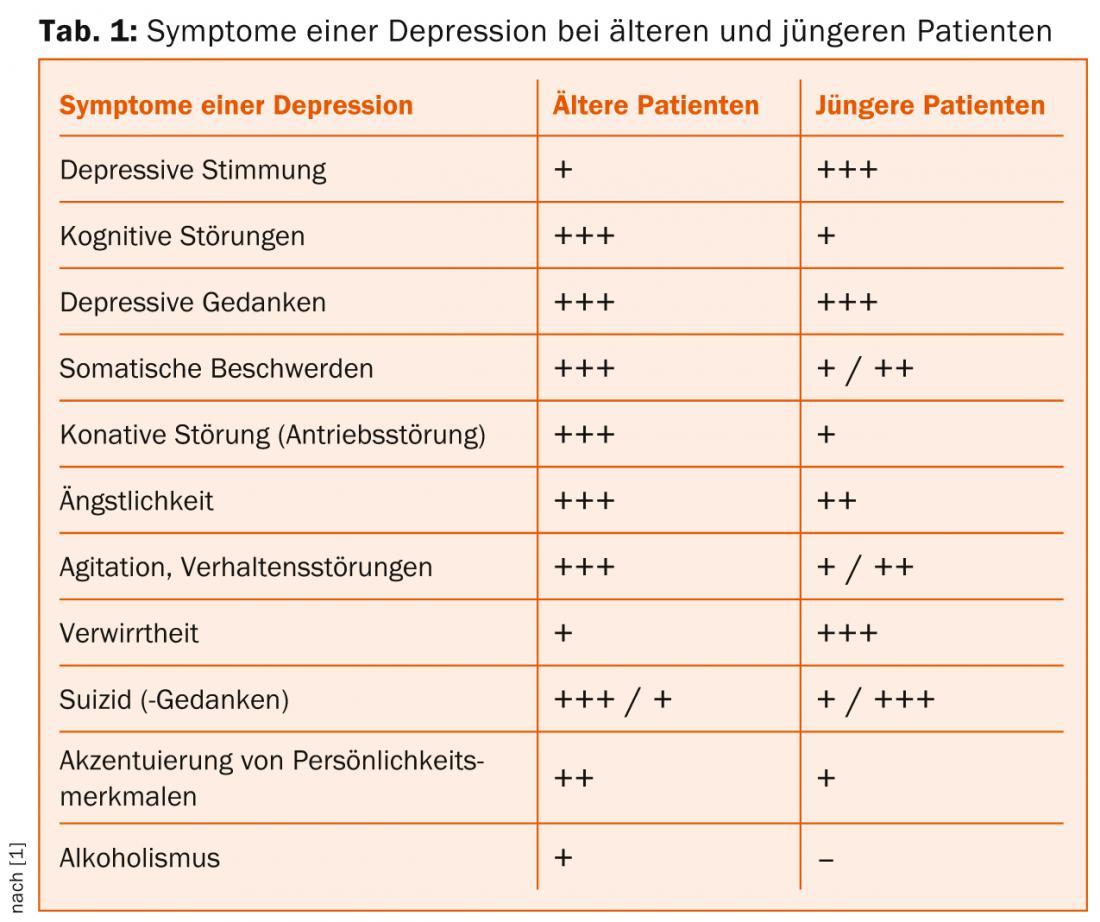
The focus is not necessarily on a depressed mood or dejection, but on complaining about body-related symptoms, which are often also misinterpreted, trivialization of one’s own feelings, anxiety, the occurrence of late alcoholism or suicidal ideation. The symptomatology of old-age depression leads to a diagnostically difficult situation, since the symptoms are often classified by the patient’s environment as “normal” and corresponding to age.
Old age depression vs. dementia
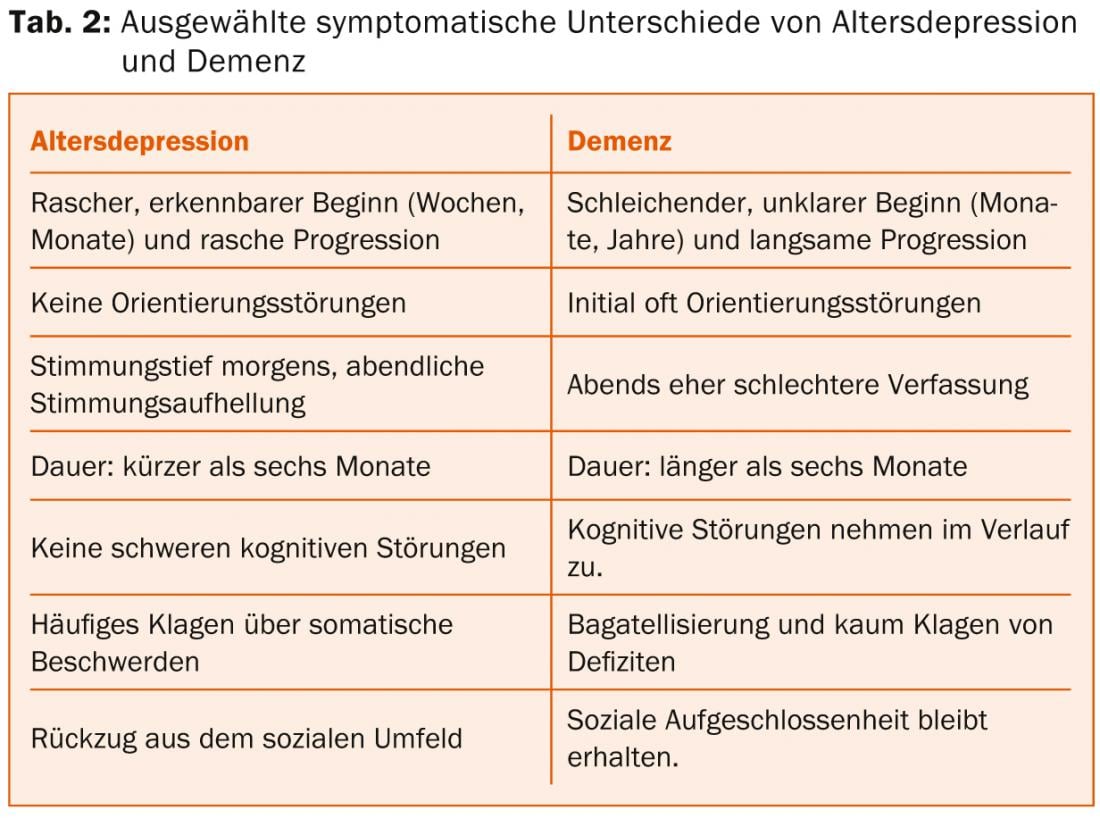
Especially in the initial phase of dementia, depressive moods can often be observed in the patient, as the patient perceives the gradual onset of the disease and the associated, increasing limitations. This awareness of incipient dementia may trigger a reactive depressive episode with suicidal risk in the patient. Therefore, it is important to rule out depression when dementia is suspected. Conversely, depressed patients may experience cognitive impairment, such as forgetfulness and memory impairment. Table 2 shows a comparison of selected findings to differentiate the two partially overlapping diseases.
Therapy of old age depression
For the treatment of old-age depression, a combined therapy is recommended, which takes into account pharmacotherapeutic treatment (antidepressant) and psychotherapeutic procedures (e.g., cognitive behavioral therapy and interpersonal psychotherapy). In this respect, the treatment of geriatric depression is not fundamentally different from the treatment of depressive disorders in younger patients. However, pharmacotherapeutic treatment places greater demands on the treating physician compared to younger patients, as comorbidities, impaired organ function, and possible interactions with other medications must be considered in the choice of therapeutic agent.
How to find the right antidepressant?
This question is important because not all patients respond and react equally well to every antidepressant. Success rates with respect to the first prescribed medication are about two-thirds for mild to moderate depression and much lower for severe depression, at about 50%. To date, a truly accurate selection of an antidepressant for a particular patient is not possible. The following criteria have proven most effective:
- Psychopathological symptoms
- Treatment history
- Reasonable side effects.
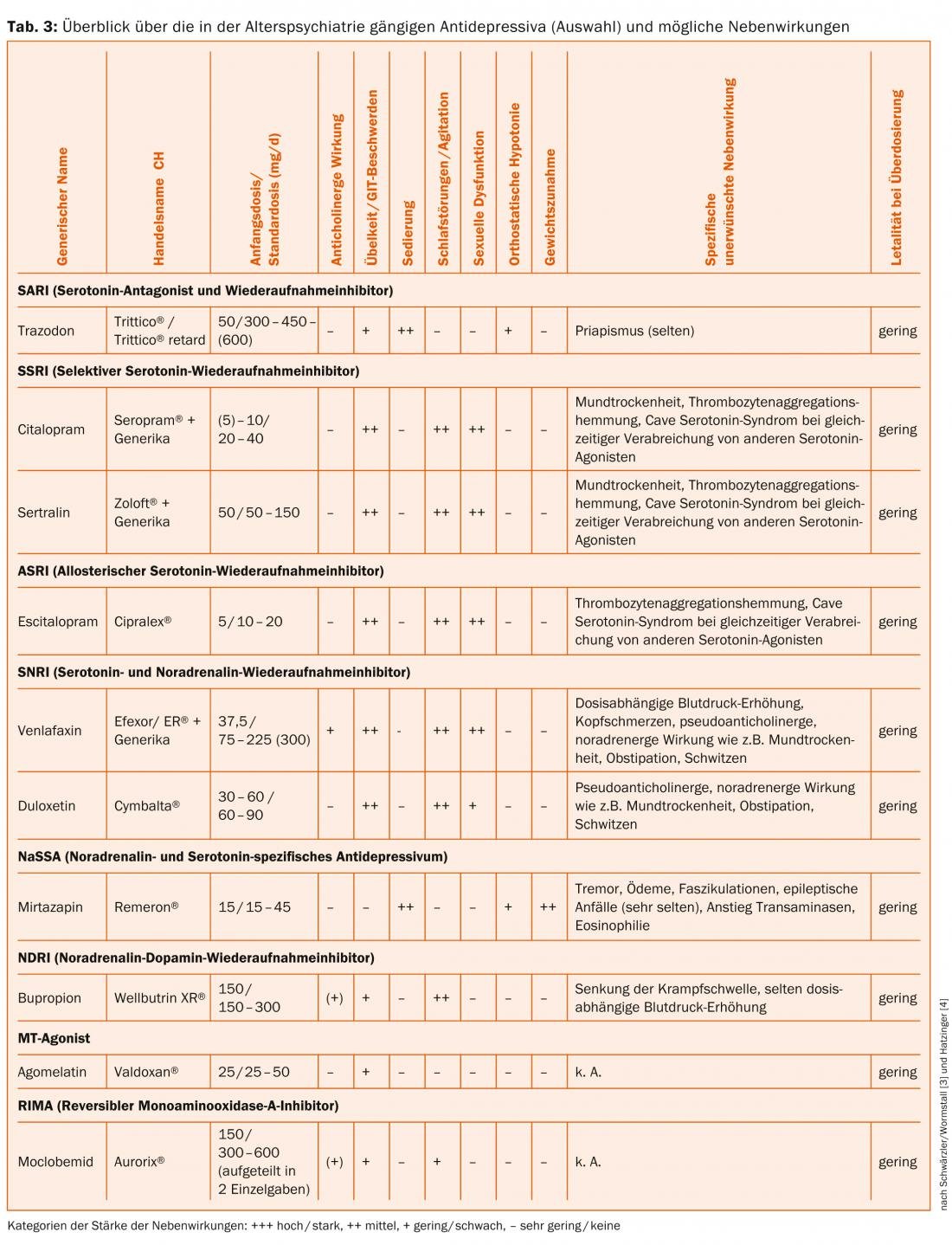
Table 3 provides an overview of antidepressants commonly used in geriatric psychiatry and their underlying, potential side effects.
When administering an antidepressant to treat depression, the basic rule is to “start slow – go slow,” and generally with half the usual starting dosage. The duration of treatment in the acute phase is four to six weeks at the recommended dose, although the effect of the antidepressant is rather rare in the first few days of treatment. The patient should be informed about this by the treating physician so that therapy discontinuations in case of alleged ineffectiveness can be avoided. Should no relevant therapeutic effect occur after an appropriate time and in sufficient dosage:
- Be prescribed an antidepressant from the same or a different pharmacological group.
- In cases of treatment resistance, consider a combination treatment of two antidepressants of different classes.
- Consider augmentation treatment (antidepressant with lithium, antidepressant with atypical antipsychotics, antidepressant with valproate or lamotrigine).
- Non-pharmacological interventions (sleep deprivation, ECT, light therapy) should be considered.
The goal of therapy is complete remission, which can usually be achieved within a longer period of time (between 6 months to 1.5 years).
Harald Gregor, MD
Prof. Dr. med. Armin von Gunten
Literature:
- Adapted from Clément JP: La dépression de l’âge avancé. Dans: Giannakopoulos et Gaillard. Abrégé de psychiatrie de l’âge avancé. Médecins et Hygiène 2010; 171-183.
- Wolfersdorf M, Schüler M: Depression in old age. Verlag W. Kohlhammer 2005 Stuttgart.
- Schwärzler F, Wormstall H: The depression of the elderly. Ars Medici Dossier 2009; IX.
- Hatzinger M: Affective disorders in old age. Swiss Archives of Neurology and Psychiatry 2011; 162(5): 179-189.
- The survey was conducted by Vifor Pharma AG and Fluentis GmbH as part of training events in 2013.
- World Health Organization (WHO) Department of Mental Health: Lausanne Technical Consensus Statements on Psychiatry of the Elderly. 1999 Geneva.
InFo Neurology & Psychiatry 2014; 12(1): 25-29.
HAUSARZT PRAXIS 2014; 1(9): 39-43