The lower the better and better early than late – this is the strategy in LDL treatment. While a new hopeful substance for LDL reduction is in development with the antibody PCSK9, the HDL hypothesis has faltered.
Dyslipidemia treatment focuses primarily on reducing low-density lipoprotein (LDL) cholesterol. Depending on the risk group, the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) guidelines recommend an LDL of <1.8 mmol/l (70 mg/dl) in patients at very high risk, and in patients at high risk values of <100 mg/dl and moderate risk LDL levels of <3.0 mmol/l 115 mg/dl (Tab.1).

In addition to lifestyle-altering factors, pharmacological therapy with statins is of high importance in the treatment of dyslipidemia. Diverse studies have shown that statins can significantly reduce cardiovascular morbidity and mortality in both primary and secondary prevention. In contrast, the question of whether a threshold exists above which no positive effect of LDL treatment is detectable remained unanswered for a long time. An answer was now provided by a CTT meta-analysis of 14 trials of statins (Fig. 1) [1].
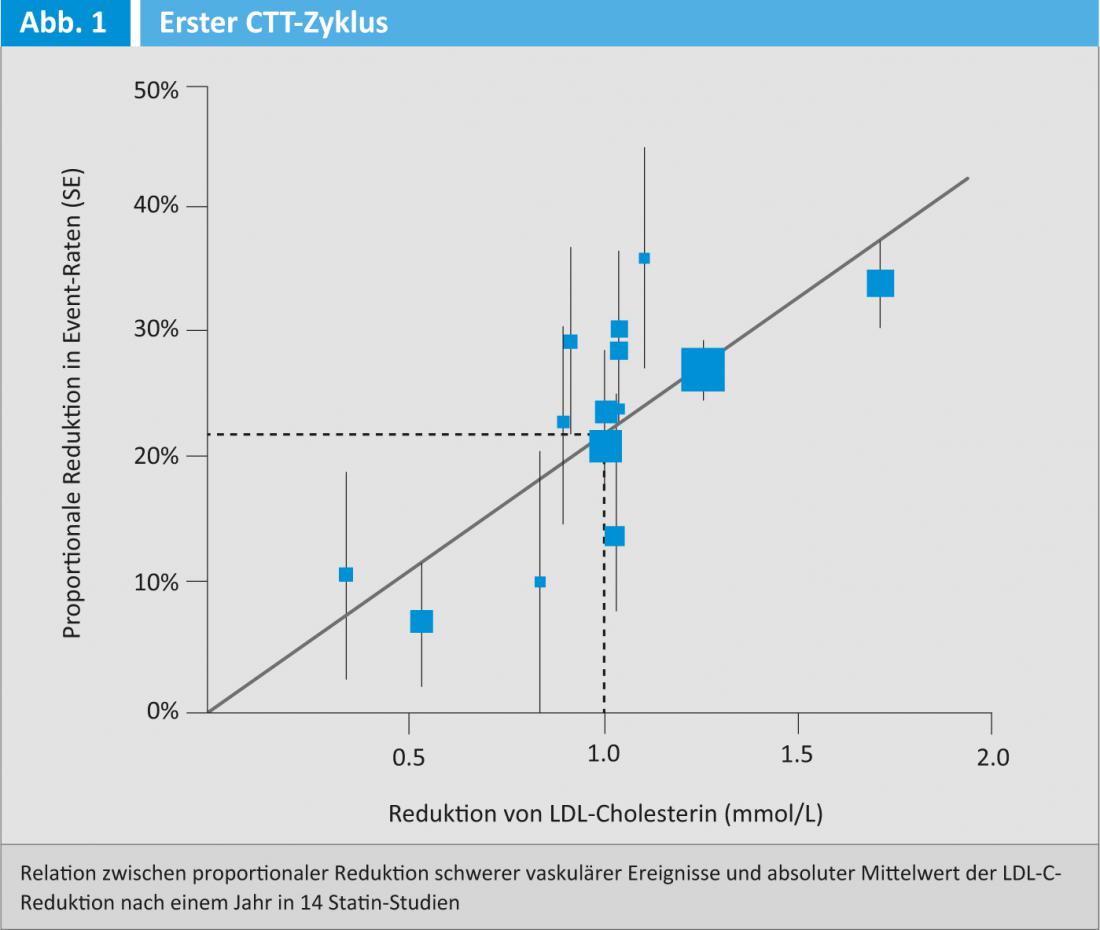
This had shown that for every LDL unit reduced by 1 mmol/l, the number of total deaths decreased by 12% annually and the number of deaths from CHD by as much as 19%. “This confirms the hypothesis of a linear relationship between LDL reduction and the decrease in cardiovascular events,” said Prof. John Chapman, MD, Hôpital de la Pitié, Paris, in Davos. “So the lower the LDL, the better!”
Early LDL lowering required
An advanced age as well as the presence of risk factors for many years often lead to the fact that the residual risk remains high despite the existing treatment options.
To find out what impact lifelong low LDL levels have on cardiovascular risk, Ference et al. a study of individuals who had different gene variants, each associated with low LDL [2]. The authors were able to show that the risk of coronary heart disease is three times lower if LDL cholesterol is lowered early in life. “So it’s no longer just the lower the better, but better early than late,” Prof. Chapman said.
Regarding the safety of statin treatment, the speaker pointed out that rhabdomyolysis is a dose-dependent and rather rare complication. In addition, a meta-analysis that showed a positive association between statin therapy and new-onset diabetes mellitus had recently caused uncertainty [3]. However, the risk of diabetes is considered low compared with the benefits of statin treatment.
HDL hypothesis remains unconfirmed
The high-density lipoprotein (HDL) hypothesis originated in epidemiological studies that showed an inverse relationship between the level of HDL and the incidence of coronary heart disease. In addition, a direct anti-atherogenic effect of HDL cholesterol was observed in studies with healthy subjects. “These results have led to the question of whether one should additionally raise HDL cholesterol in patients with an increased cardiovascular risk,” said Prof. Ulf Landmesser, MD, of the Cardiology Clinic at the University Hospital Zurich.
With the premature termination of the AIM-HIGH and HPS2-THRIVE trials with niacin, the HDL hypothesis is now shaken [4, 5]. “While the AIM-HIGH trial was too small to demonstrate an effect of niacin, the increased cardiovascular events in the HPS2-THRIVE trial may be due to the potentially pro-atherogenic properties of the prostaglandin receptor antagonist laropiprant,” Prof. Landmesser said. This substance was used to prevent the undesirable occurrence of “flushings” under niacin.
Another strategy to positively affect HDL cholesterol is to inhibit cholesterol transfer protein (CETP). This causes a reversal of cholesterol transport from the periphery to the liver, resulting in an increase in HDL cholesterol and a decrease in circulating LDL. Due to the increase in cardiovascular events as well as all-cause mortality, the study of the CETP inhibitor torcetrapib had to be stopped prematurely [6]. “We have believed for too many years that we can influence the occurrence of cardiovascular events by simply changing HDL cholesterol,” said Prof. Landmesser. One problem, he said, is that the HDL hypothesis is based mainly on studies with healthy subjects. Recent studies now show that the role of HDL depends strongly on whether a person is healthy or already has coronary heart disease. Against this background, the question of combined LDL and HDL treatment is likely to occupy the scientific community for some time to come.
New kid on the block: PCSK9
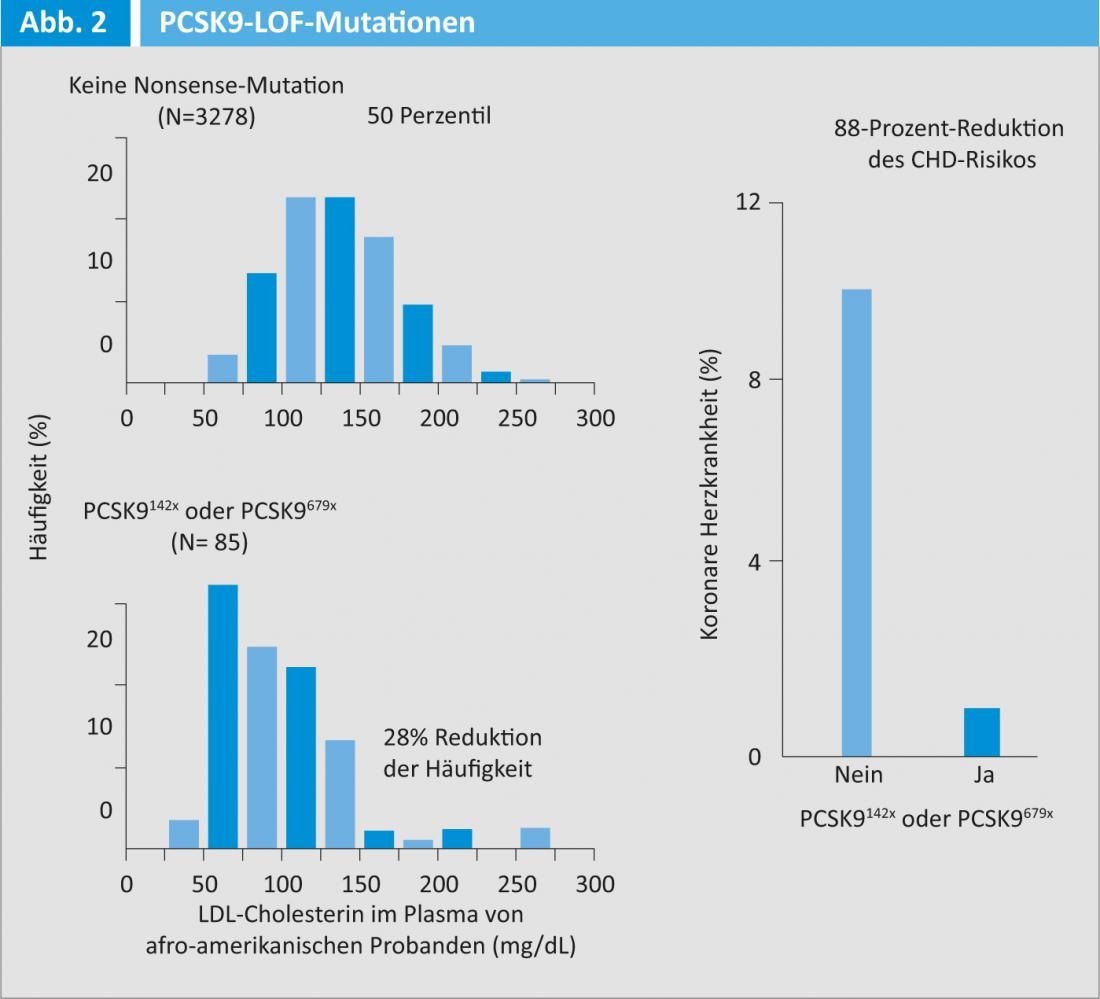
The accidental discovery that individuals with a mutation of the PCSK9 gene have significantly lower LDL cholesterol in their blood led to the development of a monoclonal antibody with the same name. PCSK9 is a glycoprotein secreted mainly in the liver. In mice, overexpression of PCSK9 led to a decrease in LDL receptors in the liver, which was reflected in an increase in LDL cholesterol in the blood. Conversely, the absence of PCSK9 was associated with an increase in LDL receptors as well as increased uptake of LDL from plasma. As shown in the ARI study, mean LDL cholesterol was reduced by 28% the risk of coronary heart disease by 88% in African-American individuals with a PCSK9 mutation (Fig. 2) [7].
The recently published results of a phase II study evaluating the monoclonal antibody at different doses (150, 200, and 300 mg) and dosing intervals (two or four weeks) in patients with familial hypercholesterolemia on statin therapy, with or without ezetimibe, provided a taste of the extreme LDL reduction to be expected from this therapy [8]. As Prof. John Kastelein, MD, Amsterdam, The Netherlands, said, several manufacturers are currently working on the development of antibodies against PCSK9.
Literature list at the publisher
Source: Cardiology Update 2013, February 10-15, Davos