The prevalence of diabetes mellitus is increasing worldwide, and with it the diabetes-associated secondary diseases. At the SGIM congress in Basel, it was reiterated that lifestyle intervention can provide greater benefit to the patient than the most aggressive medication. It should therefore always be attempted. Rare but clinically relevant to diabetic patients are endocrine disorders and diabetic autonomic neuropathy. In therapy, individualized strategies and coaching are currently being used to achieve improvement.
There is hardly any other field of internal medicine where so much research and publication is done as in diabetology. A scientific seminar at the SGIM congress was devoted to three rare but clinically relevant topics. Prof. Dr. med. Petra M. Schumm-Draeger, Munich, Prof. Dr. med. Jacques Philippe from Geneva and Prof. Dr. med. Peter Diem from Bern discussed the effects of endocrine diseases on diabetes mellitus, cardiovascular risk of diabetic patients and autonomic neuropathy.
Metabolism and endocrinium
Chronic poor metabolic management in people with type 1 and type 2 diabetes can alter endocrinological parameters. Dysfunctions in hormone balance, in turn, have serious effects on metabolic control in diabetes mellitus. “If symptoms are unclear, it is worthwhile to check the thyroid, adrenal and growth hormones,” Prof. Schumm-Draeger pointed out at the SGIM congress, using case studies. Hyperthyroidism, for example, promotes metabolic derailment through increased insulin resistance, decreased insulin sensitivity in the periphery, inhibition of insulin secretion, increased intestinal glucose uptake, pathologic glucagon release, and increased glycogenolysis in the liver.
Hypoglycemic tendency is increased in hypothyroidism. In patients with type 1 diabetes, serum TSH levels should be determined once a year and attention should also be paid to appropriate symptoms in type 2 diabetes.
Multi-glandular disease (polyglandular autoimmune syndrome, PAS, type-1 and type-2) is rare but clinically relevant. It can occur at the same time as type 1 diabetes or years later. Patients with incipient PAS may experience derailment even with latent hypofunction. “In people with autoimmune endocrinopathy or known PAS, regular screening for other endocrinopathies and associated diseases must be done,” Prof. Schumm-Draeger urged. The combination of immunothyreopathy and type 1 diabetes occurs most frequently in young adulthood (20-29 years). Autoimmune thyroiditis with hypothyroidism (or hyperthyroidism in Graves’ disease) and enteropathy autoantibodies (sprue) may occur. Prof. Schumm-Draeger illustrated with a recent case from her clinic that a new onset of hyperthyroidism can also massively derail type 1 diabetes mellitus during pregnancy. A 26-year-old diabetic patient developed Graves’ type hyperthyroidism and grade III endocrine orbitopathy at the tenth week of pregnancy, and her diabetes was derailed. Complete euthyroidism and metabolic stabilization were achieved by thyrostatic monotherapy with propylthiouracil. The woman gave birth to a healthy baby girl and postpartum Graves’ hyperthyroidism remained stable. Other cases from Munich showed the difficulty of blood glucose control in patients with adrenocortical insufficiency, and acromegaly also causes problems. A patient who presented to Prof. Schumm-Draeger with a diagnosis of metabolic syndrome ultimately suffered from Cushing’s syndrome due to hypercorticism.
Cardiovascular risk
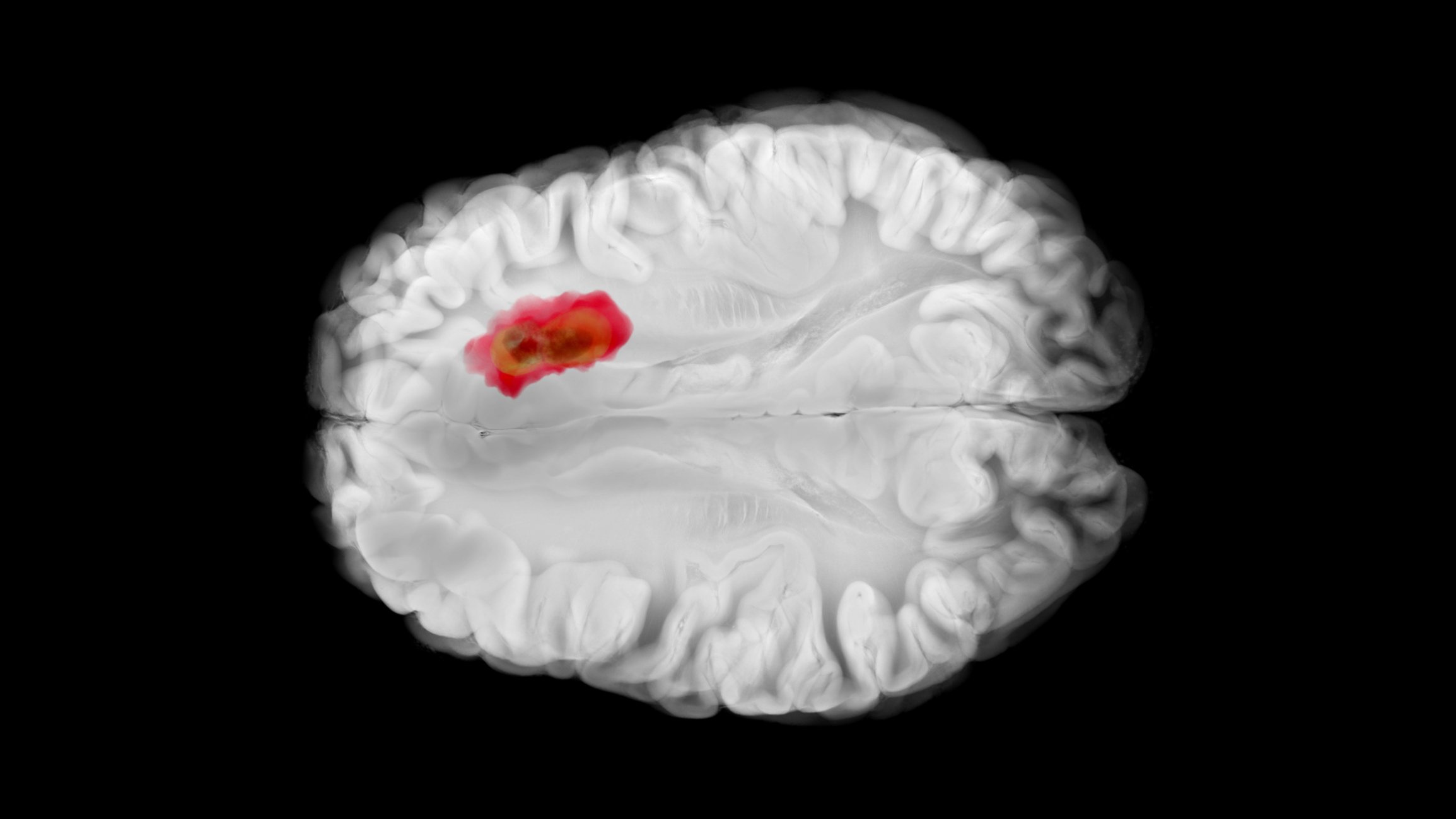
Diabetes mellitus doubles the risk for a variety of vascular diseases, independent of conventional risk factors. Cardiovascular event rate correlates with HbA1c, Prof. Philippe pointed out. Patients with type 2 diabetes, for example, have clustered ischemic coronary events, but often have no perception of risk due to lack of symptoms. They have poorer long-term prognosis and more complicated courses after cardiovascular interventions. In people without diabetes, the influence of fasting blood glucose concentration is modest and nonlinearly associated with vascular disease risk.
Intensified therapy of diabetes mellitus can reduce mortality from cardiovascular events. Prof. Philippe [1] referred to these facts, which are supported by study data. Nevertheless, systematic screening for coronary artery disease is not warranted, he said. To identify patients at increased risk, he said, it’s enough to put them on an EKG. Zoungas (2011) shows which patients should be screened for CHD and how.
Conversely, two-thirds of patients with initial manifestation of CHD have pathological glucose tolerance (IGT) or manifest diabetes. In IGT, early lifestyle modification and therapy with metformin or acarbose can prevent the development of manifest diabetes. Early and consistent treatment of IGT or diabetes shows the highest long-term effectiveness in preventing macrovascular events.
Diabetic autonomic neuropathy
“Little understood, there at some point, and mimicking hundreds of diseases,” is how Prof. Diems describes diabetic autonomic neuropathy. Autonomic neuropathies (AN) may present with pupillary dysfunction, cardiovascular with orthostatic hypotension or rate rigidity (“cardiovascular autonomic neuropathy”, CAN), gastroenterological with gastroparesis or enteropathy with alternation of constipation and diarrhea. In the genitourinary tract, bladder emptying disorders and erectile dysfunction are a consequence. Trophic skin changes or anhidrosis are relatively common. According to Prof. Diem, AN is clearly preventable.
“A cardinal symptom is gastroparesis. Patients complain of rapid satiety, food lingers for a long time (pizza still tastes good for breakfast). They feel bloated, and many suffer from nausea, vomiting and loss of appetite. In addition to smaller and more frequent meals, better management of diabetes (AN is partially reversible) and occasional proton pump inhibitors may provide relief.”
The management of CAN begins with diagnostics. Dysfunction in the regulation of the autonomic cardiovascular system is usually tested by heart rate variability and blood pressure response (“Ewing battery”). The first sign is a permanently increased heart action which, in contrast to heart-healthy persons, does not adapt to the current physical stress (constantly accelerated pulse even at rest, Schellong test).
In advanced neuropathy, nerve damage can cause circulatory disturbances of the heart to go unnoticed, “silent ischemia” of the heart. Therapy involves lifestyle changes and an individualized HbA1c level. It is important to avoid nocturnal hypoglycemia. If the heart rate is too high (sinus tachycardia), beta blockers can be used in low doses.
Detection of the risk
How high a person’s risk of developing diabetes can be determined using questionnaires such as the score from Kahn et. al. [2] and can also be determined on the Internet (e.g. Swiss Risk Test www.diabetesgesellschaft.ch or German Risk Test at www.dife.de). To date, numerous predictors of type 2 diabetes development have been identified that can be used for risk determination and targeted interventions. In addition to metabolic syndrome components (visceral obesity, hypertension, dyslipoproteinemia), these include lifestyle information (low physical activity, smoking), family history, dietary patterns, and several biomarkers. “Sensitivity and specificity can be significantly improved by including values for plasma glucose, HbA1ctriglycerides, HDL cholesterol and liver enzymes (gamma-GT, GPT) are increased,” noted Prof. Gerard Waeber, MD, from Lausanne. However, it is not possible to predict who will develop the disease and who will not on the basis of genotype alone (MEIGS 2012, Marques Vidal 2013). Another important piece of information is that those who manage to lose weight and maintain the weight loss reduce the risk of progression. 15 minutes of exercise per day over two weeks already improve insulin action (PENN 2013 CoLaus).
Currently, the relationship between iron and diabetes is also being increasingly investigated: Ferritin as a marker of diabetic inflammation. People with hemochromatosis are also more likely to get type 2 diabetes. After bloodletting had disappeared from the scene for a long time, scientific evidence has recently emerged that it could have beneficial effects on diabetes mellitus or on high blood pressure in obese people. An intervention study at Charite Berlin showed a good reduction of blood pressure by a mean of 16 mm Hg in hypertensive patients [3].
Therapy aspects from the expert
Prof. Dr. med. Marc Donath from Basel gave a practical account of how he manages his diabetes patients. “You can’t do it without lifestyle discussion,” he elaborated. If possible, he consults a sports physician in order to find a physical activity that he enjoys, even for the most resistant to exercise to date. It’s a matter of getting reserves out, not just relying on drugs. As long as a patient presents in good general health, a great deal can be accomplished through lifestyle modifications. Even when it comes to nutrition, Prof. Donath relies less on prohibitions and more on giving the patient tips with a positive connotation: “If you are allowed to eat a piece of chocolate cake for breakfast, you will manage better to lose weight, stick to a diet and maintain your weight [4]. Eating is something legal, you won’t achieve anything with prohibitions.” It is also important that patients with diabetes always drink enough. Numerous coaching programs have been tested for success and are an important tool.
For the treatment of type 2 diabetes mellitus, metformin is definitely number two after lifestyle modifications. If these measures are not sufficient, further individualized combinations are used today. Sulfonylureas are no longer an option for Prof. Donath because of the risk of hypoglycemia and weight gain: “The new substances gliptins (DPP-IV inhibitors) and GLP1 analogs for weight problems have been in use for six years, they are safe, and the successes with them also justify the higher costs.” In addition, he said, there are attractive effective combinations.
Insulin continues to have its firm place. “Insulin is always the right thing to do to achieve therapeutic success in unclear cases,” Prof. Donath elaborated. “New is a very long-acting insulin: Deglutec (Tresiba®). The advantages are somewhat more stable blood glucose control, fewer nocturnal hypoglycemias and a wide range of users. The consequences of hypoglycemia have long been underestimated. They cause psychosocial stress as well as a negative impact for cardiovascular and neurological comorbidities.” In those over 65 years of age, they disproportionately lead to emergency admissions [5].
Source: “Diabetes richtig therapieren”, Seminar at SGIM/ SSMI Congress, May 29-31, 2013, Basel.
Literature:
- Boussageon R, et al: Effect of intensive glucose lowering treatment on all cause mortality, cardiovascular death, and microvascular events in type 2 diabetes: meta-analysis of randomised controlled trials. BMJ 2011; 343: d4169. doi: 10.1136/bmj.
- Kahn HS, et al: Two riskscoring systems for predicting incident diabetes mellitus in US adults age 45 to 64 years. Ann Intern Med 2009; 150(11): 741-751.
- Houschyar S, et al: Effects of phlebotomy-induced reduction of body iron stores on metabolic syndrome: results from a randomized clinical trial. BMC Medicine 2012, 10: 54.
- Jakubowicz D, et al: Meal timing and composition influence ghrelin levels, appetite scores and weight loss maintenance in overweight and obese adults. Steroids 2012 Mar 10; 77(4): 323-331.
- Budnitz DS, et al: Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011 Nov 24; 365(21): 2002-2012.
- Gaede P, et al: Intensified multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: the Steno type 2 randomised study. Lancet 1999 Feb 20; 353(9153): 617-622.
CONGRESS SPECIAL 2013; (1-2): 27-30