Giant cell arteritis and polymyalgia rheumatica are inflammatory rheumatic diseases that often occur together and almost exclusively affect people over the age of 50. Glucocorticoids are initially used for both clinical pictures, whereby the steroid dose should be reduced over the course of the disease in order to counteract the negative consequences of long-term use. As part of steroid-sparing therapy, immunosuppressants and biologics have proven their worth as add-ons.
In polymyalgia rheumatica, joints, tendon sheaths, entheses and bursae are inflamed. It mainly affects older people, although the prevalence is significantly higher in women. There are relevant overlaps between polymyalgia rheumatica (PMR) and giant cell arteritis (GCA), emphasized Prof. Dr. med. Frank Buttgereit, Deputy Clinic Director and Senior Consultant, Charité Universitätsmedizin Berlin [1]. There is an association between PMR and RZA in at least 50% of cases. Important differential diagnoses are seronegative rheumatoid arthritis, spondyloarthritis, crystal arthropathies, autoimmune myositis, fibromyalgia and osteoarthritis [2]. Glucocorticoids are still an important pillar of treatment, but should be phased out over the course of the disease. In addition to methotrexate (MTX), interleukin (IL)-6 blockade with tocilizumab is an effective steroid-sparing treatment option for PMR. In addition, promising data are now also available on rituximab and tofacitinib, the speaker reported [1].
In case of PMR, arrange for duplex sonography of the temporal arteries
If over 50-year-olds experience persistent muscle pain in the shoulders and/or pelvic girdle for at least two weeks with persistent muscle pain in the shoulders and/or pelvic girdle, accompanied by pronounced morning stiffness and general symptoms such as fever, fatigue, weight loss, depression or night sweats, this may be an expression of PMR [3]. New, bitemporally accentuated headaches, chewing pain, hypersensitivity of the scalp and visual disturbances are typical of RZA [4]. RZA is also accompanied by general symptoms such as fever or weight loss. The aetiopathogenesis of PMR and RZA is not yet fully understood; it is assumed that genetic factors, infections, ageing processes of the immune and vascular systems and endocrine axis disorders play an important aetiological role [5]. RZA and PMR are typically associated with elevated inflammatory markers; laboratory evidence of accelerated ESR and/or elevated CRP is indicative. A suspected diagnosis can be confirmed by imaging examinations (box) . Prof. Buttgereit advised looking for the presence of (subclinical) RZA by means of vascular ultrasound/angiography during the initial investigation of PMR, as this could have treatment-relevant implications [1].
| In PMR, ultrasound reveals inflammation in the area of the joints and the bursae of the shoulders and hips. Caliber jumps and low-echo concentric wall thickening (“halo” sign) in color-coded Doppler sonography are characteristic of RZA. Contrast-enhanced MRI of the shoulder girdle is helpful for the differential diagnosis of PMR, according to Prof. Buttgereit [1]. This is one of the findings of a study published in 2024 by Fruth et al. [19]. Corticosteroids are the standard induction therapy for both PMR and RZA. As a steroid-sparing treatment alternative, the data situation for tocilizumab is best for both RZA and severe, MTX-resistant PMR [11,15,16]. |
Treatment algorithm with MTX and tocilizumab as an add-on
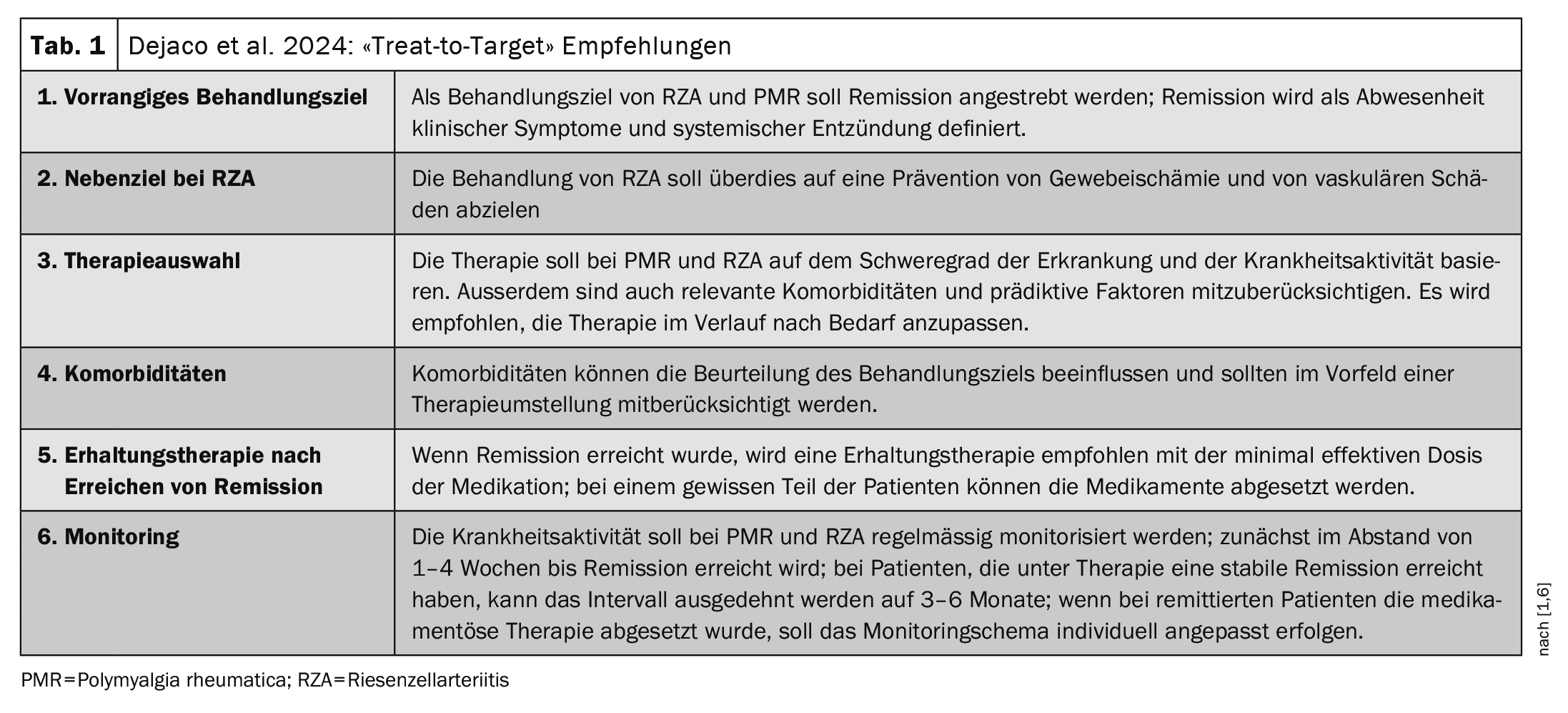
In the article by Dejaco et al. published in 2024 in the journal Annals of the Rheumatic Diseases a “treat-to-target” strategy is recommended, with remission and the prevention of tissue ischemia and vascular damage proposed as the treatment goal (Tab. 1) [1,6].
Remission is defined as the absence of clinical symptoms and systemic inflammation. Glucocorticoids (GC) are still used as first-line therapy for PMR and RZA, explained Prof. Buttgereit [1]. For PMR, he recommends prednisolone (p.o.) at a dose of 12.5-25 mg/d daily for initial therapy, followed by an individualized tapering regimen [3]. As a rule of thumb, the prednisolone dose should still be 10 mg/d after 4-10 weeks. In the event of a relapse, the dose must be slightly increased again temporarily. If it is not possible to reduce the steroids as planned, the immunosuppressant methotrexate (MTX) can be added to reduce the cumulative GC dose and the relapse rate [7]. In most studies, MTX doses of 10-15 mg/week p.o. or s.c. are used. In several prospective randomized studies, MTX proved to be effective, although the number of cases was rather small [8–10]. The interleukin (IL)-6 receptor-blocking monoclonal antibody tocilizumab also showed great potential for saving GC and has proven particularly effective in severe PMR and in the presence of PMR and RZA [11–13]. In a randomized proof-of-concept study, rituximab (RTX) also showed considerable corticosteroid-sparing effects [14]. In Switzerland, tocilizumab (Actemra®) has been officially approved for the indication of giant cell arteritis; in the case of PMR, a cost credit can be applied for [7,17]. To avert the threat of blindness in RZA, i.v. pulse therapy with methylprednisolone (250-1000 mg/day) for three days is recommended in the early stages of treatment [15,18].
Congress: EULAR Annual Meeting
Literature:
- “Polymyalgia rheumatica: What is new”, Prof. Dr. med. Frank Buttgereit, EULAR Annual Meeting, Vienna, 12-15 june, 2024.
- Mahmood SB, et al: Polymyalgia rheumatica: An updated review. Cleve Clin J Med 2020; 87(9): 549-556.
- Buttgereit F, et al: Polymyalgia Rheumatica and Giant Cell Arteritis: A Systematic Review. JAMA 2016; 315(22): 2442-2458.
- Schäfer VS, et al: Ultrasound cut-off values for intima-media thickness of temporal, facial and axillary arteries in giant cell arteritis. Rheumatology (Oxford) 2017; 56(9): 1479-1483.
- Buttgereit F, et al: S3 guideline for the treatment of polymyalgia rheumatica: evidence-based guideline of the DGRh, the ÖGR and the SGR and the participating medical-scientific societies and other organizations. Z Rheumatol 2018; 77(5): 429-441.
- Dejaco C, et al: Treat-to-target recommendations in giant cell arteritis and polymyalgia rheumatica. Ann Rheum Dis 2024; 83(1): 48-57.
- Rheumaliga Schweiz: Polymyalgia rheumatica and giant cell arteritis, www.rheumaliga.ch/assets/doc/ZH_Dokumente/Broschueren-Merkblaetter/Krankheitsbilder/Polymyalgia.pdf,(last accessed 23.07.24)
- Mahr AD, et al: Adjunctive methotrexate for treatment of giant cell arteritis: an individual patient data meta-analysis. Arthritis Rheum 2007; 56(8): 2789-2797.
- Cimmino MA, et al: Long-term follow-up of polymyalgia rheumatica patients treated with methotrexate and steroids. Clin Exp Rheumatol 2008; 26(3): 395-400.
- Marsman DE, et al: PolyMyalgia Rheumatica treatment with Methotrexate in Optimal Dose in an Early disease phase (PMR MODE): study protocol for a multicenter double-blind placebo controlled trial. Trials 2022; 23(1): 318.
- Devauchelle-Pensec V, et al: Efficacy of first-line tocilizumab therapy in early polymyalgia rheumatica: a prospective longitudinal study. Ann Rheum Dis 2016; 75(8): 1506-1510.
- Stone JH, et al: Trial of Tocilizumab in Giant-Cell Arteritis. New England Journal of Medicine 2017; 377(4): 317-328.
- Hosoya T, et al: Novel treatment strategy of polymyalgia rheumatica targeting drug-free remission. Clin Exp Rheumatol 2021; 39(3): 701-702.
- Marsman DE, et al: Efficacy of rituximab in patients with polymyalgia rheumatica: a double-blind, randomized, placebo-controlled, proof-of-concept trial. Lancet Rheumatol 2021; 3(11): E758-E766.
- Horvath L, Hellmich B. Therapy of giant cell arteritis and polymyalgia rheumatica. Z Rheumatol 2020; 79(2): 175-185.
- Bonelli M, et al: Tocilizumab in patients with new onset polymyalgia rheumatica (PMR-SPARE): a phase 2/3 randomized controlled trial. Ann Rheum Dis 2022; 81(6): 838-844.
- Swissmedic: Medicinal product information, www.swissmedic.ch,(last accessed 23.07.2024).
- Dejaco C, et al: 2015 Recommendations for the management of polymyalgia rheumatica: a European League Against Rheumatism/American College of Rheumatology collaborative initiative. Ann Rheum Dis 2015; 74(10): 1799-1807.
- Fruth M, et al: MRI of shoulder girdle in polymyalgia rheumatica: inflammatory findings and their diagnostic value. RMD Open 2024 May 9; 10(2): e004169.
HAUSARZT PRAXIS 2024; 19(8): 38-39 (published on 22.8.24, ahead of print)