In type 2 diabetics, renal function should be checked at regular intervals. Nowadays, modern treatment approaches are available that can slow down the progression of diabetic nephropathy. If early use of SGLT-2 inhibitors does not lead to the desired improvement, a GLP-1 RA or a combination with other active substances (e.g. finerenone) should be considered as an alternative.
Type 2 diabetes is one of the most common causes of the development of chronic kidney disease ( CKD) in the long-term [1]. “We know that kidney function impairment, and early CKD in particular, statistically leads to a dramatic reduction in life expectancy,” reported Prof. Sebastian Meyhöfer, MD, Director of the Institute of Endocrinology and Diabetes and Head of the Division of Endocrinology, Diabetology and Metabolic Medicine, University Hospital Schleswig-Holstein (D) [2]. CKD promotes arterial hypertension and is a relevant cardiovascular risk factor [3]. Moreover, renal anemia, metabolic acidosis, hyperkalemia, renal osteopathy, and vascular calcification due to hypocalcemia and hyperphosphatemia are among the complications of CKD [3].
How often should type 2 diabetics be screened for CKD?
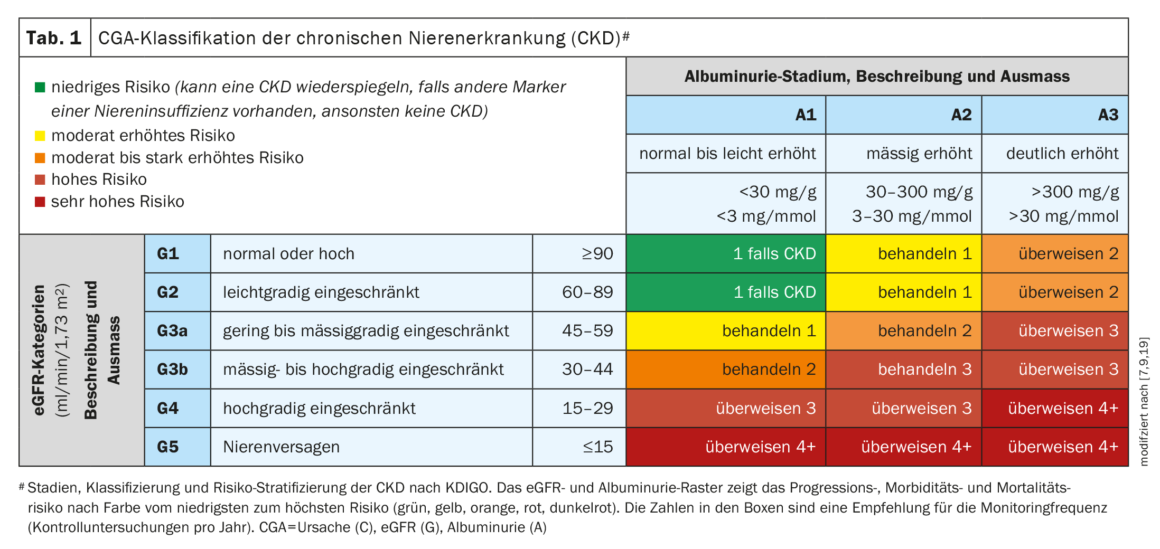
Regular monitoring of relevant diagnostic parameters to check renal function is very important in type 2 diabetes (T2D) to detect CKD as early as possible and to counteract progression by adequate treatment. It is recommended to screen for albuminuria at least once a year, and eGFR (estimated glomerular filtration rate) should also be determined [4]. In case of a positive finding regarding eGFR (<60 ml/min per 1.73m2) or albuminuria (UACR ≥30 mg/g), the examination should be repeated after a certain period of time [5]. If reduced GFR or relevant albumin excretion in urine is detectable for at least 3 months, chronic renal failure is present [6].
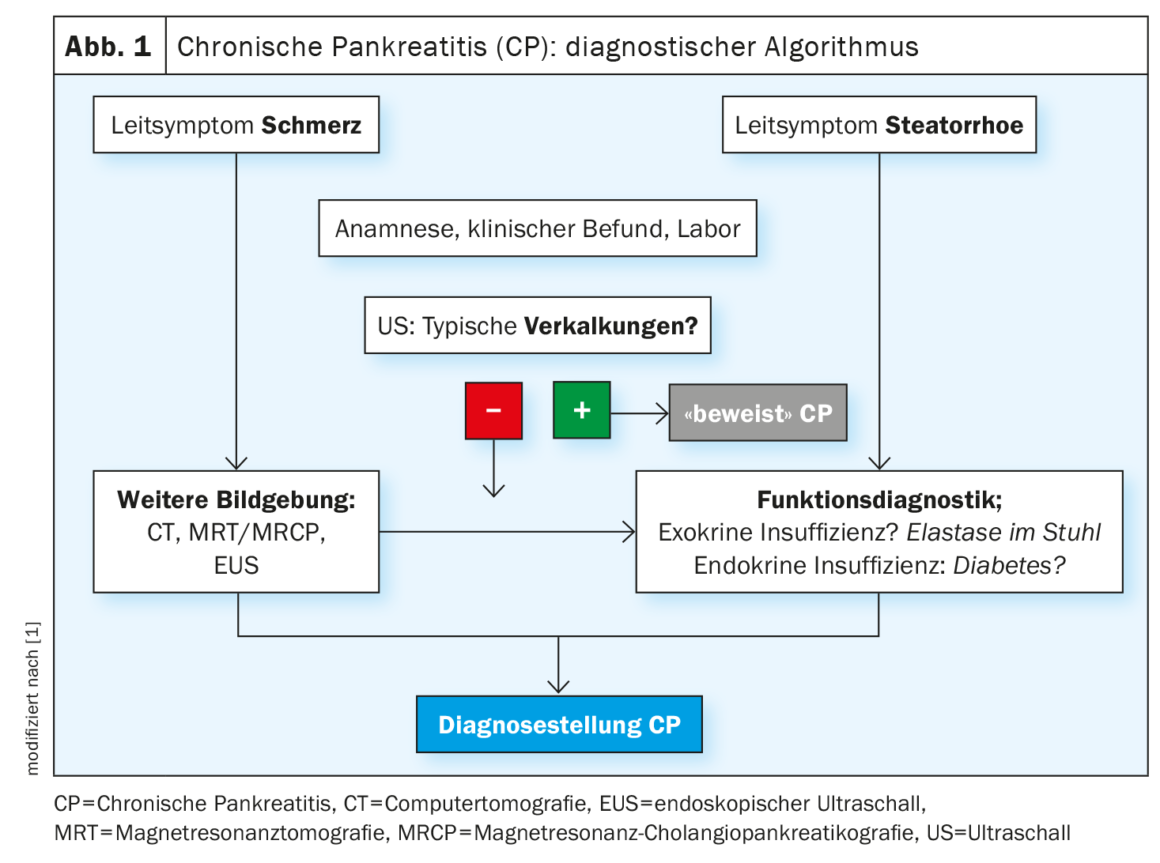
The Swiss Society of Nephrology also recommends that patients with type 2 diabetes be screened for the presence of CKD at least once a year [7,8]. The extent of renal function impairment can be classified using the CGA scheme: Cause, GFR category (G1-G5), albuminuria category (A1-A3) [7,9]. The CGA scheme is shown in Table 1 and the recommended screening algorithm is summarized compactly in Figure 1 .
SGLT-2-i: dapagliflozin and empagliflozin protect the kidney
In current guidelines for the therapy of T2D, the GLP$-1 receptor agonists (GLP-1-RA) and the SGLT&-2 inhibitors(SGLT-2-i) have a great importance due to the multiple proven organ-protective additional benefit. According to the German National Health Care Guideline (NVL), when lifestyle measures alone are not sufficient in patients with T2D, a cardiorenal risk assessment should first be performed [2,10]. If a clinically relevant cardiovascular/cardiorenal pre-disease is present, it is recommended to combine metformin with an SGLT-2-i or a GLP-1-RA right at the beginning of drug therapy**. “We select the substance according to the appropriate risk endpoint,” said Prof. Meyhöfer [2]. In diabetics with chronic renal insufficiency, the use of SGLT-2-i is favored [3]. “For all patients with chronic kidney disease up to an eGFR of 20 ml/min, SGLT-2 inhibitors have been shown to be highly efficient, both for renal endpoints, but also for the combination of cardiovascular death and dialysis dependency,” explained Univ.-Prof. Dr. med. Julia Weinmann-Menke, Head of Focus Nephrology, University Medicine of the Johannes Gutenberg University Mainz (D) [11]. Among others, the nephroprotective benefit of dapagliflozin was impressively demonstrated in the DAPA-CKD-(“Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease”) study. The main outcome of the study was that the use of dapagliflozin was associated with a risk reduction in terms of renal failure and hospitalization in CKD patients with and without T2D [12,13]. However, relevant evidence of efficacy is now also available for empagliflozin. The EMPA-KIDNEY (“Study of Heart and Kidney Protection with Empagliflozin”) study demonstrated cardio- and nephroprotective benefits in all eGFR categories [14,15].
$ GLP=Glucagon-like Peptide
& SGLT=sodium-glucose cotransporter
** A recent position paper of the Swiss Society of Endocrinology and Diabetology (SGED) suggests combining metformin with either an SGLT-2-i or a GLP-1-RA right at baseline in all T2D patients, regardless of cardiorenal risk [20].
Combinable treatment approaches to slow CKD.
Treatment of CKD in T2D addresses hemodynamic factors (increased blood pressure and/or intraglomerular pressure), metabolic aspects (poor glycemic control), and inflammatory-fibrotic factors, Prof. Meyhöfer explained [2]. SGLT-2-i influence both hemodynamic and metabolic factors. Alternatively, a GLP-1 RA can be used if target values are not achieved or if the patient is intolerant. There are several options for further escalation of therapy. In patients with albuminuria and hypertension, the current KDIGO guideline recommends renin-angiotensin-aldosterone (RAAS) blockade [16]. If there is a high residual risk of CKD progression and cardiovascular events or persistent albuminuria (>30 mg/g), a nonsteroidal mineral corticoid receptor antagonist (MRA) may be considered. Finerenone is currently the only nonsteroidal MRA with proven renal protective and cardiovascular benefits. That finerenone can slow the progression of diabetic kidney disease was shown by the FIDELIO-DKD (Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease), FIGARO-DKD (Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease) studies and the FIDELITY [16–18] analysis based on them.
Congress: Diabetology without borders
Literature:
- German Kidney Foundation: Diabetes and Kidney Disease, www.nierenstiftung.de/fuer-betroffene/niere-a-bis-z/diabetes-und-nierenerkrankungen,(last accessed 23.03.2023).
- “Cardio-renal-metabolic syndrome, pathophysiology and current therapy options. From the perspective of diabetology”, Prof. Sebastian Meyhöfer, MD. Diabetology Limitless, Feb. 03, 2023.
- “Chronic Renal Insufficiency,” www.medix.ch/wissen/guidelines/chronische-niereninsuffizienz, Last revised: 01/2021. Last modified: 02/2023, (last call 23/03/2023)
- Landgraf R, et al: Therapy of type 2 diabetes. Exp Clin Endocrinol Diabetes 2022 Sep;130(S 01): S80-S112. doi: 10.1055/a-1624-3449.
- “Rational Laboratory Diagnostics for the Assessment of Acute Renal Impairment and Progressive Kidney Disease,” interdisciplinary s2 guideline, 2021,
https://register.awmf.org,(last accessed 23.03.2023) - Greite R, Schmidt-Ott K: What is certain in the therapy of chronic kidney disease? [What is confirmed in the treatment of chronic kidney disease?]. Inn Med (Heidelb) 2022; 63(12): 1237-1243.
- Swiss Society of Nephrology, www.swissnephrology.ch/wp/wp-content/uploads/2021/11/161121_SGN_Pocketguide_CKD_Web_A4_d.pdf,(last accessed Mar. 23, 2023).
- SGED: GDMD criteria for “good” disease management diabetes in primary care, www.sgedssed.ch/fileadmin/user_upload/6_Diabetologie/64_Ressourcen_Hausarzt/Diabetes_Kriterien_2017_SGED_def.pdf,(last accessed 03/23/2023).
- American Diabetes Association. 5 Facilitating Behavior Change and Well-being to Improve Health Outcomes: Standards of Medical Care in Diabetes-2021. Diabetes Care 2021 Jan; 44(Suppl 1): S53-S72.
- National Health Care Guideline (NVL) Type 2 Diabetes – Partial Publication, 2nd edition, March 25, 2021.
- “Cardio-renal-metabolic syndrome, pathophysiology and current therapy options. From the perspective of nephrology”, Univ.-Prof. Dr. med. Julia Weinmann-Menke. Diabetology without borders, 03.02.2023.
- Heerspink HJL, et al.: Rationale and protocol of the Dapagliflozin And Prevention of Adverse outcomes in Chronic Kidney Disease (DAPA-CKD) randomized controlled trial. Nephrol Dial Transplant 2020; 35(2): 274–282.
- Heerspink HJL, et al.: DAPA-CKD Trial Committees and Investigators. Dapagliflozin in Patients with Chronic Kidney Disease. N Engl J Med 2020; 383(15): 1436–1446.
- Bakris G, et al.: Effects of Canagliflozin in Patients with Baseline eGFR <30 ml/min per 1.73 m2: Subgroup Analysis of the Randomized CREDENCE Trial. Clin J Am Soc Nephrol. 2020; 15(12):1705–1714.
- Chertow GM, et al.: DAPA-CKD Trial Committees and Investigators. Effects of Dapagliflozin in Stage 4 Chronic Kidney Disease. J Am Soc Nephrol 2021; 32(9): 2352–2361.
- Rossing P, et al.: Executive summary of the KDIGO 2022 Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease: an update based on rapidly emerging new evidence. Kidney Int 2022; 102(5): 990–999.
- Bakris GL, et al.: FIDELIO-DKD Investigators. Effect of Finerenone on Chronic Kidney Disease Outcomes in Type 2 Diabetes. N Engl J Med 2020; 383(23): 2219–2229.
- Pitt B, et al.: FIGARO-DKD Investigators. Cardiovascular Events with Finerenone in Kidney Disease and Type 2 Diabetes. N Engl J Med 2021; 385(24): 2252–2263.
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. Kidney Int 2013; 3(Suppl): 1–150.
- Gastaldi G, et al: Summary: Swiss Recommendations of the Society for Endocrinology and Diabetes (SGED/SSED) for the Treatment of Type 2 Diabetes Mellitus (2023), www.ksa.ch (last accessed Mar. 23, 2023).
HAUSARZT PRAXIS 2023; 18(4): 24–26