The fact that asthma is a clinical diagnosis that can only be made by looking at all the findings together applies particularly to children and adolescents. Patients with rare asthma symptoms can also suffer severe exacerbations. This is one of the reasons why the Global Initiative for Asthma (GINA) has been recommending an ICS/LABA fixed combination instead of SABA therapy for several years. In severe asthma, the use of biologics is possible after other treatment options have been exhausted.
The occurrence of characteristic features of asthma such as reversible airway obstruction, chronic airway inflammation and bronchial hyperreactivity is variable and heterogeneous, emphasized Chiara Abbas, MD, paediatric pulmonologist, Bern [1]. Sometimes several of these characteristics apply, sometimes only some of them. The most important asthma symptoms in childhood and adolescence include [2]:
- Shortness of breath on exertion
- Expiratory breath sounds (gurgling and humming, whistling breathing), and possibly distant gurgling in the expiratory tract
- Dry cough without infection, during or after physical exertion
- persistent nocturnal cough without infections.
When adolescents with asthma have inadequate symptom control, this is often accompanied by a high level of distress, according to the speaker [1]. There is no independent test that can definitively confirm or rule out asthma in children [2,3]. In addition to a differentiated medical history, non-invasive methods such as lung function measurement, measurement of fractional exhaled nitric oxide (FeNO) and recording of bronchial hyperactivity are usually sufficient for the diagnosis of asthma [2].
Asthma may also be present in the absence of SABA reversibility
The most important spirometric measurements are the forced vital capacity (FVC), the one-second capacity (FEV1) and the ratio FEV1/FVC(Tiffeneau index) [1,2]. If there is evidence of an obstructive ventilation disorder, a reversibility test should be performed to demonstrate the variable nature of the airway obstruction. This involves checking whether lung function, in particular FEV1, can be improved with a bronchodilator drug. Measurements are taken before and 15 minutes after inhalation of a short-acting beta-2 sympathomimetic (up to 400 µg salbutamol in four separate doses) [2]. In the event of a non-response to SABA, the FEV1 response to inhaled glucocorticoids (ICS) can be tested in a stable phase of the disease by inhaling a high dose of ICS twice a day for at least four weeks. A positive reversibility test in conjunction with typical asthma symptoms confirms the diagnosis of asthma. However, asthma can also be diagnosed in the absence of SABA reversibility if there are elevated type 2 markers and a response to ICS therapy. If bronchial hyperresponsiveness (BHR) is detected, a specific allergological history should be taken. The s2k guidelines updated last year point out that repeated measurement of FeNO in children and adolescents is of clear additional diagnostic benefit. Multiple high FeNO values increase the likelihood that it is asthma and that patients will respond to ICS.
ICS/formoterol fixed combination also as on-demand therapy
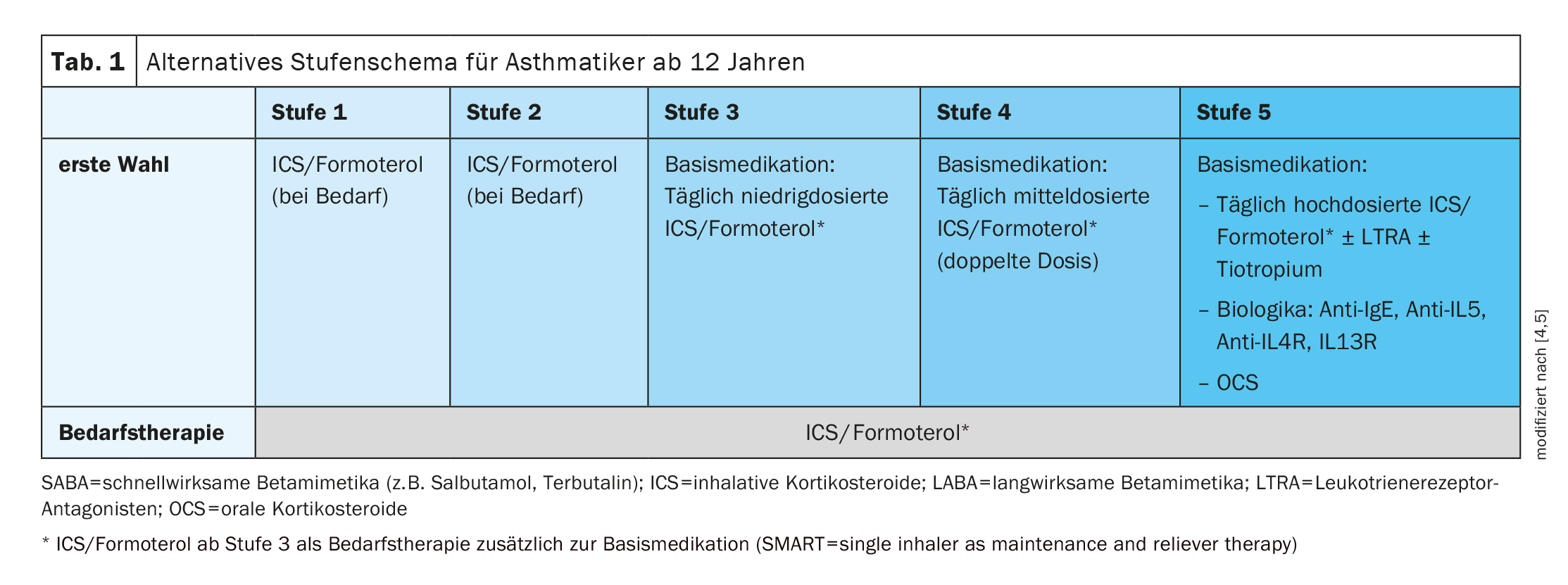
The aim of asthma treatment is to achieve and maintain the best possible asthma control, avoid exacerbations and suffer as few asthma-related restrictions as possible. Asthma therapy is based on the step-by-step scheme that is regularly updated by the Global Initiative for Asthma (GINA) in the respective guidelines [4]. In principle, treatment should be started as soon as possible after the diagnosis of asthma [5]. For some years now, a fixed combination of low-dose ICS and formoterol can be used from stage 3 both as a long-term therapy and as an on-demand therapy (Table 1). This therapeutic strategy is known as the SMART concept (“single-inhaler as maintenance and reliever therapy”) and is now considered established [2,6]. The GINA Guidelines 2019 were the first to suggest that a combination therapy with ICS/formoterol is preferable to an on-demand therapy with a short-acting betamimetic (e.g. salbutamol or terbutaline), even for adolescents aged 12 and over. According to the current guidelines, ICS/formoterol fixed combinations can be given as an on-demand therapy, i.e. when asthma symptoms occur, already in stages 1 and 2 in addition to the fixed daily basic medication (Table 1). On the one hand, this should reduce the risk of overuse of beta-2 sympathomimetics, and on the other hand, the early use of an ICS should achieve a steroid-sparing effect in the medium and long term. Dr. Abbas mentioned that she mostly uses these three medications approved for use in adolescents aged 12 and older [1,7]:
- Flutiform® DA 50/5 or 125/5 (metered dose inhaler; active ingredients: formoterol and fluticasone)
- Symbicort® (powder inhalation; active ingredients: formoterol and budesonide)
- Relvar ellipta® (powder inhalation; active ingredients: vilanterol and fluticasone furoate)
All three preparations contain a LABA (long-acting beta-2 sympathomimetic) and a glucocorticoid, but differ in terms of composition and form of administration. With regard to Flutiform®, the speaker reported that she usually uses the 125 µg/5 µg preparation twice a day [1]. Depending on this, the dose can be increased or used as required. “You can achieve better drug deposition with a pre-chamber,” says Dr. Abbas [1]. The pre-chamber is an inhalation aid and is also called a spacer or aerochamber. It should be noted that Symbicort® is not an emergency medication, which is why Ventolin® should always be added. One advantage of Relvar ellipta® is that it starts immediately and only needs to be inhaled once a day. This could be a decisive advantage for young people in particular, the speaker reported [1].
If necessary, use biologics & co. as an add-on
In most adolescent patients, treatment can be initiated at level 2, i.e. with a low-dose ICS [5]. The recommended dosages should be adhered to. In patients with pronounced symptoms (frequent awakenings, symptoms most days), therapy can be started at level 3. Level 4 is only used for cases with severe uncontrolled asthma or in the context of exacerbations. It is advisable to check the response to therapy after 2-3 months.
If asthma control is not achieved at level 3 or 4 despite the prescribed therapy, you can try doubling the ICS/formoterol dosage for a short time (for a maximum of 4 weeks). And if symptoms persist and exacerbations occur at stage 4 despite treatment adherence and correct inhalation technique, further treatment options are available at stage 5. In addition to high-dose ICS/LABA therapy, these include the addition of tiotropium, a leukotriene antagonist (montelukast) or a biologic (anti-IgE, anti-IL4R/IL13R, anti-IL5). However, the use of leukotriene antagonists has become cautious due to psychiatric side effects (e.g. nightmares), explained Dr. Abbas [1,10].
Progress assessment: Inhalation technique is crucial
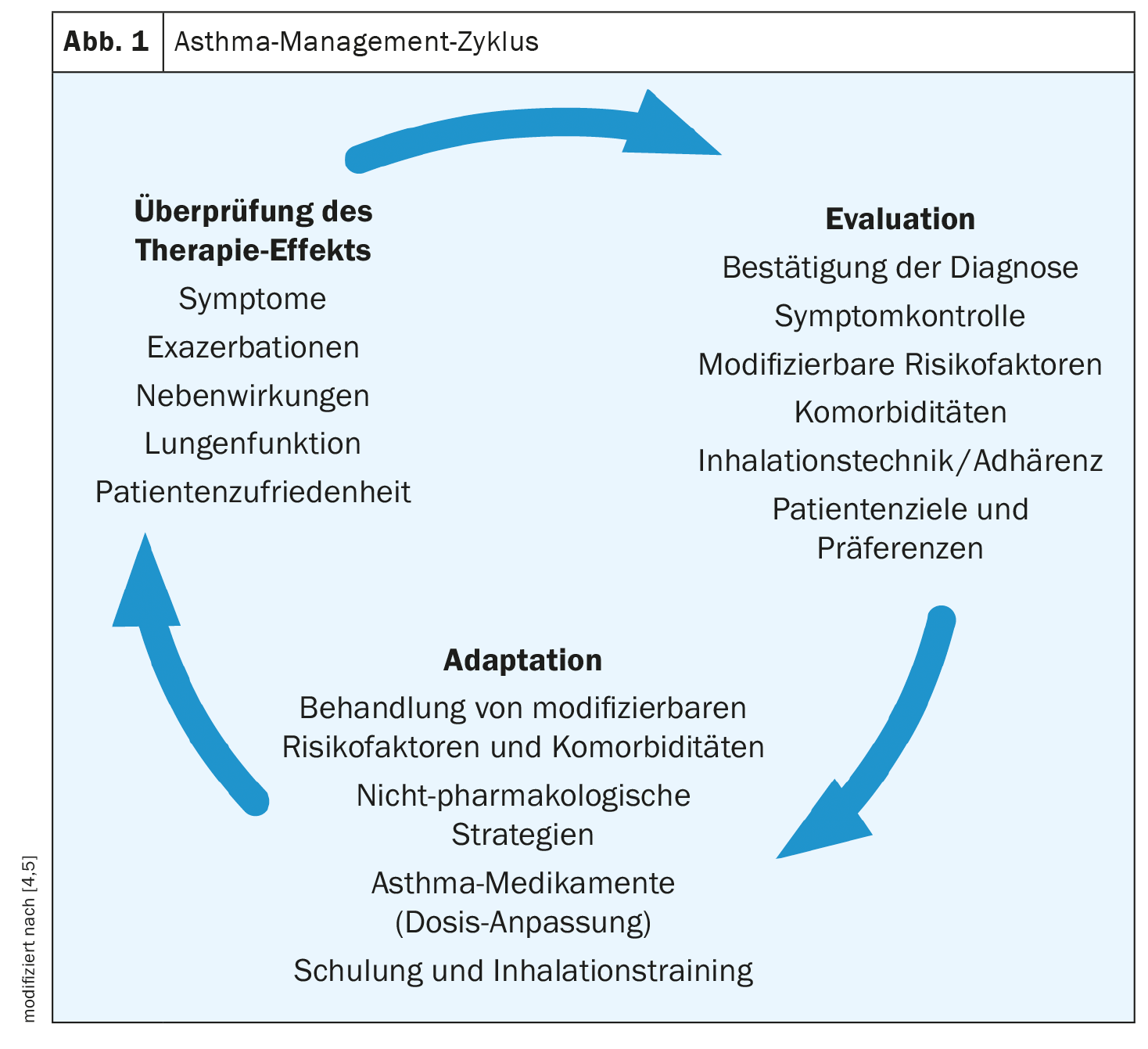
“Once you have decided on a therapy, it is important to keep reviewing it,” emphasized the speaker [1]. The individual steps of the review are shown in Figure 1. The current s2k guideline suggests recording the current level of asthma control at each patient contact [2]. It asks about complaints during physical activity, nocturnal complaints and use of emergency medication. This should be done in a structured way, for example using the (pediatric) asthma control test [11]. Correct inhalation technique is crucial for drug therapy to be effective. It is therefore important that the inhalation technique is checked regularly. It should be clarified whether the patient is comfortable with the inhaler, has mastered the inhalation technique and is carrying out the therapy as prescribed. Each inhalation device requires a specific inhalation maneuver and has its own system-specific requirements for correct inhalation [2]. If an inhalation system is changed, the patient should be retrained in its use and the need for dose adjustment should be checked [8,9].
Congress: Practical update Bern
Literature:
- “Asthma therapy for adolescents”, Dr. med. Chiara Abbas, Practice update, Bern, 21.03.2024
- “S2k guideline for the specialist diagnosis and treatment of asthma 2023”, German Society for Pneumology and Respiratory Medicine (ed.), AWMF register no.: 020-009.
- de Jong CCM, et al: Diagnosis of asthma in children: the contribution of a detailed history and test results. Eur Respir J 2019; 54. DOI: 10.1183/13993003.01326-2019
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. 2022. Available from: www.ginasthma.org,(last accessed 22.03.2024)
- Möller A, et al: Swiss recommendations for the diagnosis, treatment and management of asthma in children aged 5 years and older, https://cdn.paediatrieschweiz.ch/production/uploads/2023/09/34_3_2023_DE_02.pdf,(last accessed 22.03.2024)
- Beasley R, et al: Novel START Study Team. Controlled Trial of Budesonide-Formoterol as Needed for Mild Asthma. N Engl J Med 2019; 380(21): 2020-2030.
- Swissmedic: Medicinal product information, www.swissmedicinfo.ch,(last accessed 22.03.2024)
- Bjermer L: The importance of continuity in inhaler device choice for asthma and chronic obstructive pulmonary disease. Respiration 2014; 88: 346-352.
- Thomas M, et al: Inhaled corticosteroids for asthma: impact of practice level device switching on asthma control. BMC Pulm Med 2009; 9: 1. DOI: 10.1186/1471-2466-9-1.
- Watson S, et al: Montelukast and Nightmares: Further Characterization Using Data from VigiBase. Drug Saf 2022; 45(6): 675-684.
- Bime C, et al: Measurement characteristics of the childhood Asthma-Control Test and a shortened, child-only version. NPJ Prim Care Respir Med 2016 Oct 20; 26: 16075.
HAUSARZT PRAXIS 2024; 19(4): 30-32 (published on 18.4.24, ahead of print)