In approximately half of the patients with a venous thromboembolic event (VTE), a thrombophilic diathesis can be found with an appropriate coagulation evaluation. A coagulation test is not mandatory or useful in every case of VTE – in general, a test is useful if the (potential) result in a specific case has an influence on the indication or the duration or intensity of treatment. Furthermore, in specific patient situations, the additional information obtained from thrombophilia clarification can be helpful in the management of the patient. The authors therefore advocate an individual and situation-specific indication for coagulation clarification.
Thrombophilia – forms and frequencies
As a correlate to the clinical observation of familial clustering of VTE, inherited deficiencies for antithrombin [1], protein C [2], and protein S [3] have been found over the past 50 years, as has “resistance” to activated protein C (APC resistance)[4], which could eventually be attributed to a mutation in the gene encoding factor V [5, 6]. In this context, the nucleoside transition G → A at position 1691 of the factor V gene (FV G1691A mutation) leads to the replacement of the arginine amino acid by glutamine at position 506, resulting in a reduced degradation of factor V by the activated protein C that attaches there (APC resistance). A frequent mutation in the factor II gene (prothrombin gene mutation G20210A) was also found, which is also associated with an increased incidence of VTE via increased prothrombin levels [7]. Other coagulation parameters that appear to be associated with a clinical propensity for VTE include repetitively detected factor VIII elevation [8] as well as laboratory evidence of an antiphospholipid antibody (positive lupus anticoagulant, elevated antiphospholipid antibody titers), which is also clearly associated with VTE risk [9]. Even though thrombophilia can be detected in slightly less than half of the patients with VTE overall [10]If we consider that the two most common coagulation disorders in Europe (prevalence of FV G1691A and FI G20210A mutations ~5% and ~3%, respectively) are associated with a moderate relative risk increase for VTE of ~5% and ~3%, respectively, in isolated heterozygosity. ~3%) are associated with a moderate relative risk increase for VTE of ~5 and ~3, respectively, in isolated heterozygosity – and therefore gain clinical significance especially in the presence of additional (hereditary or acquired – e.g., anticonception) risk factors. For example, in the presence of a proven heterozygous factor V Leiden mutation, hormonal (estrogen-containing) anticonception increases the relative risk by a factor of 5-10 and thus becomes clinically relevant (VTE risk 0.2-0.5%/year) – a risk that can be circumvented with simple measures (switching anticonception to e.g. purely progestogen-containing preparations).
Protein C, protein S, and antithrombin deficiencies are rare (prevalence ~0.2%, and 0.1%, ~0.02%, respectively) but associated with higher risk (5-10-fold). In demographic assessment, they are therefore less relevant than factor V and II mutations because of their lower prevalence; however, because of the higher relative risk, they are likely to be more relevant to individual management.
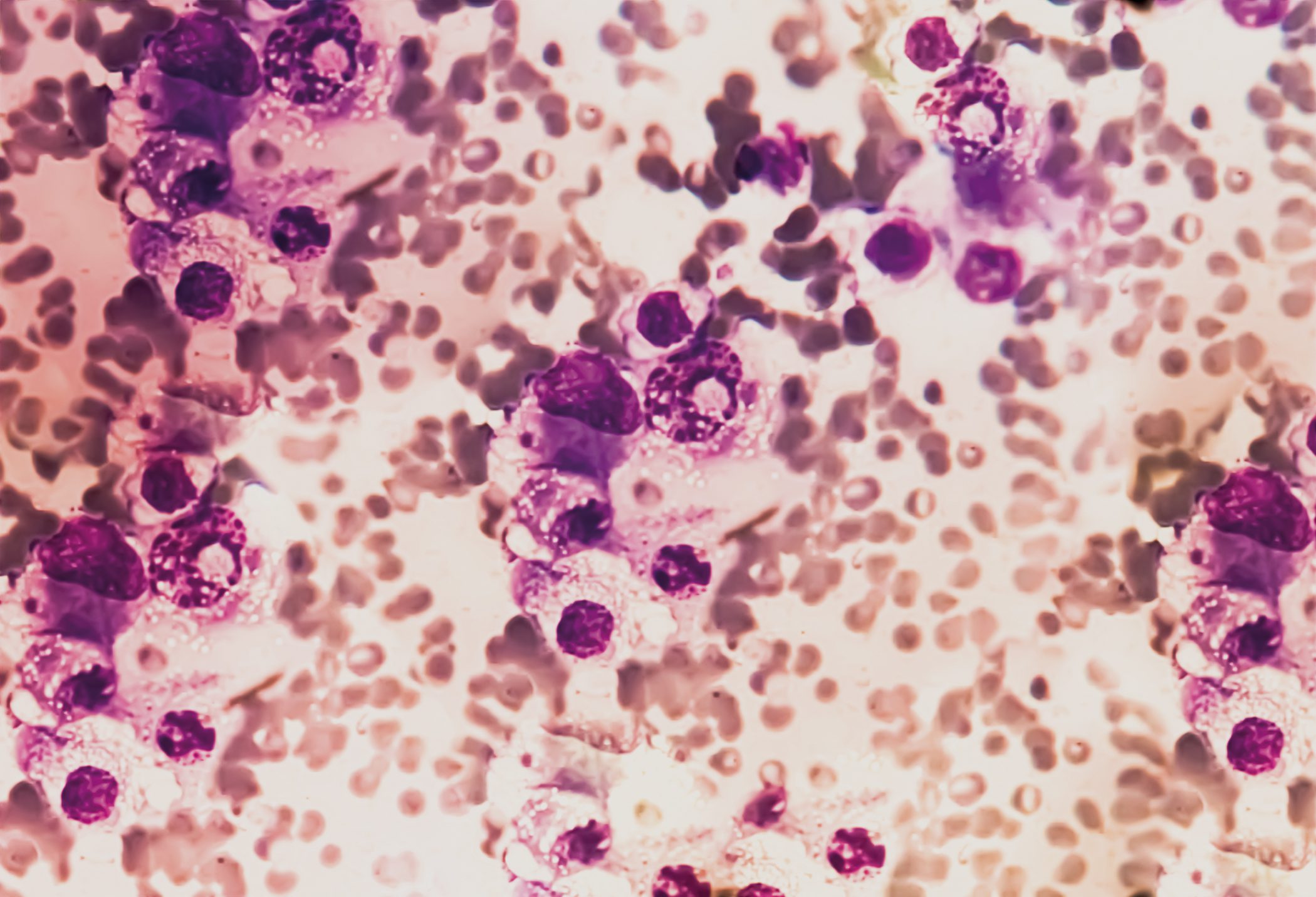
While most of the thrombophilias mentioned are hereditary, antiphospholipid antibody syndrome (APAS) in particular is acquired (although a familial clustering has also been described, but this may be due to a general familial predisposition to autoimmunopathies). Antithrombin deficiency – in addition to its inherited form – can also occur in the context of liver disease (reduced synthesis), nephrotic syndrome and protein-losing enteropathy (increased loss) and use of certain drugs (asparaginase in leukemia treatment).
More advanced coagulation analyses have not yet been defined in terms of their clinical significance.
Thrombophilia clarification – indication
Regarding the risk of recurrence after VTE, rates between 15-25% are reported within 5 years [11–13] – the “EINSTEIN extended” study has subsequently seen up to 10% recurrences after 6-12 months of anticoagulation (with vitamin K agonists or Xarelto®) in the first 12 months after completion of anticoagulation [14]. This rate explicitly applies to that patient population in which there is no compelling indication for continued (i.e., prolonged beyond 6-12 months) anticoagulation, but in which this indication is also not clearly absent.
According to these recurrence rates, it would be of interest to better define the individual risk and to derive consequences for the intensity and duration of anticoagulation. In the absence of an evidence-based rationale for routine thrombophilia assessment after VTE [15]The decision to investigate should be individualized, as the results can be very helpful for clinical assessment and further decision-making, especially when – as in the case of unprovoked VTE – even international guidelines do not clearly define the duration of oral anticoagulation or recommend risk analysis after anticoagulation beyond three months. [16]. According to the authors, this risk analysis should include not only an assessment of the bleeding risk with regard to prolonged or even unlimited anticoagulation, but also an estimation of the risk of recurrence – here, thrombophilia clarification can provide assistance. In addition, the clinical, individual situation is often more complex than can be represented in guidelines. The following brief clinical examples illustrate the complexity of the respective issues:
- For example, is a second provoked leg vein thrombosis occurring 10 years apart reason enough to start oral anticoagulation in a 50-year-old patient for the remaining decades of his life?
- Is 6 months of anticoagulation sufficient after an unprovoked pulmonary embolism that initially destabilizes the circulation in a young woman with a clearly positive family history of VTE? How to answer the query of the sister of just mentioned young woman regarding her own risk in terms of planned hormonal anticonception or pregnancy?
- How should the risks be weighed when a patient on long-term oral anticoagulation prescribed for two venous thromboembolic events now requires dual antiplatelet therapy because of a newly inserted coated stent?
These clinical scenarios show that not a general, but an individualized thrombophilia diagnosis is justified in the overall assessment of complex situations. Thrombosis in an unusual location (arm/subclavian vein thrombosis, portal or ovarian vein thrombosis) should lead to broadening the differential diagnostic spectrum beyond coagulopathy: Compression syndromes in the shoulder girdle region must be considered as a causative component in the former, intra-abdominal thromboses may be associated with an increased tendency to thrombosis in the context of a myeloproliferative syndrome (accordingly, search for a JAK2 mutation if necessary) or in the context of paroxysmal nocturnal hemoglobinuria (determination of hemolysis parameters, further clarification in this regard if necessary). Likewise, in the context of arterial and also venous thrombosis in younger patients as well as in the setting of pregnancy complications (recurrent abortions, gestoses, intrauterine growth retardation), an antiphospholipid antibody syndrome should be considered, which, if untreated, is associated with a risk of thrombosis recurrence of 10-30%/year [17] and therefore generally justifies long-term anticoagulation.
To determine the adequate duration of oral anticoagulation, a simple determination of coagulation activation parameters (e.g., D-dimers) one month after completion of 6 months of anticoagulation may be helpful: Clinical Studies [18] demonstrate that those patients with persistently elevated clotting activity have a significantly increased risk of recurrence within the subsequent two years than those with D-dimer levels <0.25mg/l (12-15% vs. 3-4%).
Family clarifications after detection of a hereditary coagulation disorder in the index person with manifest VTE must be considered and should be discussed with the potentially affected persons with regard to possible consequences before the tests are performed – since a positive finding in a relative without a personal history of VTE often remains without consequences, restraint should definitely be considered in such situations. As an exception, control in female relatives of patients with VTE and proven thrombophilia should certainly be considered here, who enter into an additional risk increase in connection with hormonal anticonception, pregnancy, or hormone therapy.
Thrombophilia clarification – timing
While molecular genetic analyses (concerning factor V Leiden and prothrombin gene mutation) are independent of the time of their determination and other factors, the natural anticoagulants and also other parameters of coagulation analysis are subject to various influencing factors. Thus, the determination of the proteins C and S, which are also vitamin K-dependent, makes little sense under coumarin therapy. Antithrombin may be distorted under heparin therapy. Coagulation parameters are also altered during pregnancy (e.g., increased D-dimers, decreased protein S), so that a thrombophilia test should only be performed after a certain latency period postpartum. The clarification with regard to an antiphospholipid antibody syndrome should ideally also be performed without simultaneous anticoagulation – although the determination of antiphospholipid antibodies is possible at any time, the search for a lupus anticoagulant, however, is influenced by changes in vitamin K-dependent factors and should only be performed after at least a three-week coumarin break and at least 24 h after the last administration of a low-molecular-weight heparin (NMH) or a new oral anticoagulant.
Finally, it is not uncommon for coagulation parameters to be altered by consumption in the situation of an acute thrombotic event, so that a time interval between VTE and thrombophilia clarification is generally recommended.
Pragmatically, we usually recommend performing the thrombophilia assessment one month after completion of e.g. 6 months of anticoagulation after VTE. This can then also be combined with the determination of coagulation activation parameters (see above). However, if a clinical risk situation exists that makes a suspension of anticoagulation inadvisable (v.a. antiphospholipid antibody syndrome, recurrent VTE, previous potentially fatal VTE, sinus vein thrombosis), we switch coumarin therapy to morning NMH (alternatively new oral anticoagulants) three weeks before the planned coagulation assessment – on the day of the coagulation assessment, the patient will apply NHM only after blood sampling, which also eliminates this potential confounding factor. A simultaneous determination of the highly sensitive CRP helps to detect inflammatory confounders.
Michael Baumann, MD
Prof. Dr. med. Wolfgang Korte
Literature list at the publisher