Purpose: This multicenter controlled observational study investigates α-synuclein immunoreactivity at the enteric nervous system in patients with idiopathic REM sleep behavior disorder (iRBD) and controls as a possible biomarker for prodromal parkinsonian syndrome.
Background
Longitudinal studies suggest that REM sleep behavior disorders are a prodromal stage for subsequent Parkinson’s disease in up to 80% of cases. Other biomarkers for prodromal parkinsonian syndromes include hyposmia, impaired color vision, presynaptic dopamine transporter deficit in the putamen, and hyperechogenicity of the substantia nigra on transcranial ultrasound. The aim is to detect prodromal Parkinson’s syndromes as early as possible in order to be able to conduct studies on disease prevention in the future.
Patients and methodology
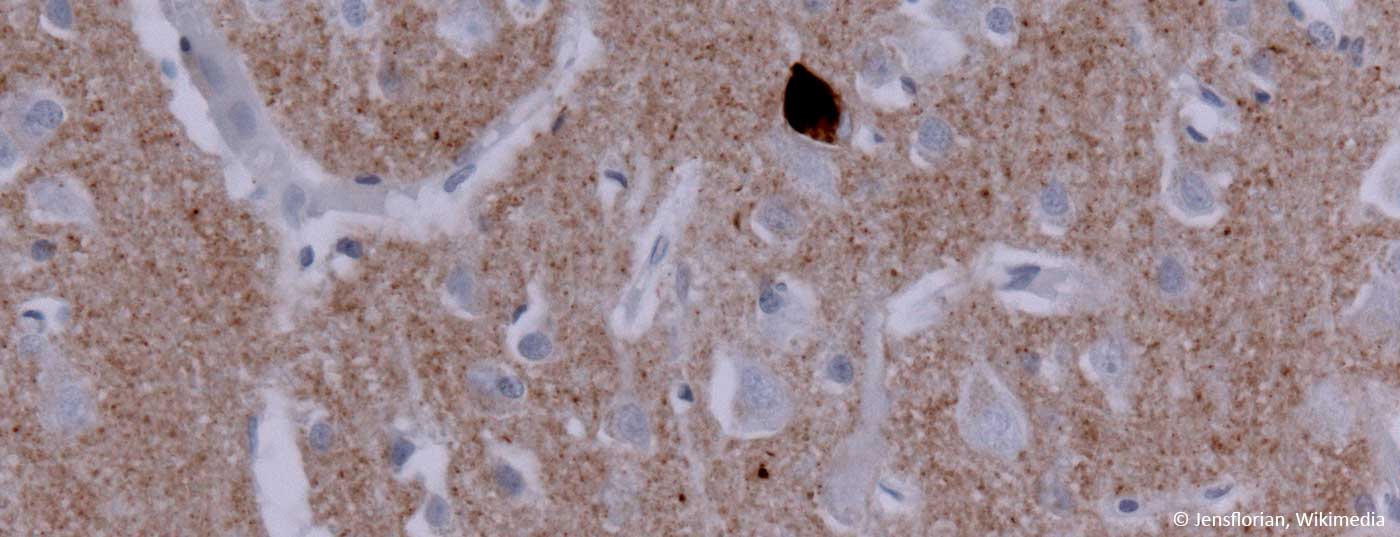
The multicenter controlled observational study included 20 patients with polysomnographically confirmed iRBD, 24 patients with Parkinson’s disease according to the UK Parkinson’s Disease Society Brain Bank diagnostic criteria, and 22 healthy controls. Colon biopsies were taken from all of them. In addition to olfaction (UPSIT and Sniffin’ Sticks) and possible parkinsonian symptoms (MDS-UPDRS parts I-III), biopsies were examined immunohistochemically for phosphorylated and nonphosphorylated α-synuclein.
Results
Compared with the control group and iRBD patients, PD patients had significantly higher scores in MDS-UPDRS, as expected. The sense of smell was significantly reduced in both Parkinson’s and iRBD patients. While all biopsies contained sufficient amounts of mucosa for further analysis, with regard to submucosa, this was the case only in 16 controls, 21 PD and 17 iRBD patients. Non-phosphorylated α-synuclein was detected in the submucosa of all patients and controls. In the mucosa, phosphorylated α-synuclein could not be detected in any group. In the submucosa, phosphorylated α-synuclein was found in four of 17 iRBD patients, but in one of 19 PD patients, but in none of the control group, but without reaching the significance level.
Conclusions of the authors
Considering further work, it is concluded that antibodies directed against non-phosphorylated (native) α-synuclein have no value as biomarkers for prodromal parkinsonian syndromes. Although no significant difference was found, the detection of phosphorylated α-synuclein in four of 17 iRBD patients and none of the controls is interpreted by the authors as possible evidence for a relevant difference. However, it remains unclear why this can no longer be detected in Parkinson’s patients. A connection with a possible nerve cell loss in the course of the disease is discussed. Other complicating factors in performing these and similar studies include different techniques and targets of the antibodies used.
Comment
The early correct diagnosis of Parkinson’s disease is not only important in clinical routine (here it is particularly important to distinguish it from other atypical forms), but is also particularly important in current scientific questions of disease prevention and causal influence on the course of the disease. Thus, the search for suitable biomarkers is directly related to the search for causal therapeutic options. The early manifestation of α-synucleinopathy in the gastrointestinal system would also be consistent with the hypothesis that the disease originates there and spreads via the vagus nerve to the brainstem and then to the other brain regions.
InFo NEUROLOGY & PSYCHIATRY 2016; 14(2): 33.