Pulmonary emphysema is often referred to as the “end stage” of COPD. Hyperinflation is a significant component of respiratory distress in affected patients. Lung volume reduction is an effective treatment for patients with emphysema and hyperinflation.
Reducing the volume of a diseased organ seems counterintuitive at first, even reckless or dangerous. However, with appropriate knowledge of the pathophysiology of emphysema, the idea and effect of lung volume reduction (LVR) is almost ingenious and was a pioneering procedure just a few decades ago. In order to understand the principle of action of LVR, a short excursion into propaedeutics is necessary.
Pulmonary emphysema is often referred to as the “end stage” or “extreme form” of chronic obstructive pulmonary disease (COPD). In a narrower sense, COPD itself is initially a chronic inflammatory respiratory disease that leads to chronic (possibly productive) cough and dyspnea with increasing airway obstruction. The most important prophylactic and therapeutic intervention is a consistent cessation of smoking, since tobacco smoking, in addition to chronic bronchitis, leads to irreversible destruction of the alveoli with loss of the elastic restoring forces of the lungs. This results in dynamic and static pulmonary hyperinflation, which can be measured bodyplethysmographically by increased residual volume (RV) [1]. Hyperinflation in emphysema is a definitive component of dyspnea. This realization led to initial efforts in the 1950s to reduce hyperinflation by LVR, with the goal of improving dyspnea [2]. Finally, thanks to the National Emphysema Treatment Trial (NETT), invasive treatment in the form of LVR is now part of the established therapy for emphysema, as it can significantly improve quality of life as well as first-second capacity (FEV1) and 6-minute walking distance [3]. In suitable candidates, FEV1 can be improved by approximately 100-600 ml. The 6-minute walking distance as an objectifiable measure of physical endurance improves by approximately 50-100 meters after LVR. Individual studies have even demonstrated an increase in survival time. Meanwhile, both surgical and bronchoscopic LVR with endobronchial valves, coils, or water vapor are among the official treatment recommendations of the Global Initiative of Chronic Obstructive Lung Disease (GOLD) for advanced emphysema [4]. However, in addition to the basic requirements mentioned in part above, various criteria must be met when evaluating a suitable LVR procedure, depending on the method. This article is intended to provide the reader with an overview of the procedures, requirements, and effectiveness of an LVR.
Active principle of lung volume reduction
The lung overinflation, which in turn is a consequence of the loss of elastic restoring forces as well as bronchial obstruction, leads to a flattening and loss of function of the diaphragm, the most important respiratory muscle, which in healthy individuals performs approx. 80% of the respiratory work. This leads to progressive failure of the respiratory muscle pump. In addition, overdistended (destroyed) portions of the lungs increasingly compress less affected areas of the lung, which leads to another component, namely the so-called distribution disorder (ventilation-perfusion mismatch). And thirdly, overinflation during expiration leads to compression of the airways, which in turn promotes overinflation in the sense of a vicious circle. Through the removal resp. elimination of an overinflated lung area, a “decompressive effect” is achieved, which counteracts the three pathological mechanisms mentioned above and often improves the patient’s respiratory distress abruptly and, above all, sustainably.
Basic prerequisite for lung volume reduction
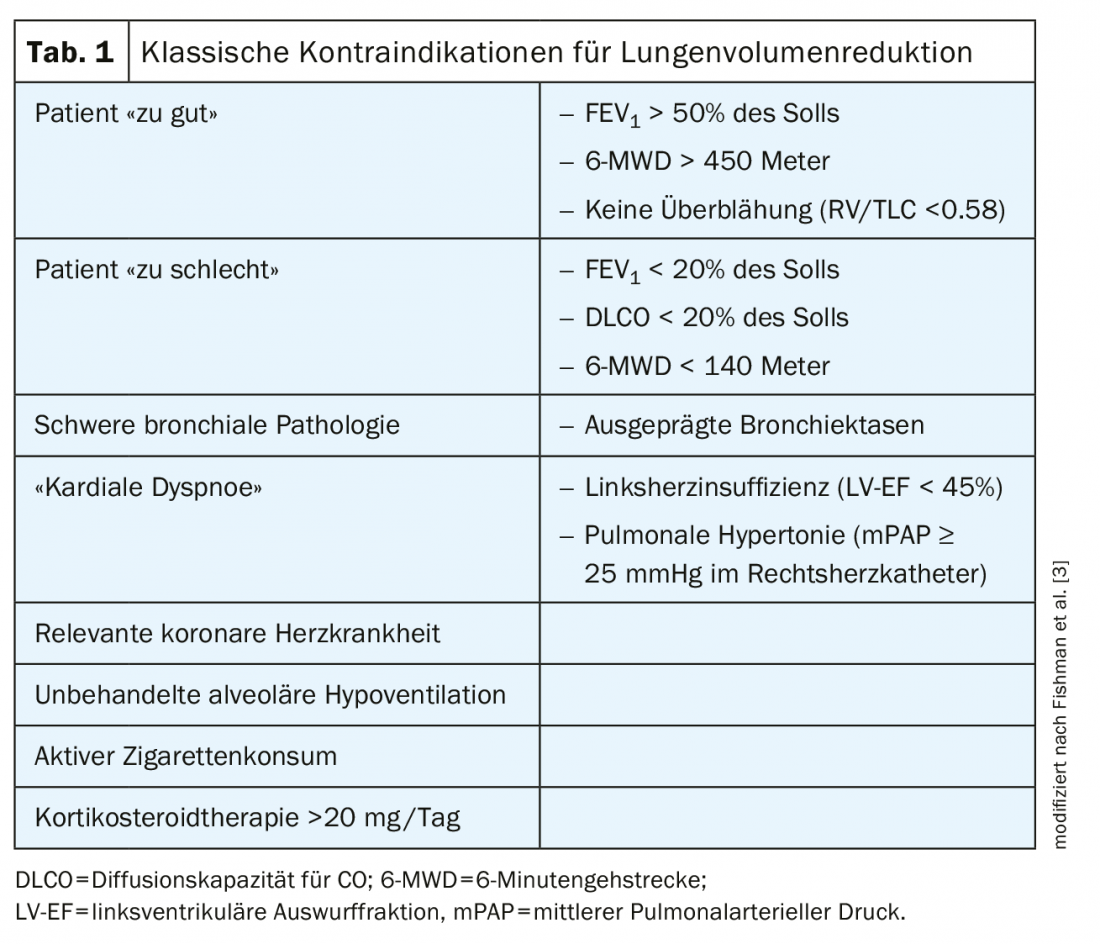
When evaluating an LVR, the first step – regardless of the method – is to determine whether a patient is suitable in principle for such a procedure. The criteria and indications/contraindications used are essentially based on the inclusion and exclusion criteria of the NETT [3], which were largely adopted in the subsequent studies of bronchoscopic LVR methods (valves, coils, steam). (Tab.1). The most basic requirements for LVR are an established baseline COPD therapy including smoking cessation according to GOLD recommendations [4] as well as a bodyplethysmographically measurable hyperinflation (RV >175% of target, RV/TLC 0.58). The presence of clinical (e.g., barrel chest) or radiologic (e.g., flattened diaphragm on conventional radiograph) features of hyperinflation may further emphasize the decision to perform LVR [5]. In addition, a relevant cardiac (or other) cause of dyspnea should be ruled out with appropriate workup and treated upstream of LVR. The patient should be neither too well (e.g., FEV1 >50% of target) nor too poor (e.g., FEV1 <15% of target) before LVR. In the first case, the patient would probably not benefit significantly from LVR, whereas otherwise an increased periinterventional/perioperative morbidity and mortality risk should be expected. However, it must be clearly emphasized that some of these traditional contraindications from Table 1 have been challenged in recent years and are no longer considered a clear dividing line. However, deviations from the classic contraindications should definitely be in the hands of specialists with relevant experience with LVR.
Surgical lung volume reduction
Surgical lung volume reduction (LVRS) is usually performed thoracoscopically (keyhole surgery). Patients are hospitalized for an average of 10-12 days for this. With adequate patient selection, significant improvement in quality of life, physical performance, and pulmonary function can be achieved [6,7]. In addition, the risk of future COPD exacerbations has been shown to decrease postoperatively [8]. These beneficial effects can last up to five or more years postoperatively [6]. After pulmonary function values and symptoms have returned to preoperative levels, repeat LVRS or, more recently, bronchoscopic LVR can be evaluated in selected cases, as this can restore improvement lasting at least one year [9]. Preoperatively, relevant coronary artery disease must be excluded (a.e., with myocardial perfusion scintigraphy). An incidentally discovered round focus suspected of carcinoma is not a contraindication to surgical lung volume reduction. If the suspicious finding is located in an emphysematous target zone, a curative approach can even be achieved with anatomic resection [10]. While one must expect lung function losses with other pulmonary cancer surgeries, this way (“resection in the LVRS concept”) even results in an improvement. Complications after LVRS occur with a frequency of approximately 30% within 30 days. The most common complications are prolonged air fistulas. The published 90-day mortality after LVRS is 5.5% [11]; however, based on our own experience, this number is much lower and is approximately 1%.
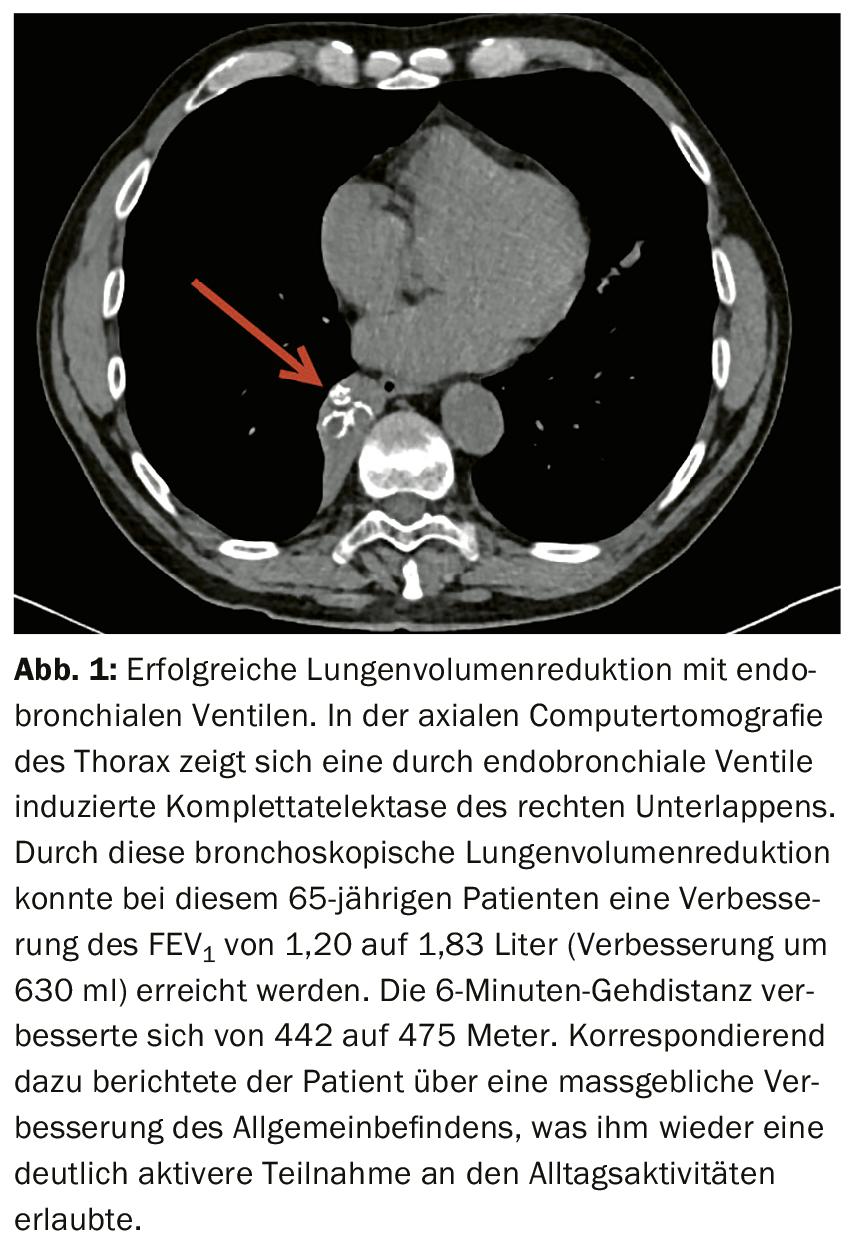
Bronchoscopic lung volume reduction with endobronchial valves.
In bronchoscopic LVR with endobronchial valves (EBV), “deflation” is produced by artificial atelectasis in the valved lung lobe (Fig. 1), with the valves allowing exclusively unidirectional airflow, namely on expiration. The inspiratory airflow can no longer return to the pulmonary lobe due to the valves, thus “venting” the lobe. The positive effect in terms of dyspnea, exercise capacity, and quality of life has been demonstrated in six randomized trials [12–18] and is comparable to LVRS. Significant advantages of EBV treatment are both the minimally invasive nature of the procedure and its reversibility, since valves can usually be removed again without difficulty by bronchoscopy if this is desired or necessary in the course of the procedure. Patients are usually hospitalized for 5-6 days for valve implantation. The most common adverse treatment effect is pneumothorax, which can occur in about 20-30% (usually in the first 24 hours after the procedure).
The crucial prerequisite for successful EBV treatment and the development of atelectasis, respectively, is a lack of collateral ventilation between the treated and adjacent lobe of the lung [19], with bronchiolo-alveolar (Lambert) and interbronchiolar (Martin) connections presumably acting as collateral channels [20]. The presence of collateral ventilation can be measured both with special instruments (“Chartis”) during bronchoscopy or estimated with computed tomographic analysis of the interlobar fissures (“StratX”). If collateral ventilation in the target lobe must be assumed on the basis of the two examinations, treatment with valves is out of the question. In this case, surgical LVR or another bronchoscopic procedure must be chosen. However, it makes perfect sense to always primarily evaluate bronchoscopic LVR with EBV for two reasons. On the one hand, valve treatment has an extremely robust evidence base with seven randomized trials demonstrating efficacy and safety [12–18]. On the other hand, this is a potentially reversible process. A direct comparison of different LVR procedures does not exist to date.
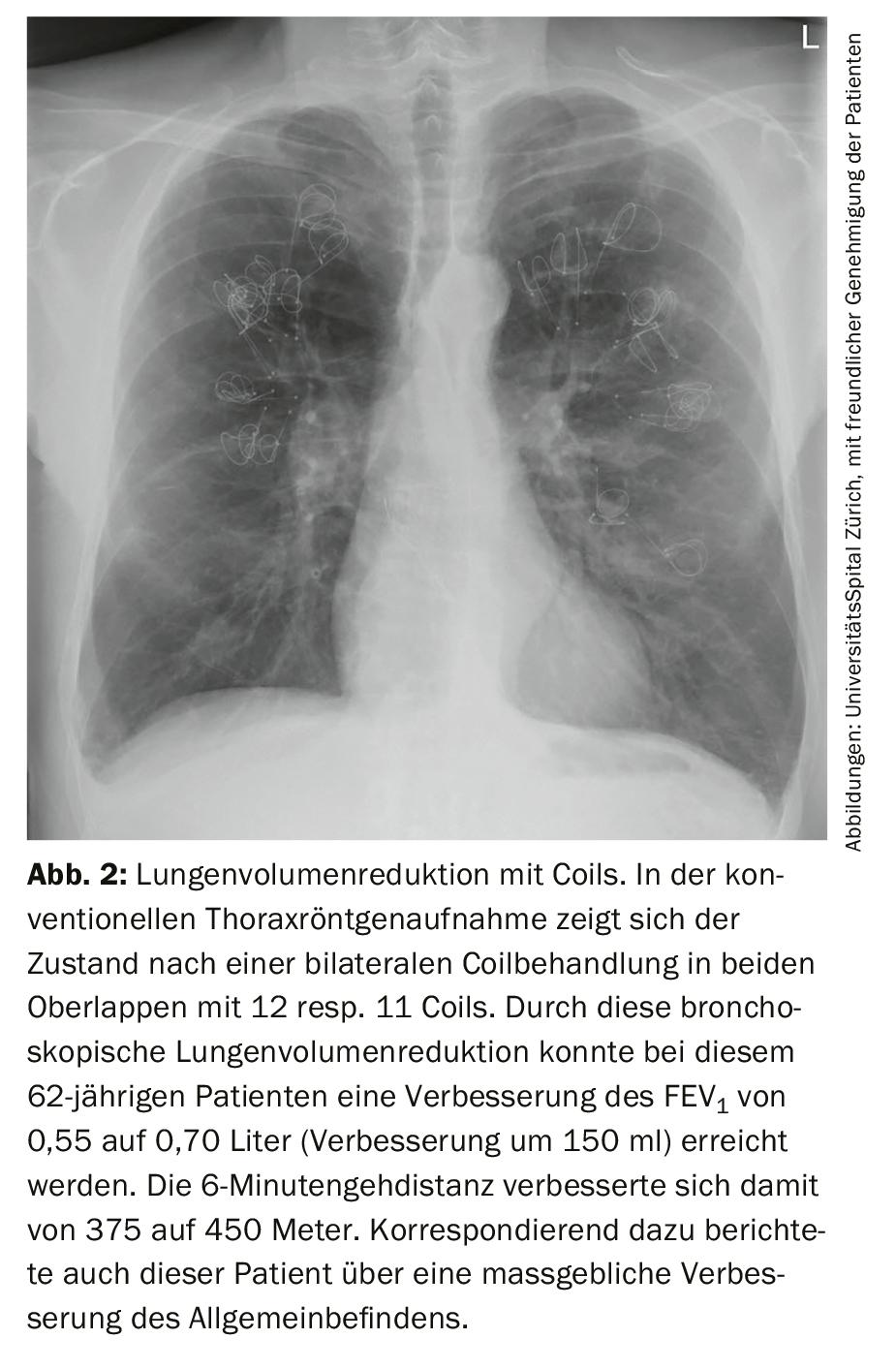
Bronchoscopic lung volume reduction with coils
Coils are highly elastic wire spirals or springs made of nitinol (alloy of nickel and titanium), which are inserted bronchoscopically into one or two lobes of the lung (Fig. 2). As a rule, the treatment is performed in two sessions. 10-14 coils are used per lung lobe. The exact mechanism of action of coils is not known. Coils are thought to contract the lungs while supporting elastic restoring forces that have been largely destroyed in emphysema lungs. The resulting improvement in dyspnea and quality of life has been demonstrated in three randomized trials [21–23]. This procedure also has a very good safety profile; occasionally, transient mild hemoptysis may occur. Coil treatment is independent of collateral ventilation. The important contraindications are severe nickel allergy and already established oral anticoagulation or double platelet antiaggregation. The hospitalization time for coil treatment is 3-5 days.
Bronchoscopic lung volume reduction with water vapor or polymer foam
Steam or polymer foam (AeriSeal®), which is introduced into the diseased lung via a flexible bronchoscope, causes thermally or chemically induced inflammation in the treated lung segments. After a few weeks, localized scarring develops in this area, leading to shrinkage and thus LVR. The efficacy of both procedures has been demonstrated in one randomized trial each [24,25]. The most common adverse effect after these two procedures is an exuberant (systemic) inflammatory reaction with fever, which must be treated with cortisone and macrolide antibiotics. AeriSeal®, which is used for chemical LVR, was no longer available until recently due to financing problems. However, it has since been purchased by another company and can now be used again in a few centers within a registry study. Both procedures are independent of collateral ventilation.
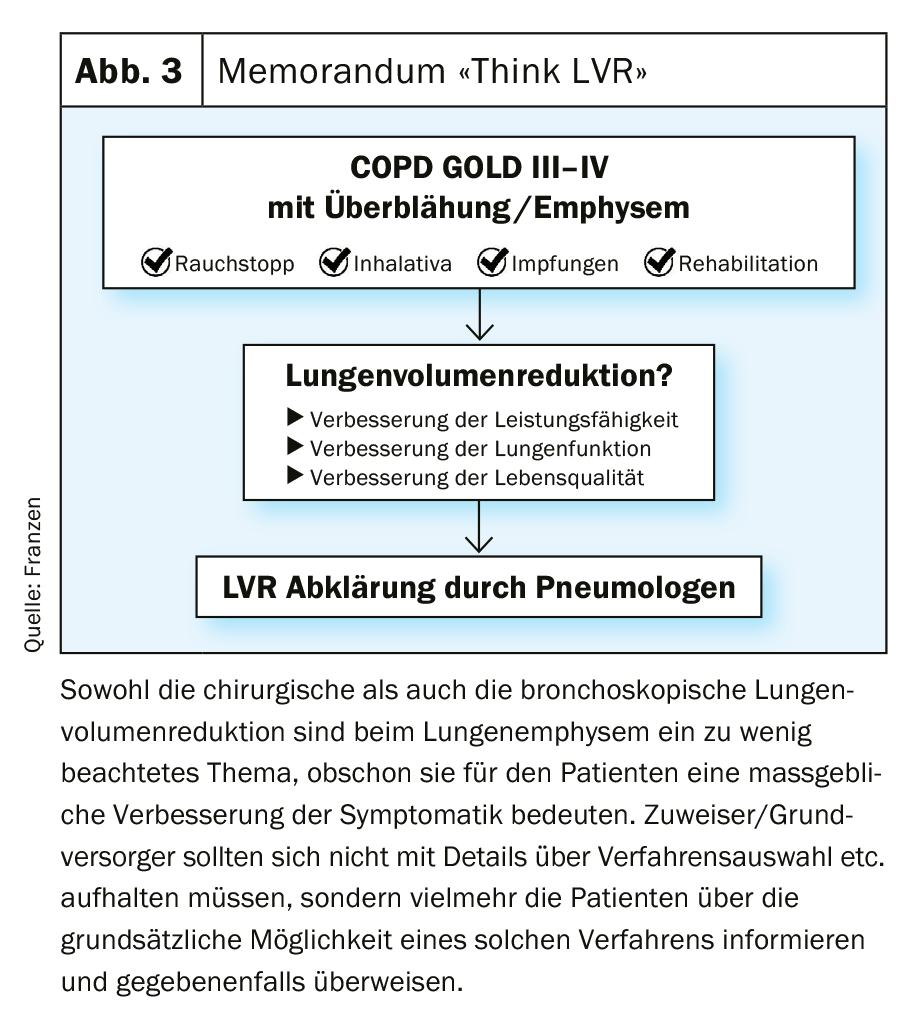
Selection of the best individual lung volume reduction procedure and role of the primary care provider.
Local expertise/infrastructure and individual patient preference should certainly be taken into account when selecting the appropriate LVR procedure. And finally, taking into account these circumstances and diagnostic tools, each case should be discussed at an interdisciplinary conference [26]. However, it is critically important for patients that potential candidates for LVR are referred to an appropriate center of excellence. With this in mind, Figure 3 is intended to be an easy-to-use guide and memorandum for an effective adjunct to emphysema therapy without confusing the referring/primary care provider with details about specific procedures and patient selection.
Take-Home Messages
- Hyperinflation (increased residual volume) is usually a definitive component of respiratory distress in patients with emphysema.
- Lung volume reduction is a very effective treatment for respiratory distress in patients with emphysema and hyperinflation.
- Various bronchoscopic procedures and surgery are available for lung volume reduction. All procedures have a good safety profile. The selection of the most suitable procedure for the individual is mainly based on various clinical, radiological and anatomical criteria.
- At the latest from COPD GOLD III, affected patients should be co-managed by a pulmonologist to evaluate lung volume reduction.
Literature:
- Kemp SV, Polkey MI, Shah PL: The epidemiology, etiology, clinical features, and natural history of emphysema. Thorac Surg Clin 2009; 19: 149-158.
- Brantigan OC, Mueller E: Surgical treatment of pulmonary emphysema. Am Surg 1957; 23:789-804.
- Fishman A, Martinez F, Naunheim K, et al: A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003; 348: 2059-2073.
- Global Strategy of the Diagnosis M, and Prevention of Chronic Obstructive Pulmonary Disease, Global Initiative for Chronic Obstructive Lung Disease (GOLD): https://goldcopd.org 2019
- Straub G, Caviezel C, Frauenfelder T, et al: Successful lung volume reduction surgery in combined pulmonary emphysema and fibrosis without body-plethysmographic hyperinflation-a case report. J Thorac Dis 2018; 10: pp. 2830-2834.
- Tutic M, Lardinois D, Imfeld S, et al: Lung-volume reduction surgery as an alternative or bridging procedure to lung transplantation. Ann Thorac Surg 2006; 82: 208-213; discussion 213.
- Hamacher J, Buchi S, Georgescu CL, et al: Improved quality of life after lung volume reduction surgery. Eur Respir J 2002; 19: 54-60.
- Washko GR, Fan VS, Ramsey SD, et al: The effect of lung volume reduction surgery on chronic obstructive pulmonary disease exacerbations. Am J Respir Crit Care Med 2008; 177: 164-169.
- England DM, Hochholzer L, McCarthy MJ: Localized benign and malignant fibrous tumors of the pleura. A clinicopathologic review of 223 cases. Am J Surg Pathol 1989; 13: 640-658.
- Choong CK, Mahesh B, Patterson GA, et al: Concomitant lung cancer resection and lung volume reduction surgery. Thorac Surg Clin 2009; 19: 209-216.
- Naunheim KS, Wood DE, Krasna MJ, et al: Predictors of operative mortality and cardiopulmonary morbidity in the National Emphysema Treatment Trial. J Thorac Cardiovasc Surg 2006; 131: 43-53.
- Sciurba FC, Ernst A, Herth FJ, et al: A randomized study of endobronchial valves for advanced emphysema. N Engl J Med 2010; 363: 1233-1244.
- Herth FJ, Noppen M, Valipour A, et al: Efficacy predictors of lung volume reduction with Zephyr valves in a European cohort. Eur Respir J 2012; 39: 1334-1342.
- Davey C, Zoumot Z, Jordan S, et al: Bronchoscopic lung volume reduction with endobronchial valves for patients with heterogeneous emphysema and intact interlobar fissures (The BeLieVeR-HIFi trial): study design and rationale. Thorax 2014
- Klooster K, Ten Hacken NH, Hartman JE, et al: Endobronchial Valves for Emphysema without Interlobar Collateral Ventilation. N Engl J Med 2015; 373: 2325-2335.
- Valipour A, Slebos DJ, Herth F, et al: Endobronchial Valve Therapy in Patients with Homogeneous Emphysema. Results from the IMPACT Study. Am J Respir Crit Care Med 2016; 194: 1073-1082.
- Kemp SV, Slebos DJ, Kirk A, et al: A Multicenter Randomized Controlled Trial of Zephyr Endobronchial Valve Treatment in Heterogeneous Emphysema (TRANSFORM). Am J Respir Crit Care Med 2017; 196: 1535-1543.
- Criner GJ, Sue R, Wright S, et al: A Multicenter Randomized Controlled Trial of Zephyr Endobronchial Valve Treatment in Heterogeneous Emphysema (LIBERATE). Am J Respir Crit Care Med 2018; 198: 1151-1164.
- Herth FJ, Eberhardt R, Gompelmann D, et al: Radiological and clinical outcomes of using Chartis to plan endobronchial valve treatment. Eur Respir J 2013; 41: 302-308.
- Gompelmann D, Eberhardt R, Herth FJ: Collateral ventilation. Respiration 2013; 85: 515-520.
- Sciurba FC, Criner GJ, Strange C, et al: Effect of Endobronchial Coils vs Usual Care on Exercise Tolerance in Patients With Severe Emphysema: The RENEW Randomized Clinical Trial. Jama 2016; 315: 2178-2189.
- Shah PL, Zoumot Z, Singh S, et al: Endobronchial coils for the treatment of severe emphysema with hyperinflation (RESET): a randomised controlled trial. Lancet Respir Med 2013; 1: 233-240.
- Deslee G, Klooster K, Hetzel M, et al: Lung volume reduction coil treatment for patients with severe emphysema: a European multicentre trial. Thorax 2014; 69: 980-986.
- Shah PL, Gompelmann D, Valipour A, et al: Thermal vapor ablation to reduce segmental volume in patients with severe emphysema: STEP-UP 12 month results. Lancet Respir Med 2016; 4: e44-e45.
- Come CE, Kramer MR, Dransfield MT, et al: A randomised trial of lung sealant versus medical therapy for advanced emphysema. Eur Respir J 2015; 46: 651-662.
- Oey I, Waller D: The role of the multidisciplinary emphysema team meeting in the provision of lung volume reduction. J Thorac Dis 2018; 10: pp. 2824-2829.
InFo PNEUMOLOGY & ALLERGOLOGY 2019; 1(1): 6-9.











