Introduction: Primary CNS lymphomas, predominantly of the B-cell type, are rare tumors with a peak incidence in middle to older age. Conventional MRI examination yields essentially nonspecific findings of a mostly KM-receiving, typically ventricle-proximal mass. The value of advanced MRI diagnosis and MRI-guided biopsy is presented in the following case report.
Case report: A 21-year-old male patient had a slowly progressive left hemiparesis. An evaluative MRI showed a right-sided contrast-enhancing lesion centered in the thalamus. A cerebrospinal fluid (CSF) puncture revealed unremarkable findings. There was no evidence of immunodeficiency either anamnestically or on the basis of laboratory diagnostics. Neurofibromatosis 1 (NF1) without neurological manifestation had been diagnosed about ten years earlier. The hemiparesis had significantly improved after low cortisone administration and the patient was subsequently repatriated.
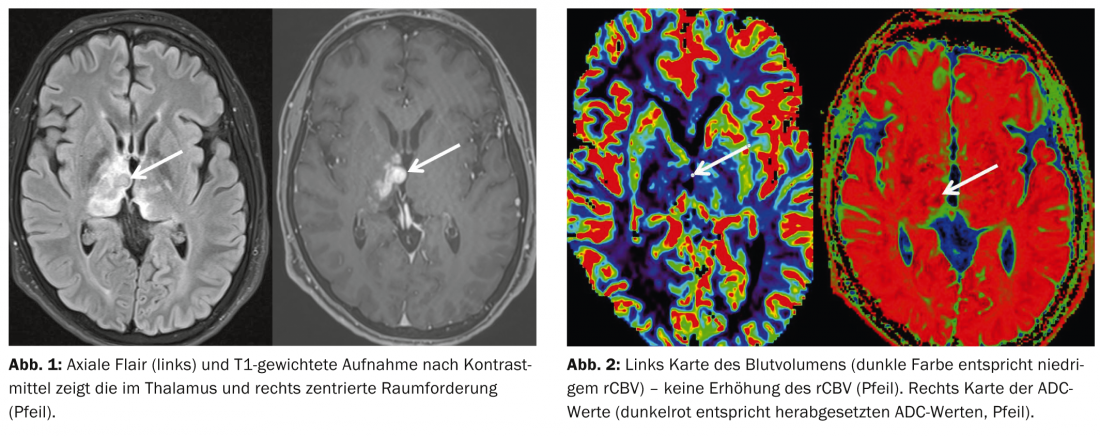
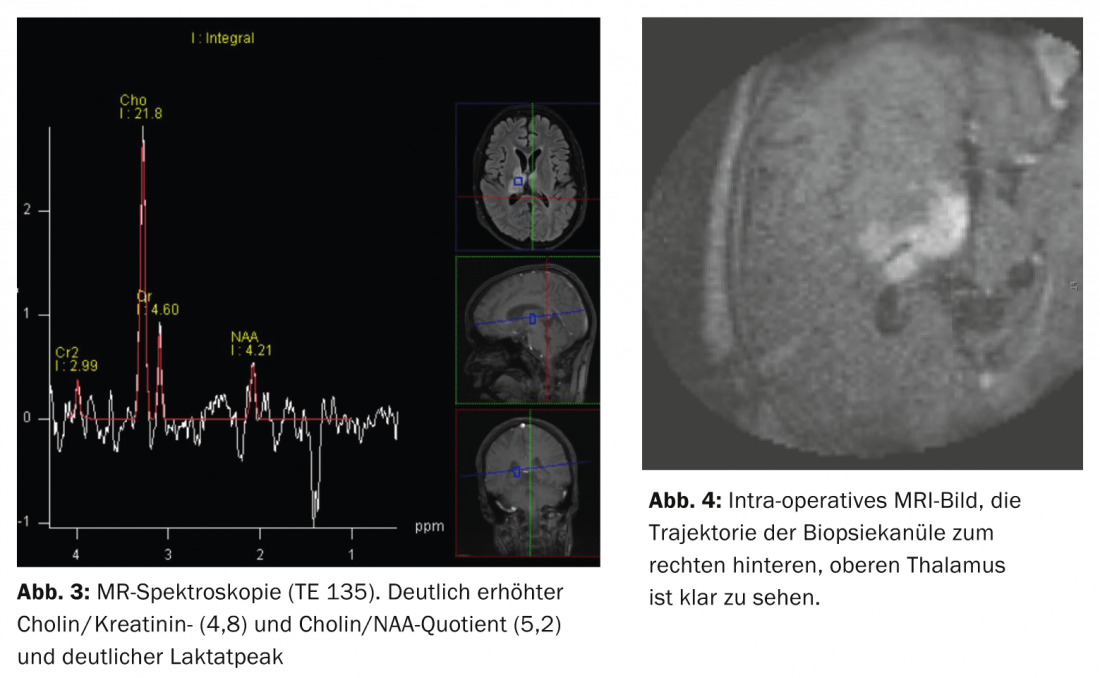
On admission, persistent left-sided hemisymptomatology was the leading symptom. On T2/FLAIR-weighted images, the lesion was inhomogeneous with clearly hypointense/isointense portions centrally (fig. 1). Relative cerebral blood volume was not increased in a side-to-side comparison, and ADC values were significantly decreased in some cases (Fig. 2) .
Spectroscopy showed a markedly increased choline/creatinine (4.8) and choline/NAA (5.2) quotients and a clear lactate peak (Fig.3). Due to the location of the lesion, but especially due to the results of the extended MR diagnostics, a primary CNS lymphoma had to be assumed in this case, especially after PET-CT showed no evidence of systemic involvement.
The tentative diagnosis was confirmed by stereotactic biopsy performed on intra-operative MRI (Polestar, Medtronic). The bioptic trajectory reached the contrast-receiving areas of the posterior superior thalamus from the right parietal side bypassing the visual radiation. Neurological deficits did not occur (Fig. 4). The histological diagnosis was aggressive B-cell non-Hodgkin lymphoma (Mib1 [Ki67] proliferation index 92-98%).
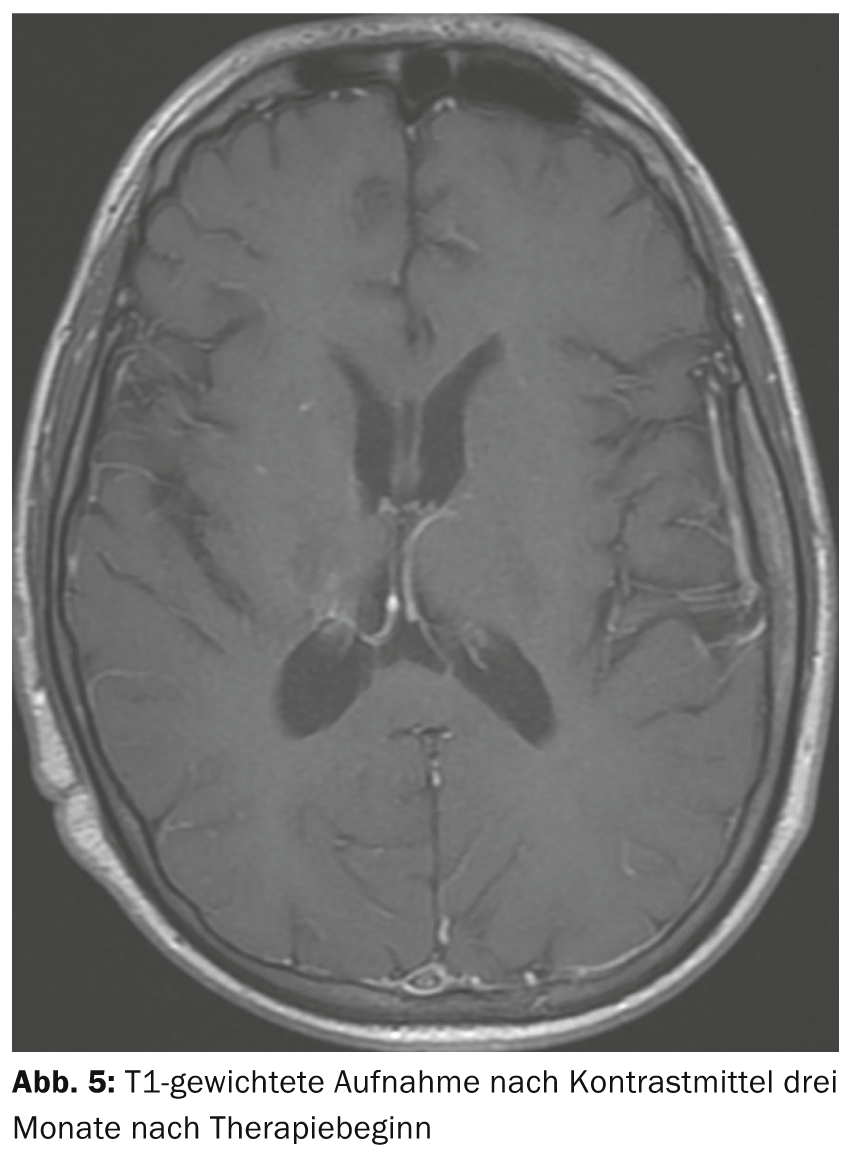
Immunochemotherapy consisting of the combination of high-dose cytosine arabinoside and high-dose methotrexate was started in analogy to the IELSG PCNSL trial [1]. Due to strong CD20 antigen expression, rituximab (375 mg/m2, day 1) was also used. The patient showed improvement in his left-sided hemiparesis already during the first cycle of therapy. A follow-up MRI three months after the start of therapy showed hardly any contrast-absorbing areas (Fig. 5).
Discussion: Primary CNS lymphoma is a rare tumor entity (approximately 2-5% of all intracranial tumors), and its incidence has also been decreasing in HIV-positive patients since the introduction of antiretroviral therapy. Our patient has special features with regard to the typical characteristics of the disease: He is young and did not show any neuropsychological abnormalities clinically, but only a spastic hemiparesis on the left side. With regard to NF1 known in the patient, no association with the occurrence of CNS lymphoma is certain; only very isolated case reports exist in this regard.
MR imaging was typical of primary CNS lymphoma based on lesion location and signal characteristics. Other focal contrast-absorbing pathologies to be considered for differential diagnosis were extremely unlikely, especially also due to the enhanced MRI imaging with decreased ADC values and lack of blood volume increase. Nevertheless, at least at the present time, a histologically established diagnosis is a prerequisite for chemotherapy or radiotherapy.
Because of the deep brain structures frequently involved, as in this case, a stereotactic guided biopsy is usually the best method for obtaining a tissue sample. We performed the biopsy using intra-operative MRI [2]. In contrast to biopsy based purely on pre-operative MRI data, intra-operative imaging virtually eliminates the risk of mislocation of the biopsy needle, making it possible to safely reach the target area and accurately verify the position of the biopsy needle intra-operatively
Fortunately, the patient responded rapidly to immunochemotherapy. Because of the young age, if complete or partial remission is achieved after completion of four cycles of chemotherapy, consolidative whole-brain irradiation should be omitted due to neurotoxicity and high-dose therapy with autologous stem cell replacement should be performed. Assessment of cure rates is difficult: according to the literature, long-term remissions are seen in 30-40% of all patients after high-dose methotrexate/cytosine anabaside. The value of rituximab has not yet been clearly established, but in individual studies it achieves an approximately ten percent gain in long-term remissions. The first results of phase II studies of consolidating high-dose therapy with stem cell transplantation show long-term remissions of up to 70%, but the follow-up periods of these studies are still too short to make reliable statements regarding the long-term chances of remission or cure.
PD Dr. med. Ralf A. Kockro
Achim Mallmann, MD
Prof. Dr. med. Christoph Renner
Prof. Dr. med. Stephan G. Wetzel
Literature:
- Ferreri AJ, et al: International Extranodal Lymphoma Study Group (IELSG). High-dose cytarabine plus high-dose methotrexate versus high-dose methotrexate alone in patients with primary CNS lymphoma: a randomised phase 2 trial. Lancet 2009 31; 374(9700): 1512-1520.
- Quinn J, Spiro D, Schulder M: Stereotactic Brain Biopsy With a Low-Field Intraoperative Magnetic Resonance Imager. Neurosurgery 2011; 68(1 Suppl Operative): 217-224.
- Schlegel U, Thiel E: Primary CNS lymphomas. In: Commission “Guidelines” of the German Society of Neurology, Diener HC, Weimar C (eds.): Guidelines for Diagnostics and Therapy in Neurology. Thieme Verlag Stuttgart, September 2012.
InFo Neurology & Psychiatry 2014; 12(1): 14-16.
InFo Oncology & Hematology 2014; 2(2): 8-10.











