RSV is a common pathogen not only in older seniors over 65 years of age, but also in middle-aged patients between 50 and 64 years of age. In older adults hospitalized with lower respiratory tract infection, diabetes mellitus (DM) is a common comorbidity, but little information is available on the impact of DM on disease severity, and the mechanisms of any interaction are poorly understood.
Lower respiratory tract infections (L RTIs) cause significant morbidity and mortality in both adults and children. In 2019, there were more than 500 million LRTI infections worldwide, and more than 2 million LRTI-related deaths were recorded in 2016. These deaths include more than 650,000 children under the age of five and more than one million seniors over the age of 70.
The etiologic factors for LRTIs can be bacterial, viral or fungal. Among viral infections, influenza (A or B) and respiratory syncytial virus (RSV) are among the most common causes of viral LRTIs during typical (i.e. non-pandemic) endemic seasons, in addition to coronavirus. Influenza causes an estimated one billion infections, RSV causes hundreds or tens of millions of acute respiratory infections worldwide each year. RSV-related LRTIs can lead to ICU admission and death, comparable to those caused by influenza. The risk of severe RSV disease increases with age and the presence of comorbidities.
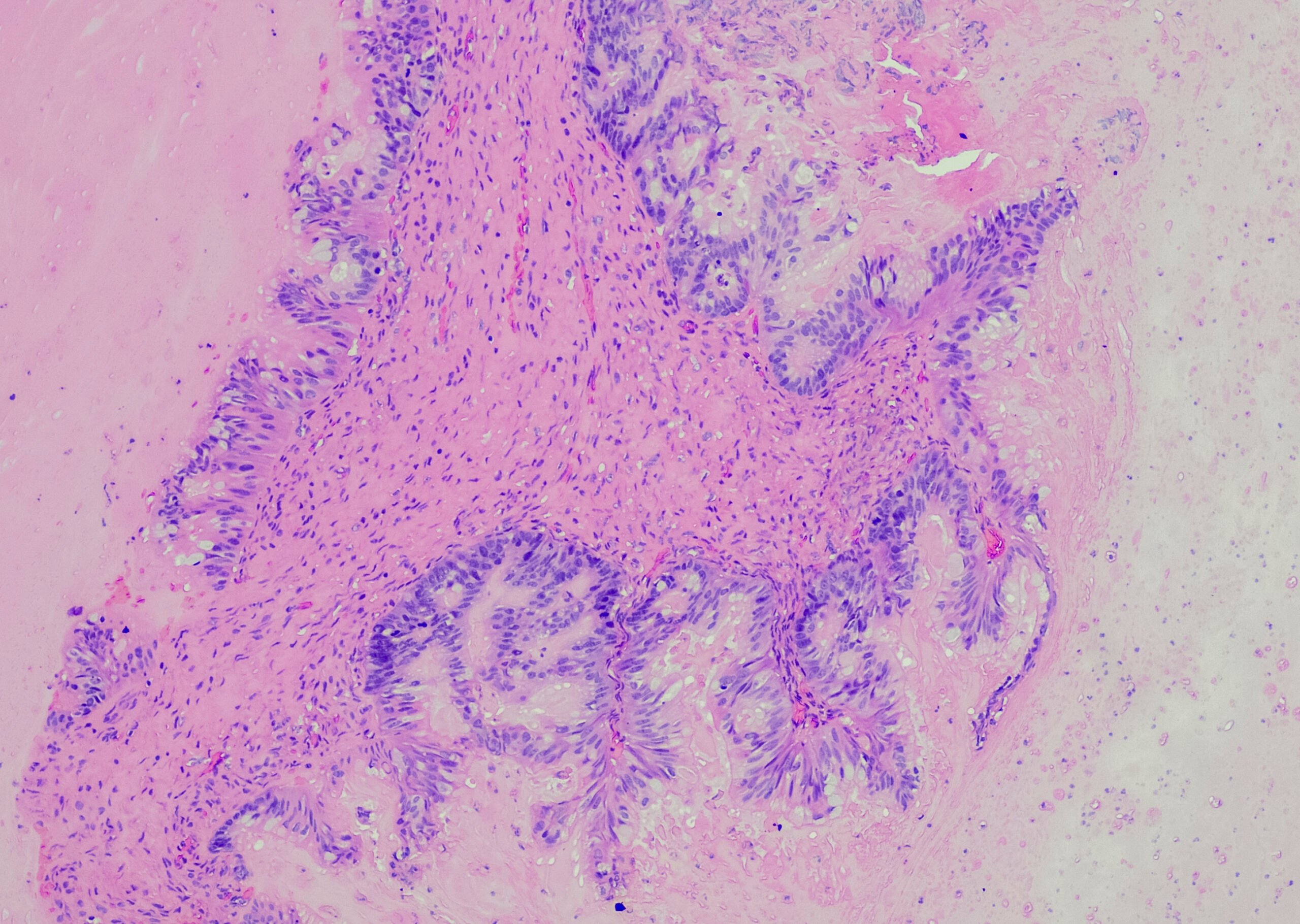
Dr. Hakan Sivgin from the Department of Internal Medicine at Tokat University Faculty of Medicine in Turkey and colleagues retrospectively analyzed 46 Turkish patients infected with respiratory syncytial virus and provided information on their comorbidities, co-infection status and symptoms [1]. Patients were categorized into four levels of severity, from mild to severe, depending on the degree of infiltration of the lung parenchyma and oxygen levels. Their work focused, among other things, on the impact of diabetes as a common chronic disease on patients with RSV and the joint impact of diabetes and superbacterial infection on the severity of LRTI.
Comorbidities, coinfection and age in association with RSV severity
All patients were negative for SARS-CoV-2 infection at enrollment. Patients diagnosed with lower respiratory tract infection, pneumonia or respiratory insufficiency were enrolled in the study within 48 hours of hospitalization. Nasal samples were collected from all participants by swabbing the turbinates with a cotton swab for 5 seconds. Reverse transcription polymerase chain reaction (RT-PCR) was performed on the samples within 24 hours of collection. Those patients (n=46) who were infected with RSV according to the PCR result were included in the analysis.
The average age of the patients was 53 years. Chronic diseases such as diabetes, heart failure, hypertension, co-infections of any kind, bacterial co-infections and age were associated with the severity of the disease. Cough was the most common symptom (89%), followed by fever (26%) and muscle pain, dyspnea and weakness (about 20%).
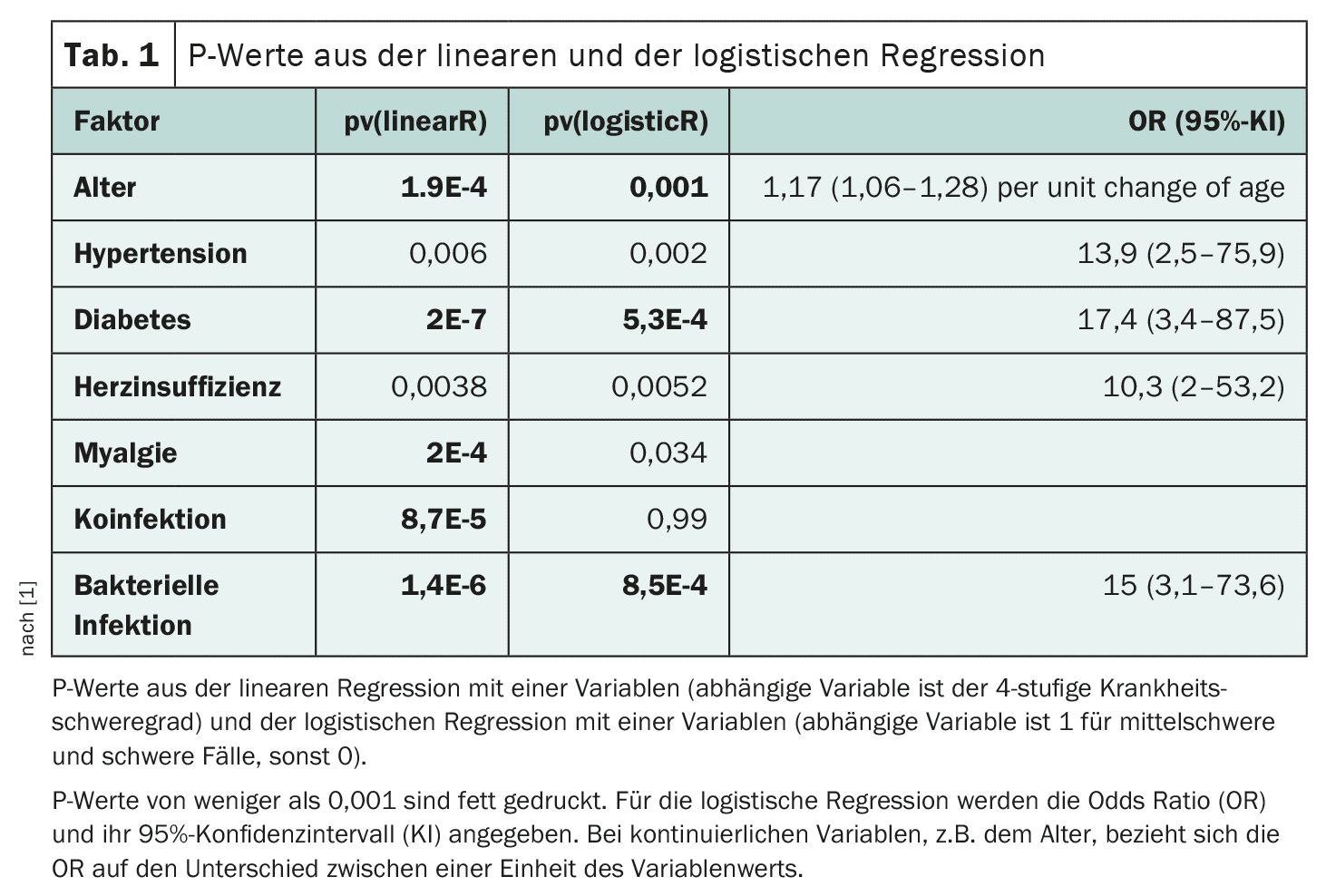
To identify all factors or symptoms associated with disease severity, two regressions were performed. The first was linear, assuming a numerical value of 0, 1, 2 or 3 for mild-a, mild-b, moderate-b and severe patients, respectively. The other was a logistic regression with a binary severity level, 0 for mild-a and mild-b and 1 for moderate and severe (Table 1). Although it is possible to use a binary severity with the severe cases in one group and the others in another, no statistically significant results were obtained at the p=0.01 level due to the small sample size in the severe group (n=5), according to the authors.
Of the pre-existing conditions, hypertension, diabetes and heart failure were associated with more severe disease, whereas asthma, chronic kidney disease and heart disease were not. All patients with severe disease (n=5) had muscle pain (myalgia), but none of the moderately ill patients (n=7) had this symptom. Although 39% of patients with mild-a infection had coinfection (11 of 17), 100% of patients with mild-b, moderate and severe infection had coinfection. In the mild-a and mild-b cases, 12% had a bacterial infection, while the proportion was 67% in the moderate and severe cases.
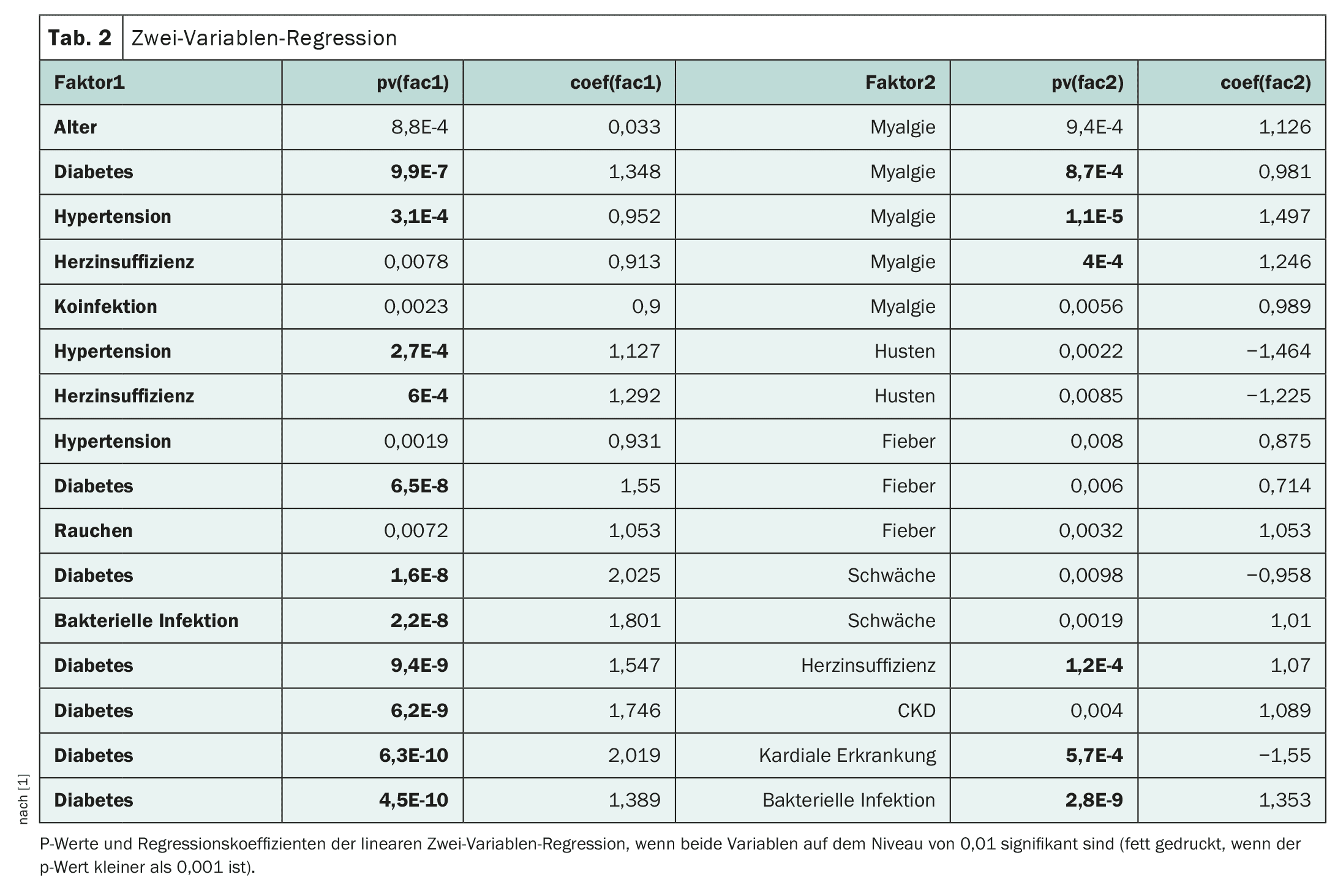
Joint contribution of diabetes and another disease
Linear regression was performed to investigate which two variables contribute independently to disease severity. Three interesting pairs of risk factors are worth mentioning, diabetes and heart failure, diabetes and heart disease, and diabetes and bacterial infections, according to the authors (Table 2). However, the interaction between diabetes and other diseases is different in these situations. In patients who had both heart disease and diabetes, the most severe situation was avoided (0 out of 4). Patients who had both heart failure and diabetes all ended up in the severe cases (3 out of 3), although two other patients with only one condition also ended up severely ill. Patients who had both diabetes and bacterial infection (n=5, aged between 50 and 73 years) were all in the severe group, and patients with only one condition (either diabetes or bacterial infection, not both) avoided the severe situation completely (0 out of 16).
As reported in a number of previous studies, not only heart failure or cardiovascular disease, but also diabetes and hypertension are serious risk factors in patients with RSV, Dr. Sivgin and colleagues explain. During the COVID-19 pandemic, chronic diabetes was not thought to be as strong a risk factor for severe disease as acute hyperglycemia or new-onset diabetes. However, according to Dr. Sivgin, their study did not provide the data needed to examine the impact of chronic versus acute hyperglycemia on disease severity in RSV-infected patients.
However, a potentially interesting finding was that all critically ill patients included in the study (n=5) had both diabetes and bacterial infection, and vice versa. This 100 percent concordance could be a chance event of their relatively small data set, but it leads to a significant two-variant regression (with diabetes and bacterial infection as two variables) for both variables, the authors point out (Table 2). If diabetes or co-infection is not an independent cause of RSV disease severity, then only one of the variables would be significant, not the other. One assumption could be that diabetics experience a threefold exacerbation after infection with RSV and bacteria. In addition, the co-significance of diabetes and bacterial infection for the severity of RSV disease persists even when sex and age are included in the multiple regression, according to the authors.
Diabetes is a highly significant risk factor for the severity of RSV disease. It was also found that even in middle-aged RSV patients, a history of diabetes and co-infection with bacteria can be a combination influencing the severity of the disease. This information should be useful for the management and treatment of RSV patients. The authors emphasize that while more samples are needed to independently validate these findings, their analysis suggests that the sample size was large enough to detect the observed signal and that there may be clues as to where precautions could be taken to save lives.
Literature:
- Sivgin H, Cetin S, Ulgen A, Li W: Diabetes and bacterial co-infection are two independent risk factors for respiratory syncytial virus disease severity. Front Med (Lausanne) 2023; 10: 1231641; doi: 10.3389/fmed.2023.1231641.
InFo DIABETOLOGY & ENDOCRINOLOGY 2024; 1(3): 22-23