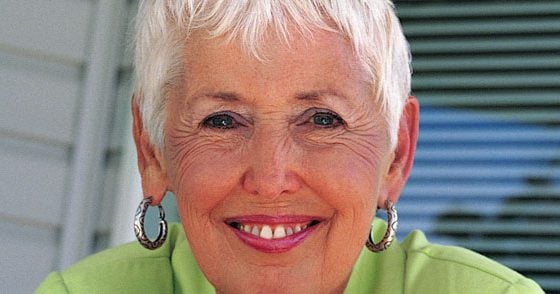
While the calcium supply in Switzerland is usually ensured to a large extent through the diet, vitamin D deficiency is common. How this deficiency can be compensated for and in which cases calcium supplementation is indicated are topics on which Prof. Dr. med. Heike Bischoff-Ferrari, Center for Ageing and Mobility, University of Zurich and Waid City Hospital, comments in the following interview.
Prof. Bischoff-Ferrari, why is it important to ensure an adequate supply of both calcium and vitamin D?
Prof. Bischoff-Ferrari:
Calcium is known to be an important building block of bones. Vitamin D promotes calcium absorption from the intestine and also has a direct, strengthening effect on the muscles. Current data indicate that vitamin D plays the more important role in this partnership. It is now known that every third person over 65 falls once a year, and over 80 already every second. Studies show that 800 IU of vitamin D per day can prevent one in three falls [1] and one in three hip fractures [2], especially in the elderly. To be able to achieve such positive results with such a low-cost strategy as vitamin D supplementation is of great importance.
What does the supply of vitamin D and calcium look like in Switzerland?
Prof. Bischoff-Ferrari:
If the vitamin D level in the blood is determined – the 25(OH)-vitamin D is measured – it is found that about 50% of the population is undersupplied. The main risk group here is older people over the age of 60. The reason for this is that our skin produces about a factor of 4 less vitamin D in response to sun exposure in old age than it does in younger years. In addition, older people do not like to be in the blazing sun. For this reason, the Federal Office of Public Health has formulated a recommendation of 800 IU per day in its new guidelines for people over 60. This recommendation should ensure prevention of vitamin D deficiency and reduce the risk of falls and fractures. And since 800 IU of vitamin D can be used safely for years, it makes sense to start supplementing even the slightly younger ones.
With regard to calcium, we in Switzerland are relatively well supplied through our diet, as we have good, calcium-rich foods such as dairy products and mineral water. With a balanced diet and, for example, one slice of hard cheese or one glass of milk per day, the calcium supply can be largely ensured. Alternatively, a calcium supplement should be considered, but we now always recommend this in combination with vitamin D. This is because calcium supplements alone, without vitamin D, do not reduce fracture risk. On the contrary, they even increase the risk of hip fractures by 64% [3]. This is probably because calcium carbonate and citrate – which are the common forms of calcium in supplements – inhibit the absorption of phosphate, which is particularly relevant in older people, who are often also phosphate deficient. In addition to calcium, the bone also needs phosphate, since a calcium phosphate product is incorporated. Vitamin D promotes both calcium and phosphate absorption.
The new findings on the cardiovascular risk of a high calcium intake in supplement form have also led to a reconsideration of the previous recommendation for calcium supplementation at 1000 mg per day, and today rather the first thing to find out is how well the calcium supply is already ensured through the diet. And given that everyone manages a calcium intake of about 500 mg through diet, a maximum of another 500 mg should be supplemented. That’s why you now see new product combinations of 800 IU of vitamin D per day with a maximum of 500 mg of calcium per day.
When is supplementation with vitamin D and calcium necessary or recommended?
Prof. Bischoff-Ferrari
The recommendations of the FOPH refer primarily to vitamin D. They say that with minimal sun exposure, in winter, with consistent sun protection and generally from the age of 60, a daily vitamin D intake of 800 IU should be ensured, and 600 IU for younger people. A minimal amount of it can be supplied through the diet. The total vitamin D requirement cannot be met even with the healthiest diet. Our primary source of vitamin D is the sun, but this is not a reliable source because consistent sun protection is recommended precisely for reasons of skin cancer prevention. Calcium supplementation is recommended in those cases where dietary supply is not ensured. So, for example, for people who do not like or tolerate dairy products and do not drink mineral water.
What is the role of calcium and vitamin D supplements in patients with osteoporosis?
Prof. Bischoff-Ferrari:
Here, too, vitamin D represents a basic therapeutic agent, since one often sees a massive vitamin D deficiency, especially in osteoporosis patients. However, data show that bisphosphonate therapy, for example, is less successful, i.e., the risk of recurrence of fracture is higher, if vitamin D supply is not ensured. Ensuring adequate calcium intake also represents an important pillar, not only of prevention, but also of therapy of osteoporosis, and the newly reconsidered reduced dosage of calcium supplements also comes into play here.
What is the easiest way to supplement calcium and vitamin D?
Prof. Bischoff-Ferrari:
On the one hand, the recommended 800 IU vitamin D can be supplied via vitamin D monopreparations. This is possible in patients who are already adequately supplied with calcium through their diet. If the calcium supply is not guaranteed, a combination preparation is ideally used that contains a maximum of 500 mg of calcium in addition to the 800 IU vitamin D.
Interview: Dr. Therese Schwender
Literature:
- Bischoff-Ferrari HA, Willett WC, Orav EJ, Kiel DP, Dawson-Hughes B. Re: Fall prevention with vitamin D. Clarifications needed. http://wwwbmjcom/content/339/bmjb3692?tab=responses (accessed Feb132012) 2011.
- Bischoff-Ferrari HA, et al: A pooled analysis of vitamin D dose requirements for fracture prevention. N Engl J Med 2012; 367: 40-49.
- Bischoff-Ferrari HA, Dawson-Hughes B, Baron JA, et al: Calcium intake and hip fracture risk in men and women: a meta-analysis of prospective cohort studies and randomized controlled trials. Am J Clin Nutr 2007; 86: 1780-1790.
FAMILY DOCTOR PRACTICE 2013; 4: 24-25