Patients suffering from schizophrenia experience profound changes in perception, thinking and behavior [1]. These often lead to significant limitations in quality of life and everyday function [2]. The disorder often begins in adolescence and young adulthood, impacting crucial developmental tasks such as education, peer interaction, and partner relationships. Early diagnosis is therefore of crucial importance for the further course of the disease [3]. This article describes the symptoms of schizophrenic psychosis and the procedure for diagnosis.
Symptoms of schizophrenic disorders can be assigned to several symptom dimensions (Table 1) [1]. For diagnostic purposes, the so-called positive symptoms are currently evaluated most strongly. These include hallucinations, sensory perceptions without the presence of a sensory object. In schizophrenia, auditory hallucinations are most common, occurring primarily in the form of hearing voices. In this symptomatology, patients may, for example, receive commands or experience their actions being commented on. Another central phenomenon is delusion, which is defined as an objectively false belief to which the patient holds with uncorrectable certainty. The most common of these are relationship delusions and persecution delusions.
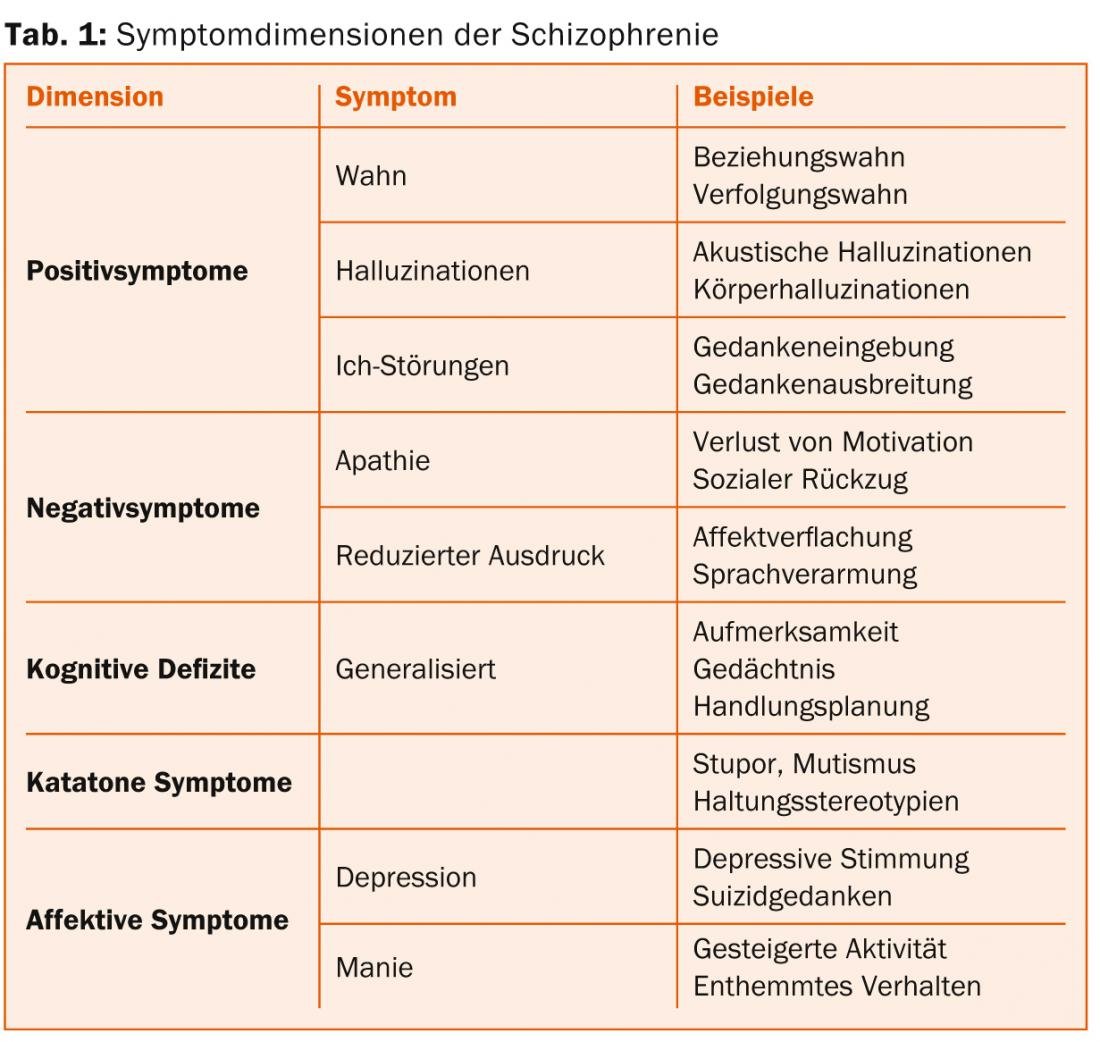
Negative symptoms refer to the loss of healthy psychological functions; they are reflected in reduced drive, social withdrawal, joylessness, reduced expression, and impoverishment of speech. In addition, patients with schizophrenia often have cognitive impairments that affect all areas of functioning, such as attention, memory, or action planning. Negative symptoms and cognitive deficits have gained increasing attention in recent years because they are highly predictive of patients’ daily functioning.
Catatonic symptoms involve psychomotor phenomena, such as mutism, stupor, and postural stereotypies. In addition to these core dimensions of schizophrenia, affective symptoms are also significantly more common in patients with schizophrenia than in the general population. Therefore, it has been suggested that depression and mania should also be defined as symptom dimensions.
ICD-10 criteria for schizophrenia
In the current ICD-10 catalog, schizophrenia is defined in category F20 (Table 2) [4]. As can be seen from the table, certain positive symptoms are considered to be of particular importance for the diagnosis. This has been criticized in the past and has led to a more balanced consideration of all symptom dimensions of schizophrenia in the new American diagnostic system DSM-V, which will also be reflected in the future ICD-11 [5].
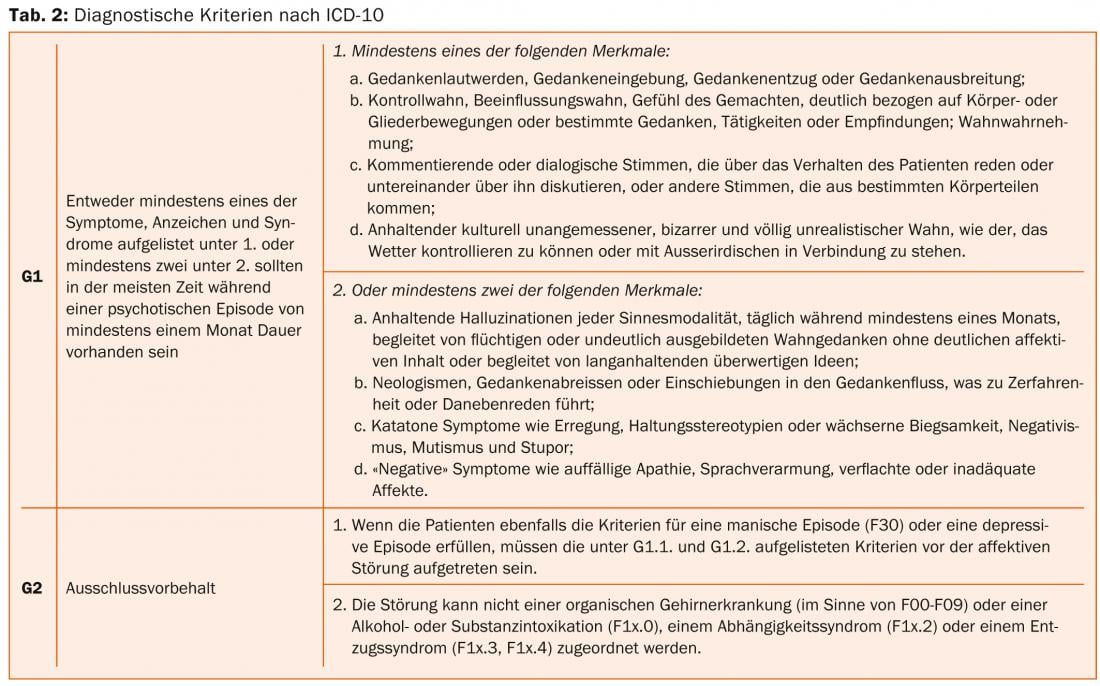
Currently, it is possible to differentiate subtypes of the disease, such as paranoid, hebephrenic or catatonic schizophrenia, depending on the dominant symptoms, when making a diagnosis according to ICD-10. This subtype classification is no longer found in DSM-V due to the lack of stability in the course of the disease and the unclear clinical relevance, which is also to be expected in ICD-11.
Differentiation from other mental illnesses
When making a diagnosis, schizophrenia must be distinguished from other mental illnesses with positive symptoms. Affective disorders are the first to be mentioned here. Psychotic symptoms can occur in both depression and mania, but only in severe affective disorders and then usually with so-called mood-congruent symptoms such as delusions of guilt in depression. In patients who meet criteria for both schizophrenia and affective disorder, there is also the possibility of diagnosing schizoaffective disorder.
A very important diagnostic category is the group of acute psychotic disorders. Many patients who come to treatment for the first time with psychotic symptoms do not meet the criteria for schizophrenia. In addition to the symptoms, the time criterion of one month is also decisive. The further course of acute psychotic disorders is very heterogeneous [6]. Important predictors of a favorable course are acuity of onset and complete remission of symptoms.
Differentiation from substance-induced psychotic disorders.
The classification of psychotic symptoms in patients with substance use is a major challenge [7]. Today, more than 50% of patients with a first episode of psychosis have a substance disorder, and the question here is often whether the psychotic symptoms are substance-induced. For example, an onset of symptoms before substance use or persistence of symptoms after cessation of substance use for more than one month argue against a substance-induced disorder. But even these and other criteria for differentiation often do not allow a clear causal assignment. One of the results of this is that after one year, more than 25% of patients with a substance-induced psychotic disorder receive another diagnosis – often that of schizophrenia.
Exclusion of somatic diseases
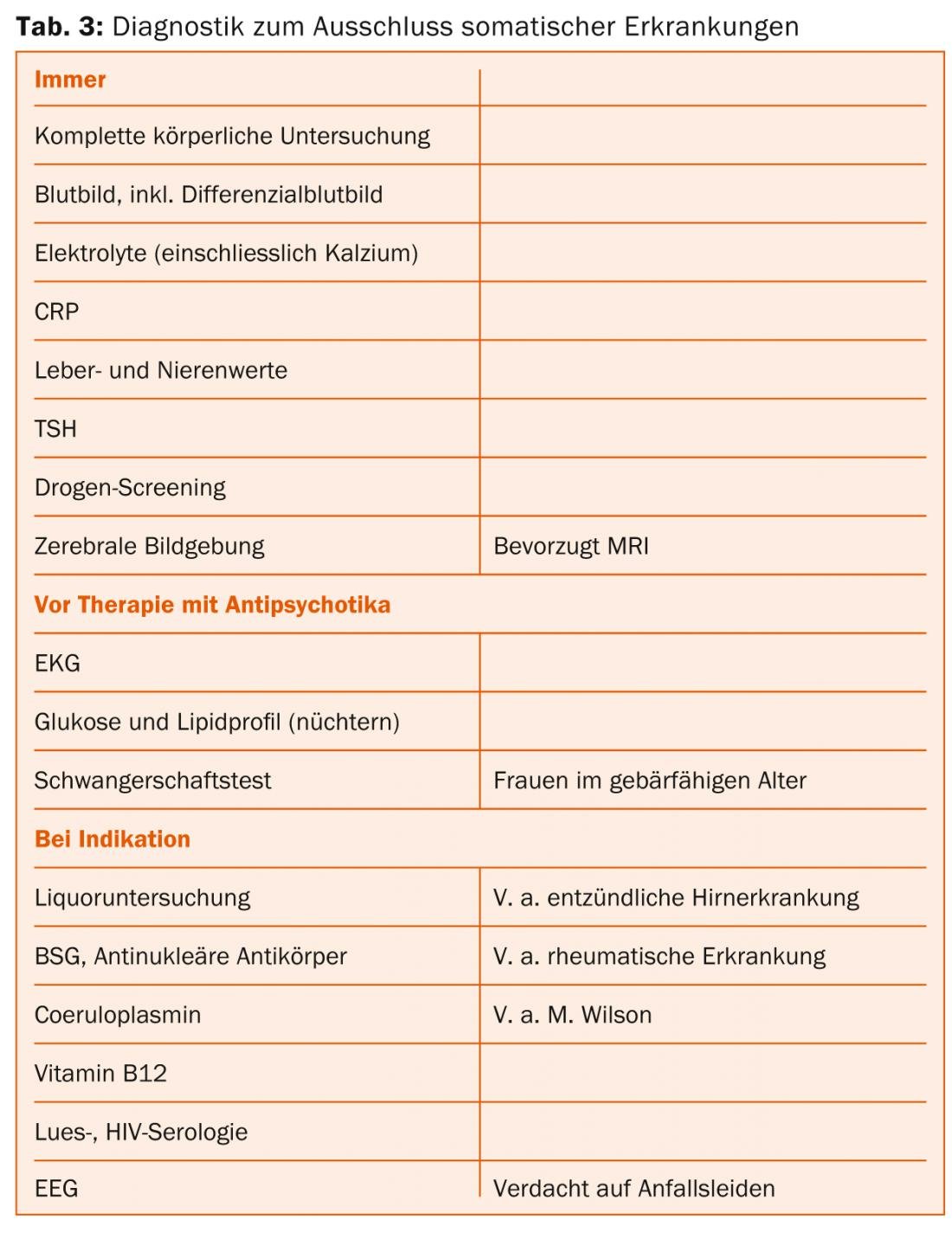
Symptoms of schizophrenia can be caused by a wide variety of neurological and internal diseases. Clinically relevant somatic diseases are found in about 8% of patients with an initial manifestation, without these always being causally responsible for the mental symptoms [8]. Therefore, both a thorough exclusion diagnosis and adequate treatment of somatic comorbidities are essential.
The examinations proposed in Table 3 are based on the guidelines of the German Society of Psychiatry, Psychotherapy and Neurology [9]. In young adults with an initial manifestation of psychotic illness, the most common organic causes come from the area of inflammatory diseases of the central nervous system.
Importance of early diagnosis
Duration of untreated psychosis (DUP) refers to the time between the first onset of psychotic symptoms and the first specific treatment [3]. It is now proven beyond doubt that a longer duration of untreated psychosis is associated with a worse course. Efforts to shorten this interval require intensive collaboration between very different professional groups, such as general practitioners, specialists, social counselors, teachers, and school psychologists [10]. General practitioners (and physicians in other specialties) are not infrequently the first contacts for patients with schizophrenic psychosis and can make a significant contribution to early diagnosis. They also play an important role in the further course, especially since somatic diseases, such as cardiovascular diseases, are significantly more frequent in patients with schizophrenia than in the general population.
Psychiatric specialists and clinics have the task of ensuring the earliest possible comprehensive diagnosis and treatment. In addition, educating and informing the public about the disease is an important measure for early detection.
In summary, it should be emphasized that for the diagnosis and, in particular, the treatment of patients with initial manifestations of schizophrenia, good networking of the various partners in the health care system in the sense of integrated care is of central importance.
Summary
Patients suffering from schizophrenia may exhibit a wide range of symptoms. These include positive symptoms (delusions and hallucinations), negative symptoms (apathy and reduced expression), cognitive deficits, psychomotor abnormalities, and affective symptoms. In the current diagnostic criteria, it is mainly the positive symptoms that are used to make the diagnosis. Differential diagnoses include affective disorders with psychotic symptoms, acute psychotic disorders, and substance-induced psychotic disorders. In addition, the exclusion of organic causes is of great importance. Early diagnosis and treatment can contribute to a favorable course of the disease.
PD Stefan Kaiser, MD
Matthias Kirschner, MD
Literature:
- van Os J, Kapur S: Schizophrenia. Lancet 2009; 374: 635-645.
- Mueser KT, McGurk SR: Schizophrenia. Lancet 2004; 363: 2063-72.
- Perkins DO, et al: Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. The American Journal of Psychiatry 2005; 162: 1785-804.
- Freyberger HJ, Dilling H: Pocket guide to the ICD-10 classification of mental disorders. Hans Huber 2012.
- Tandon R: Schizophrenia and other psychotic disorders in DSM-5. Clinical Schizophrenia & Related Psychoses 2013; 7: 16-9.
- Mojtabai R, et al: Clinical characteristics, 4-year course, and DSM-IV classification of patients with nonaffective acute remitting psychosis. The American Journal of Psychiatry 2003; 160: 2108-15.
- Mathias S, et al: Substance-induced psychosis: a diagnostic conundrum. The Journal of Clinical Psychiatry 2008; 69: 358-67.
- Freudenreich O, et al: Initial medical work-up of first-episode psychosis: a conceptual review. Early Intervention in Psychiatry 2009; 3: 10-8.
- German Society for Psychiatry, Psychotherapy and Neurology. Schizophrenia treatment guideline. Steinkopff 2006.
- Hegelstad WT, et al: Long-term follow-up of the TIPS early detection in psychosis study: effects on 10-year outcome. The American Journal of Psychiatry 2012; 169: 374-80.
InFo Neurology & Psychiatry 2014; 12(1): 4-7.











