At the European Cancer Congress in Vienna, there were new insights into the possible etiology of Hodgkin’s lymphoma. In addition, a comprehensive European comparison of cancer care was presented. In metastatic melanoma, two questions were answered: To what extent do patients with poor prognostic factors benefit from combined immunotherapy? And how should the current survival data from the COMBI-v trial be interpreted?
To better explore the etiology of Hodgkin lymphoma (HL) in children and young adults, an English team studied 621 registry cases of HL in patients aged 0 to 24 years (years 1968-2003). 247 of these were of the nodular sclerosing subtype, 105 were of the mixed type, 58 were lymphocyte-rich HL (type with best outcome), 68 fell into the “other” category, and 143 were in the “not further specified” category.
Overall, there were more male HL patients. This was also true for the nodular sclerosing HL subtype, with 130 males vs. 117 females affected. Interestingly, however, there was an age-related change in the gender ratio here: women predominated in the 20-24 age group (72 vs. 55 persons). Among young men, age-specific rates were 14.26 (per million persons/year), whereas the corresponding figure for young women was 18.79.
In addition to gender, deprivation played a role. The researchers defined these using four factors: Households with a high density of people, unemployment, no home ownership, households without a car. Deprivation was remarkably associated with lower incidence rates of the nodular sclerosing subtype. With each 1% increase in the “person density in the household” factor, there was a significant 12% reduction in risk (RR 0.88; 95% CI 0.82-0.94). A reverse trend was seen for the types not further specified. Here, the RR was 1.17. In the other subtypes, deprivation did not exert an influence on incidence.
How can the results be explained?
The data are revealing in several respects. On the one hand, the reversal in the sex ratio could be explained by hormonal factors that play a role during female puberty – including estrogens. It is possible that the etiology of the nodular sclerosing subtype is related to female hormonal changes in addition to other factors. This could be the reason why in females the incidence increases after puberty. Many genes are directly (but also indirectly) regulated by sex hormones.
The lower incidence of this subtype in crowded households may also suggest an etiologic environmental factor. Where people live close to each other, more infectious agents are present. Individuals who are exposed to various pathogens at a young age and undergo multiple infections may develop a stronger immune system that is better able to respond to future infections and cancerous cells in young adulthood. This is an advantage in the HL area. Individuals with genetic susceptibility to HL who live in large-scale conditions during childhood and experience fewer infections would, according to this theory, be more susceptible to the subtype later because their immune systems are less developed. According to the authors, the reversal of the trend in the unspecified types is more difficult to explain, but could also be a coincidence.
Care for cancer patients in Europe
EUROCARE, the largest population-based cancer registry study in Europe, has been ongoing since the late 1990s. New results with cross-national implications were presented at the congress. Data from more than ten million cancer patients aged over 15 years from 29 European countries and a total of 107 registries were analyzed with regard to 5-year survival, among other factors. This was adjusted for deaths from causes other than cancer and for age differences. Diagnoses up to 2007 were included.
Overall, survival rates are low in Eastern Europe, but high in Northern and Central Europe. Other geographic differences emerged and are summarized in Table 1 . The most dramatic differences were found in chronic myeloid and lymphocytic leukemia (CML/CLL), follicular and diffuse large B-cell lymphoma, and multiple myeloma. CML showed an average 5-year survival of 53%, but a huge variation in the different age groups. Of all hematologic cancers, regional differences were greatest for CML: 33.4% in Eastern Europe vs. 51-58% in the rest of Europe. Geographic differences were also found for cancers with poor prognosis, such as ovarian, lung, pancreatic, esophageal, and gastric cancers, brain tumors, and Hodgkin’s lymphoma-but were somewhat less pronounced overall.
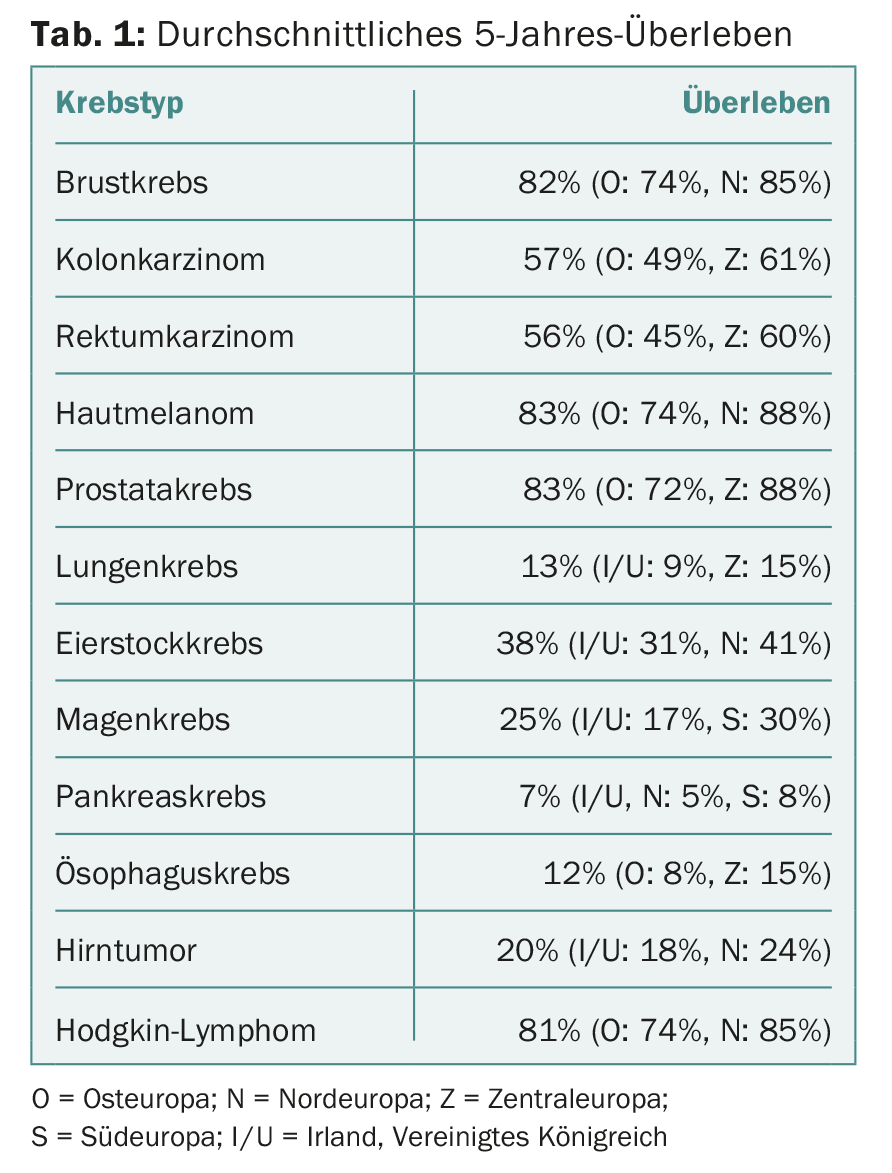
The 5-year survival rates increased throughout Europe over the observation period, especially in Eastern Europe. Specifically, rates increased for breast, cervical, liver, biliary, and head and neck (excluding laryngeal) tumors, for example. The largest increases between 1999-2001 and 2005-2007 were seen in CML (32-54%), prostate (73-82%), and rectal (52-58%) cancers. There was also a slight increase in survival for skin melanomas. Rates remained stable for esophageal, pancreatic, penile, and testicular cancers.
The combined 5-year survival rates of all cancer rates were positively correlated with gross domestic product and total national health expenditures. States with recently higher growth in both parameters had correspondingly higher growth in survival rates. However, this was not always true: countries such as the United Kingdom and Denmark should actually have achieved better rates given their high healthcare spending.
The geographic variations can be explained, among other things, by differences in diagnostic effort or quality and the presence of national screening programs (prostate, breast, colorectal cancer). In addition to early diagnosis, access to multidisciplinary treatments, good quality of care, lifestyle, and health and socioeconomic status of the respective population play an important role in survival. Whether the results will lead to concrete political efforts remains to be seen.
Combination therapies in melanoma continue to convince
CheckMate 067: The CTLA-4 and PD-1 checkpoints are used by cancer cells to override the body’s cancer-specific immune response. Inhibitors can be used to block the checkpoints, which activates the immune system or leads to increased T-cell activity. CheckMate 067 is a phase III trial that compared the PD-1 checkpoint inhibitor nivolumab alone or in combination with the CTLA-4 checkpoint inhibitor ipilimumab to ipilimumab monotherapy. The study population consisted of 945 previously untreated patients with advanced melanoma. The combination was significantly superior to ipilumumab monotherapy in terms of progression-free survival (PFS) and objective response rate. Results of a prespecified subgroup analysis were presented at the ECCO/ESMO Congress: Does the combination remain superior regardless of age, genetic status, or tumor spread? Of particular interest was how patients with poor prognostic factors fared. Subgroups differed with respect to metastases, serum levels of lactate dehydrogenase (LDH), BRAF mutation status, and age.
In the three treatment arms, the above parameters were equally distributed. PFS was 11.5 months (combination) vs. 2.9 months (ipilimumab monotherapy; significant risk reduction of 58%) vs. 6.9 months (nivolumab monotherapy; significant risk reduction of 43%).
The results for the subgroups mentioned are shown in Table 2. Overall, the PFS with the combination was again always longer. Similarly, there were no differences in the safety profile (compared with the overall population).
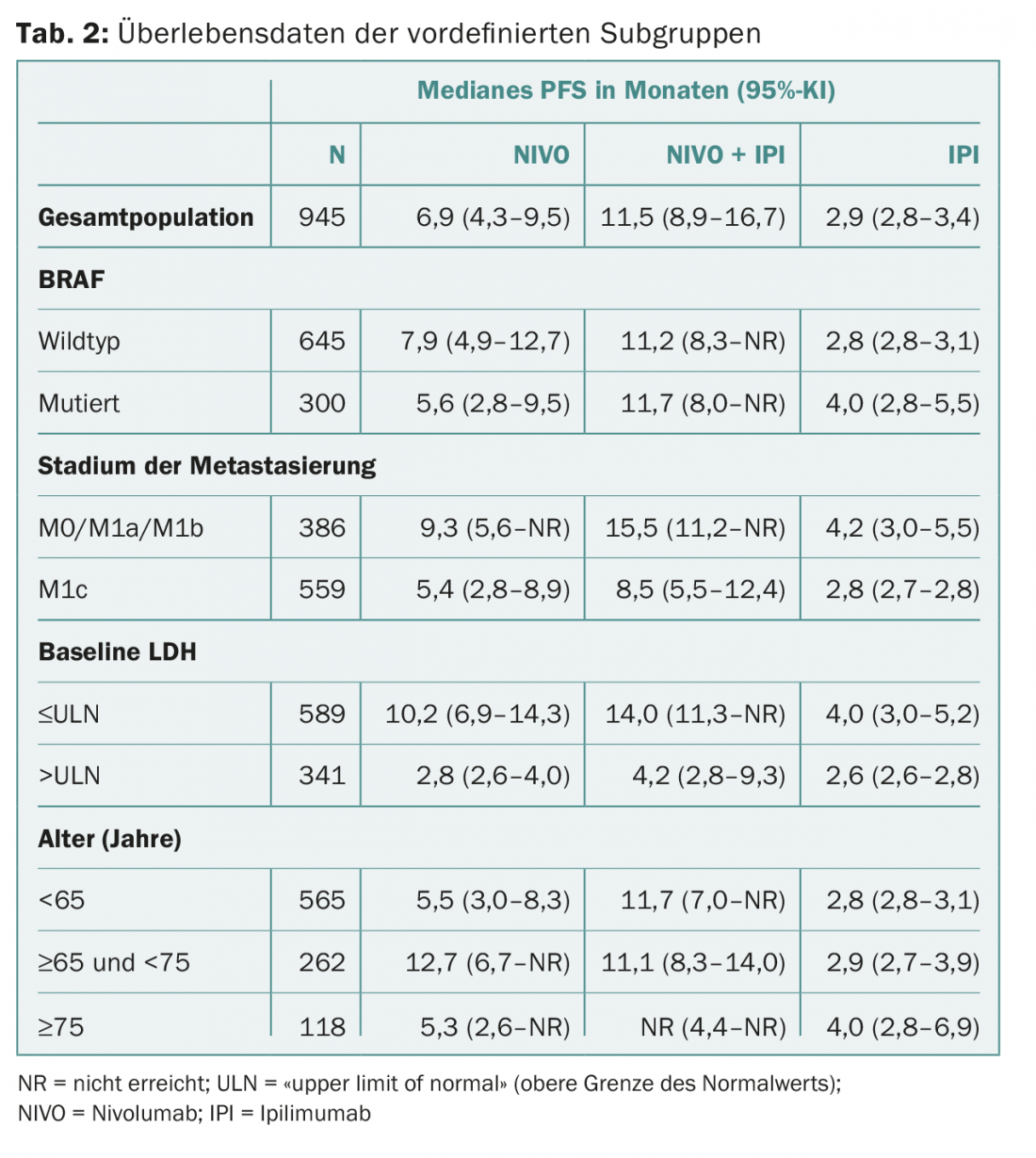
The authors conclude that the combination of nivolumab and ipilimumab is significantly superior to monotherapies even in patients with poor prognostic factors and is controllable in terms of safety profile. In practice, this could lead to faster and easier decision making regarding the use of combination therapy in the future. Especially since the researchers deliberately studied the subgroups most relevant to clinicians. Knowing whether certain patients do not benefit from the combination is important because, despite all the euphoria, it must not be forgotten that the therapies can be associated with a relatively large number of side effects.
COMBI-v: In this phase III trial, the combination of the BRAF kinase inhibitor dabrafenib and the MEK inhibitor trametinib (arm 1) with the BRAF inhibitor vemurafenib (arm 2) compared. The study population consisted of 704 previously untreated patients with metastatic, unresectable advanced stage IIIC/IV melanoma with BRAF V600E/K mutation. According to results previously published in the New England Journal of Medicine in January 2015 [1], the rate in overall survival, the primary endpoint, was 72% at 12 months in Arm 1 and 65% in Arm 2 (HR 0.69; 95% CI 0.53-0.89; p=0.005). Adverse event rates were comparable in both arms. Due to the convincing results, the study was stopped in July 2014. However, because patients had the option to remain on their respective therapies, the researchers had the opportunity for extended follow-up. An update was presented at Congress that included data through March 13, 2015:
- Median overall survival was 25.6 vs. 18 months, representing a significant mortality risk reduction of 34%.
- Median PFS was 12.6 vs. 7.3 months, representing a significant risk reduction for death or progression of 39%.
- After two years, 51 vs. 38% of patients were alive.
- There were no new surprising adverse events in the extended follow-up.
- Another sub-analysis presented at the congress also showed that the combination significantly improved quality of life.
The update thus thoroughly confirmed the convincing results of the analysis published a good eleven months earlier. The EU therefore approved the combination of dabrafenib and trametinib in this indication at the beginning of September 2015.
Source: European Cancer Congress (18th ECCO, 40th ESMO), September 25-29, 2015, Vienna.
Literature:
- Robert C, et al: Improved overall survival in melanoma with combined dabrafenib and trametinib. N Engl J Med 2015 Jan 1; 372(1): 30-39.
InFo ONCOLOGY & HEMATOLOGY 2015; 3(11-12): 32-34.











