Technical developments now allow endovascular treatment of smallest pelvic vessels in patients with erectile dysfunction. Vascular erectile dysfunction may serve as an early indicator of developing atherosclerosis, so angiologic evaluation of patients with erectile dysfunction and known cardiovascular risk is quite reasonable. Since erectile dysfunction often has multifactorial causes, interdisciplinary collaboration in treatment is important.
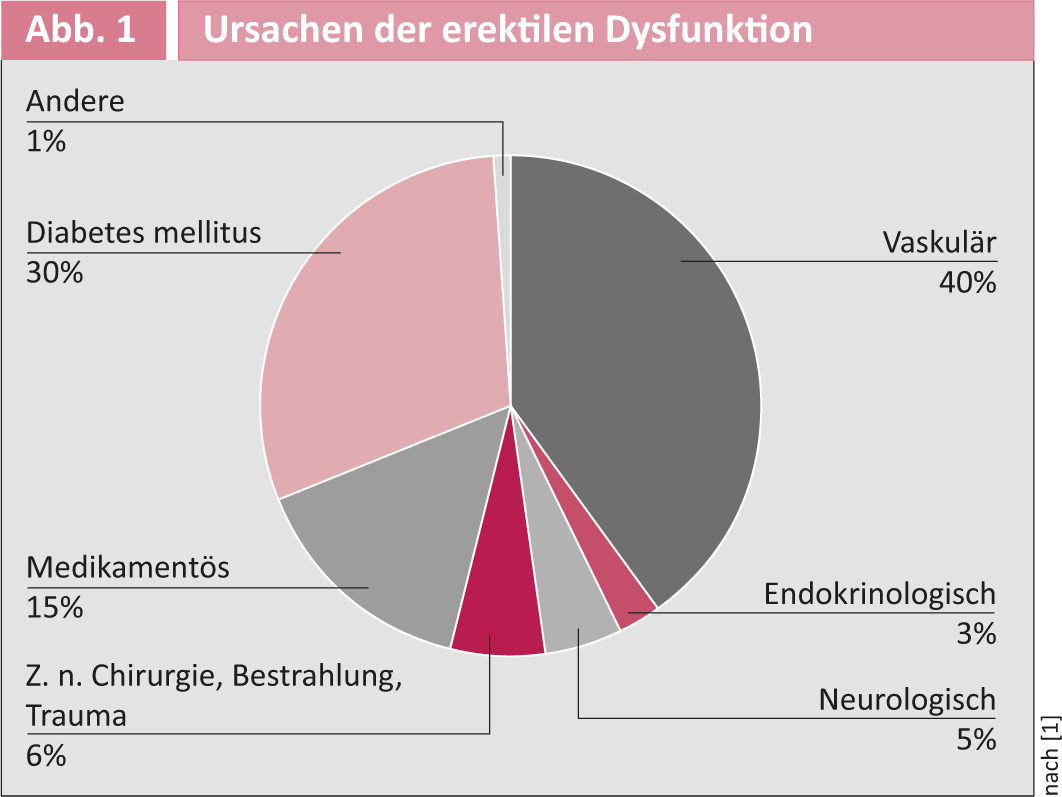
More than 150 million men worldwide suffer from erectile dysfunction (ED). Their causes are diverse and often multifactorial, but vascular problems represent one of the most important causes of organically induced ED(Fig. 1).
Many patients with ED have multiple cardiovascular risk factors such as presence of peripheral arterial disease, coronary artery disease, nicotine abuse, hyperlipidemia, arterial hypertension, diabetes mellitus, and positive family history.
In addition to the functional impairments in sexual intercourse that are the primary concern for affected patients, symptoms of ED also serve as a possible early
indicators of the presence of atherosclerotic changes in other stromal areas of the body. It has been shown that up to 70% of male patients with new-onset angina had anamnestic preceding symptoms of ED.
Current treatment methods for patients with ED, such as intracavernosal injection of prostanoids or the use of a vacuum pump, are limited and sometimes very uncomfortable.
The introduction of phosphodiesterase inhibitors such as Viagra has shown improvement in clinical use for many patients, but up to 50% of those studied show suboptimal response to these drugs.
Surgical revascularization of arterial lesions has not gained acceptance in clinical practice for several reasons:
- Various surgical techniques have been used in a nonstandard manner.
- Diffuse and nonfocal arterial obstruction is often present in ED patients with cardiovascular risk factors.
- Published studies have very limited patient numbers.
- Surgical procedures have specific morbidity risks such as wound healing disorders and impairment of nervous structures, which may lead to anesthesia and/or retrograde ejaculation.
Diagnosis of vascular causes of erectile dysfunction.
History: The specific history in ED patients in whom vascular problems are thought to be the cause includes the following:
- Cardiovascular risk factors
- Cardiovascular self and family history.
- Presence of claudication symptoms (in case of isolated iliac obstruction also gluteal or thigh claudication)
- Medication history (the following groups of medications may be causally involved in ED: Antipsychotics, antihypertensives, antidepressants, antiandrogenic and antihistaminic agents).
- Onset of ED symptomatology
- Existence of decreased rigidity, too early drop of a briefly achieved erection, or complete loss of tumescence (very rare).
- What measures have been tried (phosphodiesterase inhibitors, intracavernosal injection, vacuum erection aids, etc.)?
- Corpus cavernosum auto-injection test: If a low dose of prostaglandin results in a full erection, neurogenic, psychogenic, or hormonal ED is likely. If a moderate to high dose results in an erection, a vascular cause is likely. If even high doses do not result in erection, veno-occlusive dysfunction is likely the cause of ED.
- Two different questionnaires (International Index of erectile function [IIEF] questionnaires, IIEF-6 and IIEF-15) provide further details of the expression of ED.
Oscillometry and determination of the ankle-brachial index: Since arterial obstructions in ED patients are also located in the region of the common iliac artery and can cause the symptoms of penile blood loss, it is recommended to perform a basic angiological examination by means of palpation of the peripheral pulses, determination of the ankle-brachial index and oscillometry of the lower extremity. It should be noted that resting perfusion may be normal in patients with well-collateralized iliac artery obstructions and that the current territory of the internal iliac artery eludes this hemodynamic study because of its anatomic location. Thus, normal hemodynamic findings at rest do not exclude arterial obstruction of the large and smaller iliac arteries.
Duplex sonography: Following the above-mentioned hemodynamic examinations, duplex sonographic imaging of the iliac arteries is recommended to exclude arterial macroangiopathy. In addition, the inguinal arteries should be examined with regard to puncturability for possible angiography. In addition, penile duplex sonography under pharmacologically induced erection after intracavernosal injection of alprostadil is an important step before any further invasive procedure by angiography.
If the arterial flow velocity is below a defined threshold(Fig. 2), this is an indicator for a possible presence of proximal obstruction, which may lead to insufficient arterial inflow to the penis.
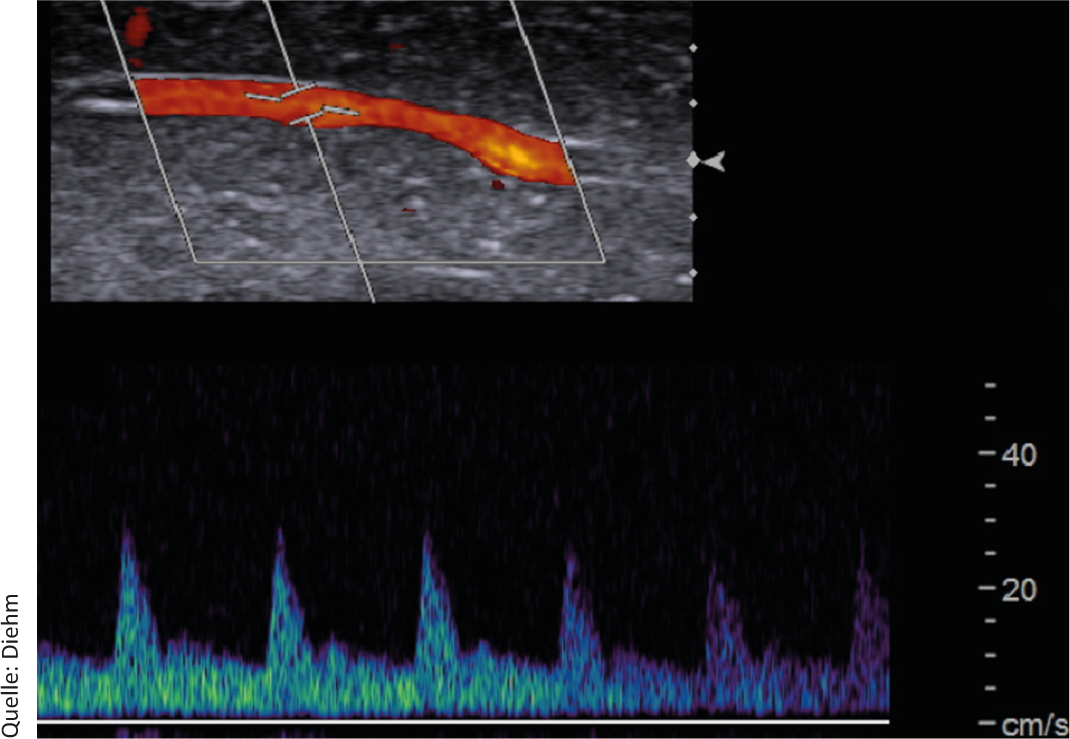
Fig. 2: Causes of erectile dysfunction. Duplex sonographic imaging of an arterial flow profile in the profunda penis artery after application of alprostadil. Systolic flow velocity is reduced and angiographic evaluation of the findings is recommended. Furthermore, end-diastolic flow velocity is borderline elevated, which is why venous leakage is also suspected.
In addition to intact arterial, neurovascular, hormonal, and structural-anatomic conditions, initiation and maintenance of an erection also requires normal veno-occlusive function. This means that blood enters the corpora cavernosa via the artery, which then fills, compressing the draining veins and thereby leading to venous leakage during erection. Thus, with preserved arterial inflow, adequate erection can occur even in the presence of venous leakage, which can often be the cause of ED. Venous leakage is assumed to be present when the end-diastolic velocity in a cavernous artery is >5 cm/s. If this is the case in an ED patient and arterial inflow is assured, open surgical or even endovascular (embolization) treatment of venous leakage can be discussed.
Technique of endovascular diagnostics and therapy
Angiography: If the presence of arterial obstruction is suspected on the basis of the above examinations, angiography of the iliac arteries is recommended. This can be performed through a small arterial puncture hole initially without insertion of an airlock.
Here, the external and internal iliac arteries are visualized on both sides. In particular, selective visualization of the internal iliac arteries requires the presence of extensive interventional experience, as manipulation in this stromal area can lead to dissection if not done carefully.
If angiographic imaging of the above-mentioned vessel segments reveals relevant obstruction, balloon angioplasty and, if necessary, stent implantation may be considered. This requires the insertion of an arterial sheath with a minimum diameter of four French.
Because ED patients are usually less polymorbid vascular patients, the puncture hole can often be treated with compression and pressure dressing, and this minimally invasive treatment approach allows the majority of patients to be treated on an outpatient basis.
In the area of the common iliac artery and internal iliac artery, implantation of a stent is often unavoidable due to frequently highly calcified eccentric lesions. In more distal vessels such as the internal pudendal artery, good morphologic results can often be achieved with balloon angioplasty alone. However, this artery usually has diameters smaller than 3 mm, and the restenosis rate after balloon angioplasty alone is unclear.
Results of endovascular therapy of arterial obstructions in the lesser pelvis.
Different authors first reported functional treatment success of ED patients with obstruction of the proximal iliac arteries (Arteriae iliacae communes, Arteriae iliacae externae) (Fig 3).
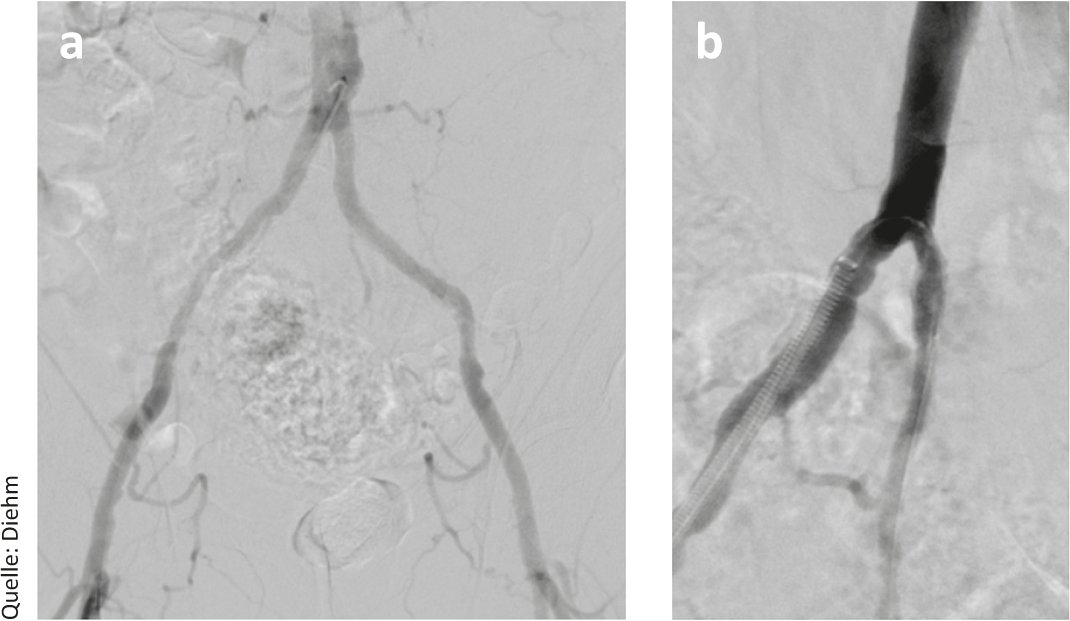
Fig. 3: (a) Arterial pelvic survey angiography. The external iliac arteries show only discrete atherothrombotic changes. However, there is functional occlusion of both internal iliac arteries; (b) Selective visualization of the right internal iliac artery and placement of drug-eluting stents.
Endovascular therapy of arterial obstructions in the stromal area of the internal iliac artery and especially the internal pudendal artery has become increasingly feasible in recent years due to miniaturization of catheter technology(Fig. 4). In line with this current development, the data available on this is currently limited to one recently published study.
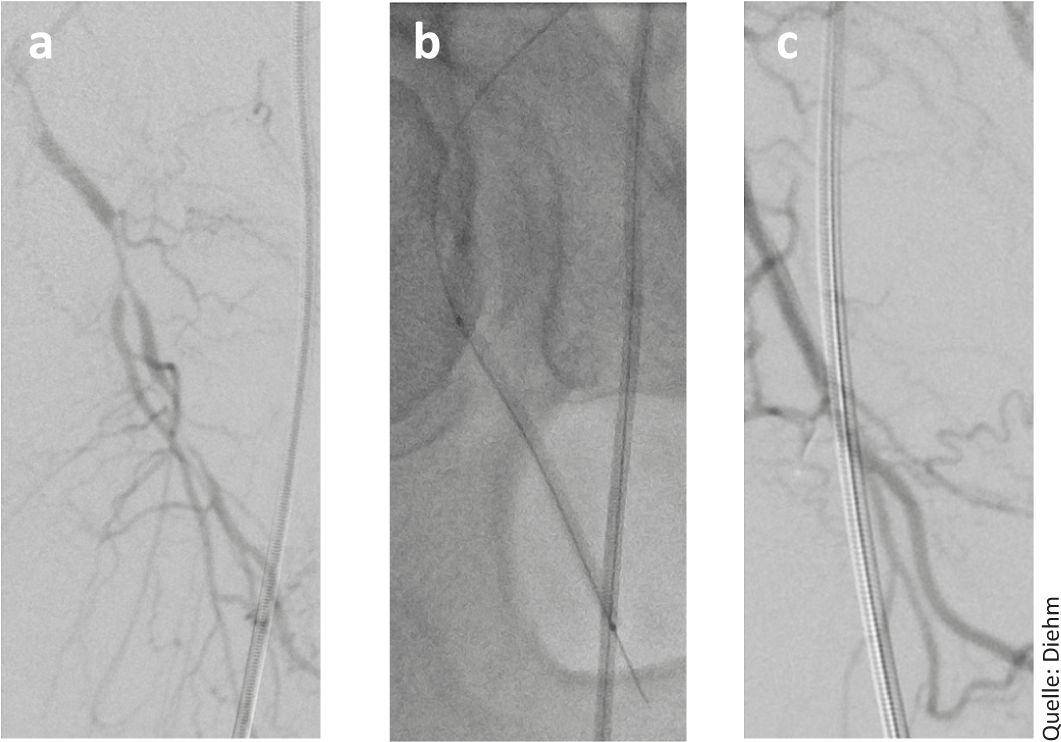
Fig. 4: (a) Angiographic demonstration of high-grade stenosis of the internal pudendal artery; b) Balloon dilatation of this stenosis (c) and angiographic final result.
Rogers and colleagues treated 30 men aged approximately 60 years and with a suboptimal response to PDE-I with angiographically verified stenosis of one or both internal pudendal arteries by implantation of drug-eluting coronary stents.
For this purpose, patients had previously been screened for penile reduced perfusion by duplex sonography of the profunda penis artery after intracavernosal injection of a prostanoid. A total of 383 patients had to be screened for this study and 89 angiographed to implant a stent in the stromal territory of the internal pudendal artery in 30 men. About one third of the patients were not suitable for dilatation due to lack of obstruction, and another third due to excessive obstruction.
The technical success of the catheter intervention, in which arteries with a mean diameter of 2.6 mm had been treated, was 100%. After stent implantation, nearly 60% of dilated patients had functional improvement in penile blood flow. However, at six months, the angiographically verified restenosis rate was 34%. This pilot study shows encouraging results of endovascular therapy in patients with ED due to atherosclerosis. Further studies in this interesting field, which has been clinically neglected in many places, should investigate the value of endovascular therapy compared with purely conservative therapeutic measures.
Conclusion
Up to 50% of ED patients show suboptimal response to PDE inhibitors. Based on the available data, revascularization of these patients may be an attractive treatment option for many.
Technical improvements and miniaturization of catheter technology now allow endovascular therapy not only of the iliac trunk vessels but also of the arteries of the lesser pelvis supplying the penis.
Stenting is technically feasible and safe in patients with ED due to atherosclerosis in both iliac truncal and internal iliac artery involvement.
In view of the available epidemiological figures and the data from the ZEN study, angiological investigation of ED patients in whom cardiovascular risk factors are known seems quite reasonable. In addition to the functional effects on erection, which can result in a significant improvement in quality of life for affected patients, the detection of vascular ED in previously otherwise cardiovascular blanched patients is an important early indicator of manifesting atherosclerosis.
It should be noted, however, that currently clinical data on this minimally invasive procedure are still limited. Patients referred for angiologic evaluation should know that not all arterial obstructions are suitable for endovascular therapy and that not all patients who have been successfully revascularized technically will have functional success. This underscores the importance of interdisciplinary collaboration in ED, which is often multifactorial.
Literature:
- Goldstein I: Sci Am 2000; 283 (2): 70-75.
- Rogers JH, et al: J Am Coll Cardiol 2012; 25; 60 (25): 2618-27.
- Saigal CS, et al: Arch Intern Med 2006; 166: 207-212.
- Blumentals WA, et al: Aging Male 2003; 6: 217-221.
- Schmid J-P, et al: www.medinfo-verlag.ch/zeitschriften/info_herz_gefaess/aktuelle_ausgabe
- Rogers JH, et al: Catheterization and Cardiovascular Interventions 2010; 76: 882-887.