Since the human skin produces vitamin D only when exposed to sunlight and food is an insufficient alternative source, a majority of the Swiss population is undersupplied during the winter months, according to the Swiss Federal Office of Public Health. In some cases, this results in bone disease. What are the ways to diagnose vitamin D insufficiency and how can it be avoided?
Vitamin D is a fat-soluble vitamin with hormone character, which is formed in the human skin under sunlight (especially UVB). It regulates calcium and phosphate absorption from the intestine and their incorporation into the bones. Thus, it is an important component of healthy bone and tooth formation [1, 2]. In the summer months, 20-30 minutes of sun exposure is enough to produce enough vitamin D in your own body. The vast majority (80%) of the Swiss population is thus sufficiently supplied [2–4].
However, since the number of sunshine hours in winter (November to April) is significantly lower and the body’s own storage possibilities are limited, an undersupply (<50 nmol/l) is to be expected in 60% of Swiss people during these months [4]. The 25(OH)D level sometimes falls to 20 nmol/l (severe deficiency <25 nmol/l) [5]. Possible consequences are bone diseases: rickets in children, osteomalacia in adults [4].
Alternative sources can meet demand
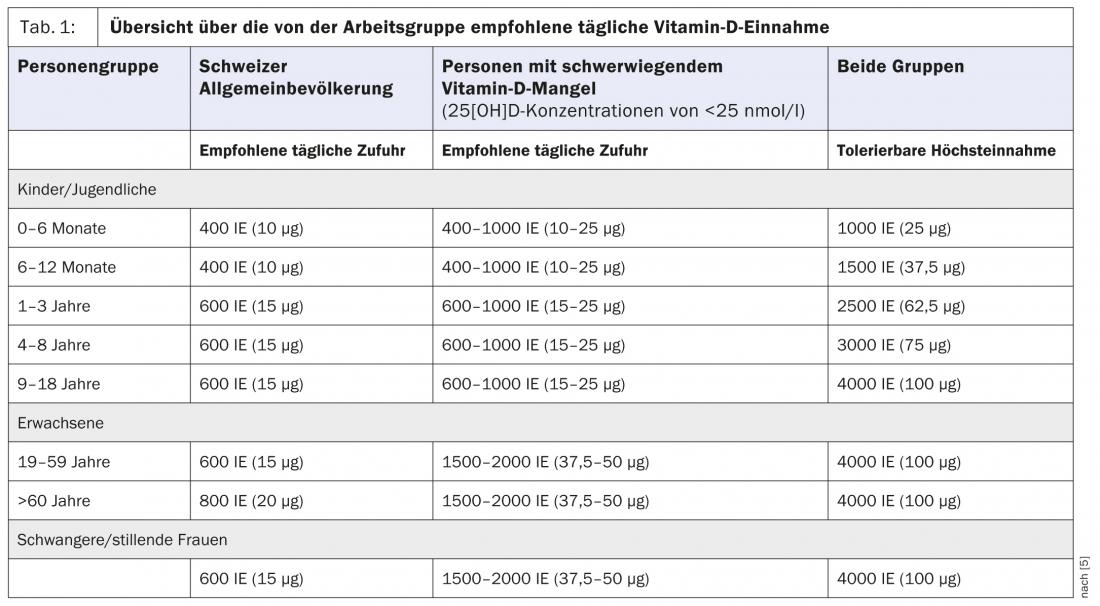
Because sun exposure poses risks and is an uncertain source due to the seasons, alternatives must be found. The body is hardly able to cover its vitamin D balance from everyday food, the amounts in it are too low. Potential sources such as fatty fish (up to 800 IU/100 g), fortified margarine (up to 300 IU/100 g), chicken eggs (up to 200 IU/100 g), or edible mushrooms (up to 340 IU/100 g) provide only part of the necessary vitamin D intake [3]. Table 1 shows a list of recommended daily doses for children, adults, the elderly, and pregnant women. It was published in March 2012 by a working group of the Swiss Federal Office of Public Health (SFOPH). The recommendations are largely consistent with the Institute of Medicine (IOM), International Osteoporosis Foundation (IOF), and US Endocrine Society guidelines [5].
Due to low vitamin D levels in the diet, the widespread use of sunscreens, and insufficient sun exposure in winter, the working group therefore concludes that vitamin D supplementation in the form of drops or tablets is useful for many individuals [5]. The following risk factors in particular are indicative of an undersupply:
- Overweight and obesity (greater volume of distribution = less available 25-hydroxyvitamin D).
- Age (the body’s own vitamin D formation is reduced fourfold).
- Pregnancy and lactation without vitamin D supplements
- Darker skin type (stronger skin pigmentation leads to lower vitamin D production).
- taking certain medicines, such as cholesterol-lowering medicines, medicines for fungal infections or for seizures, cortisone
- Diseases such as chronic liver or kidney disease, inflammatory bowel disease such as celiac disease or Crohn’s disease [3, 6].
For precise clarification, the 25-hydroxyvitamin D concentration in the blood serum should be measured in risk groups [2, 6].
Health benefits of adequate intake
Current data confirm the FOPH’s recommendations: in the elderly population, a 25(OH)D threshold of 75 nmol/l prevents falls and fractures. 50 nmol/l is needed to support bone health in all adults and muscle health in the elderly. In contrast, more data are needed on bone and muscle health in children and adolescents and on the other non-skeletal effects of vitamin D for all age groups [5, 6]: Small clinical studies show a beneficial effect of vitamin D on myocardial infarction risk and blood pressure. In addition, there is initial evidence that the prevention of colorectal cancer, tuberculosis or multiple sclerosis as well as diabetes is favored by an adequate intake [2, 6].
“To ensure effective substitution, it would be desirable for consumers to have access to effective dietary supplements and fortified foods in retail stores, in addition to the vitamin D drops and tablets currently available in pharmacies and drugstores,” the working group concludes [5]. However, vitamin D oversupply due to uncontrolled intake of supplements should also be avoided; it leads to hypercalcemia and, in the worst case, can result in cardiac arrhythmias or kidney stones [1].
Literature:
- Federal Office of Public Health: Factsheet Vitamin D, Bern, June 2012.
- Bischoff-Ferrari H A, et al: Recommendations of the Swiss Federal Commission on Nutrition on vitamin D intake for the Swiss population. Schweiz Med Forum 2012; 12(40): 775-778.
- Federal Office of Public Health: Vitamin D recommendations of the Federal Office of Public Health FOPH, Bern, June 2012.
- Federal Office of Public Health: Vitamin D: Questions and Answers, Bern, June 2012.
- Federal Office of Public Health: Vitamin D deficiency: data situation, safety and recommendations for the Swiss population, Bern, March 2012.
- Bischoff-Ferrari, H A: Vitamin D. In old age, the “normal” supply is not sufficient. Ars Medici 2010; 14: 559-564.
HAUSARZT PRAXIS 2013; 8(11): 4











