If developmental retardation with failure to thrive cannot be explained in any other way, a urinalysis with determination of the organic acids in the urine (methylmalonic acid) and a cobalamin level in mother and child should be performed at an early stage to exclude a vitamin B12 deficiency. If there is evidence of a strict vegetarian or vegan lifestyle, nutritive vitamin B12 deficiency must be considered. In cases of confirmed malnutrition, dietary changes or supplementation can reduce the risk of long-term cognitive damage.
The first internationally published papers on neurological effects in vitamin B12(cobalamin) deficiency appeared a good fifty years ago. Jadhav described in Indian children under one year of age a syndrome of developmental regression, apathy, involuntary movement patterns, and skin changes that was associated with vitamin B12 malnutrition [1]. In the meantime, a large number of papers with a comparable symptomatology have also been published by children with a European or North American background. Reports on the long-term effects of vitamin B12 deficiency, on the other hand, are few. In 1999, 73 Dutch adolescents between the ages of nine and 15 were reported to have followed an exclusively macrobiotic diet until the age of six [2]: Such a diet, similar to a vegan diet, consists mainly of grains, rice, vegetables, legumes, nuts, seeds, and fruits, but unlike a vegan diet, still contains small amounts of fish. 48 of these adolescents underwent neuropsychological follow-up and showed deficits in reasoning, spatial awareness, and short-term memory compared with an age- and socioeconomically comparable group that ate a diet without restrictions on their meat consumption. The deficits were associated with continued decreased vitamin B12 levels [3]. Such studies are consistent with clinical experience showing that cognitive impairment resulting from early vitamin B12 deficiency may not be fully reversible.
In this publication, relevant information on the metabolism and physiological requirement of vitamin B12 is first given, before the specific problem of malnutrition in childhood is pointed out.
Causes of vitamin B12 deficiency
The child’s vitamin B
12
-deficiency usually results from a maternal undersupply of vitamin B12. Newborns are not yet symptomatic because until birth an active transport system ensures adequate vitamin levels in the child at the mother’s expense. Since the maternal symptoms of B12 deficiency are usually nonspecific and the symptom picture is little known, the underlying disorder in the mother is often only recognized by the symptomatology of her abnormal child.
Recently, there has been an increase in cases of infantile vitamin B12 deficiency due to maternal malnutrition, for example, in the context of a vegan diet, without concomitant vitamin B12 substitution.
In addition to this nutritional deficiency, extracellular and, in rare cases, intracellular causes of vitamin B12 deficiency may be present. Complex vitamin B12 metabolism is described in detail in the literature cited and is tabulated in Table 1 [4].
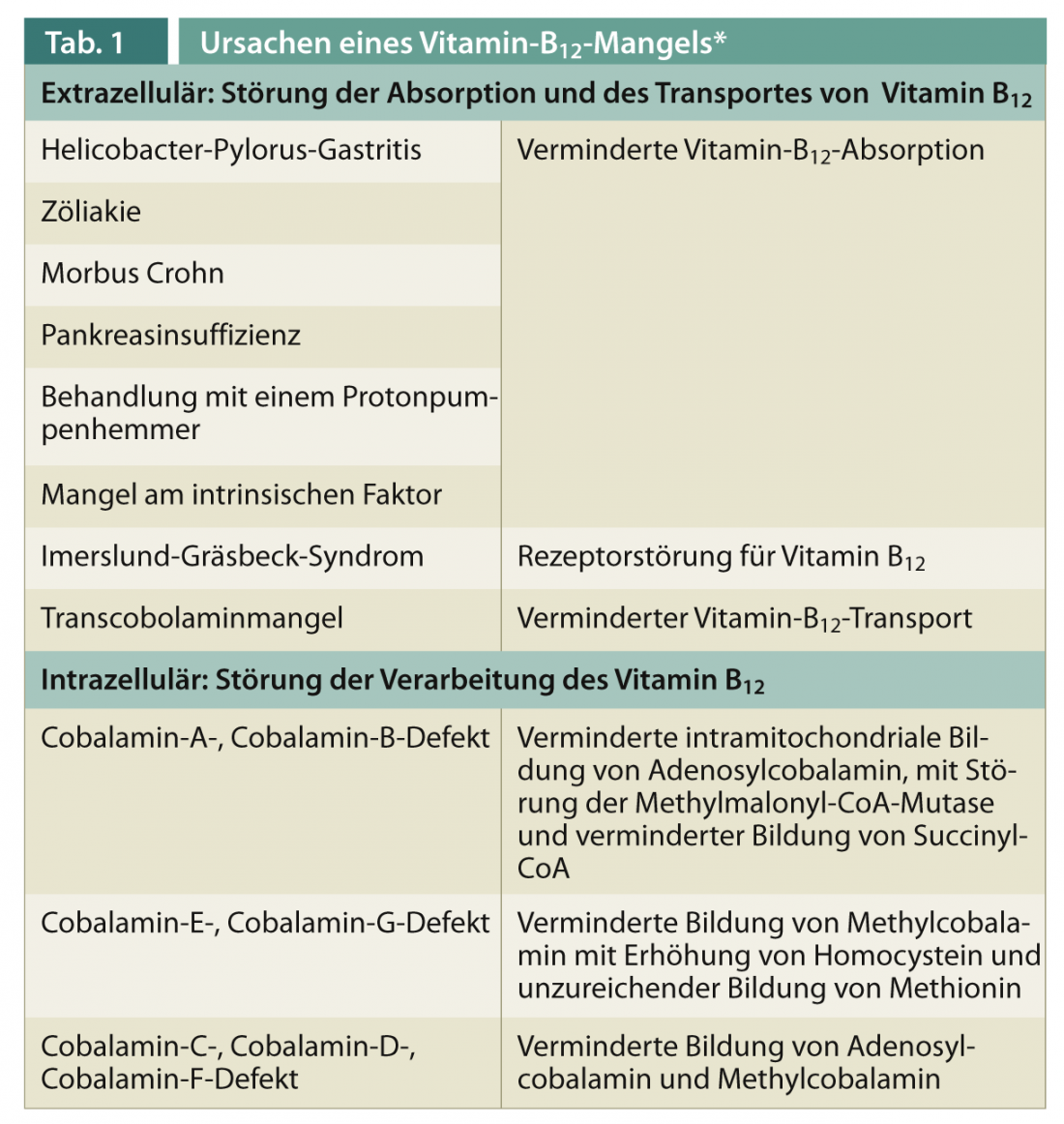
All intracellular defects require care in a metabolic center and extended and closely monitored substitution therapy of vitamin B12 and additional cofactors.
Sources and need of vitamin B12
Vitamin B12 can only be obtained from food of animal origin, the content of vitamin B12 in plant products such as algae is negligible. The following is a list of the vitamin B12 content in common foods:
- 1 dl milk = 0.2 μg
- 100 g yogurt = 0.6 μg
- 100 g cheese = 1-2 μg
- 100 g Cervelat = 0.6 μg
- 100 g Wienerli = 1.2 μg
- 100 g fish/meat = 1-5 μg
- 100 g egg (2 pieces) = 1.6 μg
Vitamin B12 requirement
The minimum requirement for vitamin B12 depends on age and increases in adolescents and pregnant women. Table 2 shows the average requirement for vitamin B12 as a function of age [5].
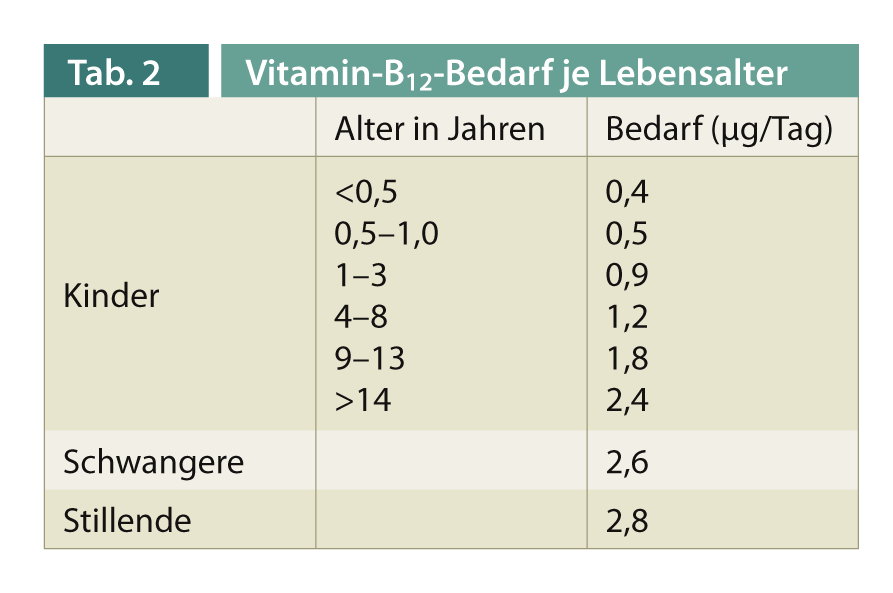
The measurable vitamin B12 concentration in the blood depends on dietary habits. With a high proportion of animal food consumed, vitamin B12 intake is 3-22 μg/day. Strict vegetarians consume only 0-0.25 μg/day. Unused vitamin B12 is excreted through the intestines; symptoms of vitamin B12 overdose are not known.
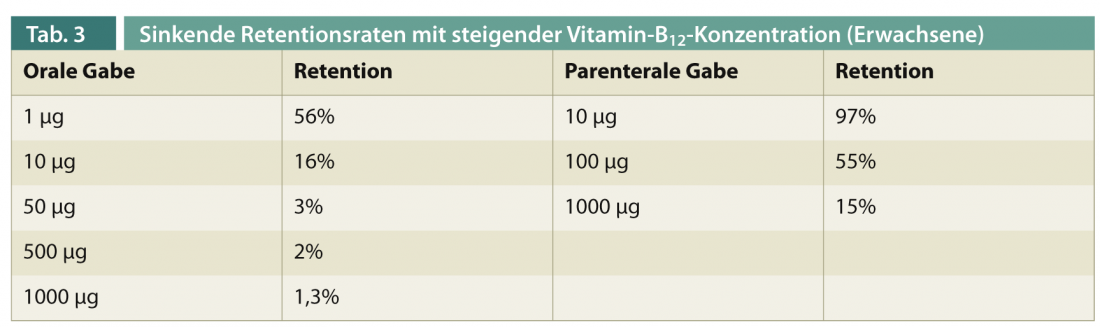
Retention rates and storage of orally or parenterally administered vitamin B12.
Since the retention rates of substituted vitamin B12 decrease with increasing concentration of substitution due to the limited capacities of the intrinsic factor, repeated replenishment of hepatic stores is required in vitamin B12 deficiency. The percentage retention rates are shown in Table 3 [6].
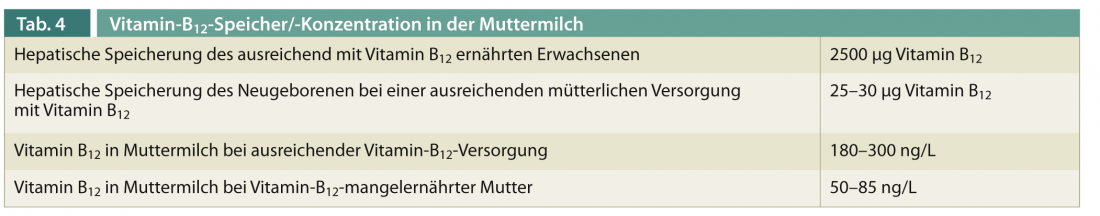
The hepatic vitamin B12 storage capacity of the newborn is only 1⁄100 of that of an adult. Provided that the mother is sufficiently supplied with vitamin B12, she can adequately ensure the infant’s daily requirement via her breast milk (0.45 µg vitamin B12/day, of which approx. 85% is utilized). In breast milk, vitamin B12 is bound to transcobalamin-1 (haptocorrin) and thus protected from the proteolytic enzymes of the stomach. The vitamin B12 concentration in the breast milk of a malnourished mother is only one third of the concentration of a mother who is adequately nourished with vitamin B12 (Tab. 4). In commercially produced powdered milk, the vitamin B12 content is generally higher than in breast milk.
Vitamin B12 deficiency
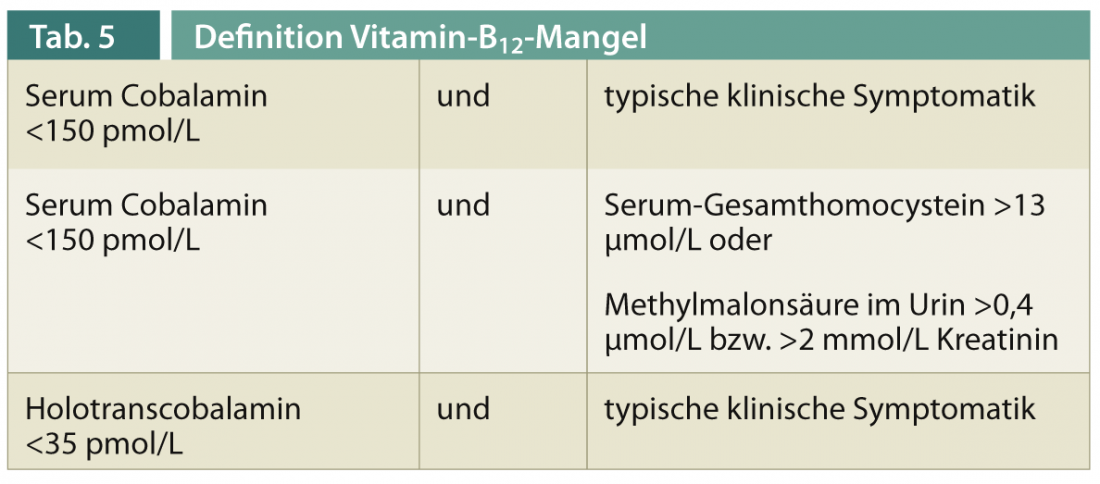
We speak of a vitamin B12 deficiency in the case of a specific constellation of laboratory values (especially cobalamin, total homocysteine [Serum] and methylmalonic acid [Urin]) as well as a typical clinical symptomatology (Tab. 5).
Macrocytic anemia is observed in only 80% of vitamin B12 deficient patients because the anemia may be masked by high folic acid levels and the macrocytosis may be masked by iron deficiency or thalassemia. Both parameters are not reliable as screening parameters.
Pathophysiological symptoms
As a result of vitamin B12 deficiency, atypically shaped fatty acids are deposited in the myelin of the nerve sheaths. These lead to impaired neuronal transmission. Furthermore, physiologically necessary methylation reactions cannot take place due to a reduced formation of S-adenosylmethionine. The increased systemic homocysteine levels additionally lead to cell-toxic degradation products. In adult patients with vitamin B12 deficiency, an increased concentration of tumor necrosis factor-α, reversible by vitamin B12 substitution, and a decreased concentration of epidermal growth factor were additionally detected. Other secondary disturbances in cytokine metabolism are conceivable. Combined, the aforementioned effects lead to impaired myelination and decreased oligodendrocyte differentiation.
Clinical symptoms of the child
Infants with vitamin B12 deficiency usually become conspicuous between the eighth and tenth months of life by otherwise unexplained irritability, lack of growth and weight gain, apathy, and anorexia. Long-term vitamin B12 deficiency can lead to regression in psychomotor development, epilepsy, and severe spinal cord damage (in the sense of funicular myelosis). Electrophysiologically, pathologically delayed evoked potentials are found as evidence of posterior cord dysfunction. In central imaging, secondary brain atrophy may occur if deficiency begins early and persists for months.
Case reports of neurologically disturbed children due to nutritive vitamin-B12 deficiency.
At the St. Gallen Children’s Hospital, we have cared for eight children with primary nutritive vitamin B12 deficiency due to maternal malnutrition over the past three years [7]. We assume that a similar prevalence can be demonstrated in other locations, provided that children are specifically screened for this purpose. The following are the symptoms of the children in our care:
- Refusal of age-appropriate food
- Frequent vomiting
- Failure to thrive with body masses below the 3rd percentile
- Regressive behavior pattern
- Developmental retardation that cannot be explained.
The diagnosis of vitamin B12 deficiency was confirmed by laboratory chemistry by an elevated urinary methylmalonic acid level and a decreased serum cobalamin level. Macrocytic anemia was detected in six of eight children. Associated with the decreased supply of vitamin B12, we saw decreased vitamin D levels, hypocalcemia, and significantly decreased serum zinc levels in all children. Further examination procedures revealed generalized EEG slowing, compaction of liver structure on sonography, ventricular dilation, and delayed evoked potentials. After substitution with vitamin B12, first parenterally and later per os and by a change of diet including meat-containing food and dairy products, all children showed a significant improvement of the core symptoms and a recovery of their weight.
Therapy of vitamin B12 deficiency
After confirming the diagnosis, hydroxycobalamin is given intramuscularly as a depot at a dose of 1 ml = 1000 µg for three consecutive days for primary replenishment of hepatic stores. Further substitution therapy depends on the underlying defect. With a reliable dietary change, if a nutritive deficiency is present, it is possible to quickly switch to per-os administration or to supplement the diet with a vitamin B12-enriched diet. In the case of intracellular dysfunction, vitamin B12 must be given in high doses as an i.m. injection for the rest of the patient’s life. Injection for the rest of life. Therapy can be guided by the clinical course as well as measurement of urinary methylmalonic acid. Administration of cyanocobalamin, the precursor of hydroxycobalamin, is less suitable because the valley levels achieved are lower than after administration of hydroxycobalamin and a cytotoxic effect cannot be excluded in the presence of concomitant methionine deficiency.
Conclusion
In cases of confirmed vitamin B12 malnutrition, dietary changes or supplementation can reduce the risk of long-term cognitive damage. Because other essential micronutrients such as zinc, vitamin D, and calcium are often decreased, extensive dietary counseling must be provided. For families who have made a conscious decision to follow a vegan or macrobiotic diet, it is important to ensure close and repeated supervision of the child to ensure a sustainable change or supplementation of food intake. If necessary, family therapeutic support is required.
Oswald Hasselmann, M.D.
Literature:
- Jadhav M, et al: Vitamin B12 deficiency in Indian infants. A clinical syndrome. Lancet 1962; 2: 903-907.
- Dusseldorp M, et al: Risk of persistent cobalamin deficiency in adolescents fed a macrobiotic diet in early life. Am J Clin Nutr 1999; 4: 664-671.
- Louwman MW, et al: Signs of impaired cognitive function in adolescents with marginal cobalamin status. Am J Clin Nutr 2000; 3: 762-769.
- Whitehead VM: Acquired and inherited disorders of cobalamin and folate in children. British Journal of Haematology 2006; 134: 125-136.
- Institute of Medicine: Dietary reference intakes: thiamin, riboflavin, niacin, vitamin B6, folate, vitamin B12, pantothenic acid, biotin, and choline. National Academy Press, Washington 1998.
- Carmel R: How I treat cobalamin (vitamin B12) deficiency. Blood 2008; 112: 2214-2221.
- Hasselmann O, Mathis A: A preventable disease – cobalamin-deficient encephalopathy in childhood. Swiss Archives of Neurology and Psychiatry 2012; 163(4): 152-154.
InFo Neurology & Psychiatry 2013; 11(1): 36-39.











