Intracranial hemorrhage is one of the most feared complications of oral anticoagulant therapy. At the annual meeting of the Swiss Cerebrovascular Society in Geneva, a lecture was dedicated to this topic. How should we proceed with NOAKs until specific antidotes are available? In addition, an interesting study on risk markers in ischemic stroke was presented.
Maurizio Paciaroni, MD, Perugia, provided an overview of the management of cerebral hemorrhagic complications during anticoagulation therapy. First, he presented data from the Perugia Stroke Registry: between 2006 and 2014, 2218 strokes and transient ischemic attacks (TIAs) and 317 intracranial hemorrhages (14.3%) occurred-37 of them, or 11.7%, occurred with warfarin, and two occurred with therapy with the new direct oral anticoagulants (NOAKs). Almost half of those with intracranial hemorrhage on warfarin or NOAK died while still in hospital, highlighting the relevance of the issue. This showed that 14 of the 37 warfarin patients, but both NOAK patients, died.
The volume of intracranial hemorrhage that occurs with vitamin K antagonists may increase within the first few hours, generally resulting in a mortality rate of nearly 70%.
What are the antidotes?
To normalize clotting as quickly as possible, fresh frozen plasma (FFP), intravenous vitamin K, and prothrombin complex concentrate work against warfarin. The latter acts faster than plasma (faster correction of INR without greater volume loading), but carries the risk of disseminated intravascular coagulation. Vitamin K takes up to 24 hours to normalize the INR.
A slightly older retrospective study [1] comparing the three antidotes concluded that volume expansion of intracranial hemorrhage occurred significantly less frequently (19%) with concentrate than with plasma (33) or vitamin K (50%). However, the difference was no longer significant provided the INR could be normalized within two hours, suggesting that normalizing the INR as soon as possible prevents hematoma growth.
There is a slightly increased risk of thrombosis after administration of a prothrombin complex concentrate (this in contrast to the other two options). Thromboembolic events occur more frequently under 4-factor prothrombin complex concentrates (1.8%) than under 3-factor concentrates (0.7%), according to a meta-analysis [2]. The overall rate was 1.4%.
“The management of cerebral hemorrhagic complications with warfarin can be summarized as follows: Prothrombin complex concentrates are preferable to FFP for immediate normalization of INR. Vitamin K is needed to maintain normalization (for both FFP and concentrates). Data from randomized trials are unfortunately not available,” Paciaroni said.
New oral anticoagulants
First, there is the question of how to measure the anticoagulant effect of NOAKs. According to the speaker, in case of major acute bleeding under thrombin inhibitors, the activated partial prothrombin time (aPTT) and the thrombin time (TT) should be collected. For factor Xa inhibitors, measurement of anti-Xa activity and prothrombin time (PT) is indicated in such a case.
Overall, fewer patients experience intracranial hemorrhage with NOAKs than with warfarin. However, a post-hoc analysis of the RELY trial [3] showed that intracerebral hemorrhage has a high mortality (more than 60%) not only with warfarin but also with dabigatran. The problem with treating cerebral hemorrhagic complications with apixaban, dabigatran, rivaroxaban, and edoxaban is that no specific antidote is available. In April 2014, the so-called RE-VERSE AD study started, which is currently recruiting patients in more than 35 countries worldwide. This study investigates idarucizumab, which is designed to reverse the anticoagulant effect of dabigatran. Previously, a study presented at the 2013 AHA Congress demonstrated that idarucizumab injection had a rapid, complete, and sustained effect against dabigatran anticoagulation in healthy volunteer participants (visible in dTT measurement).
A molecule called PRT4445, which targets rivaroxaban and apixaban, is in clinical development. In a preclinical in vivo study presented at the International Congress of Thrombosis in 2008, the activated prothrombin complex concentrate FEIBA® was shown to be effective against rivaroxaban. With the same NOAK, a 2011 randomized controlled trial [4] showed immediate and complete reversal of the anticoagulant effect by administration of 4-factor prothrombin complex concentrate (as measured by normalization of prothrombin time and endogenous thrombin potential) in healthy study participants.
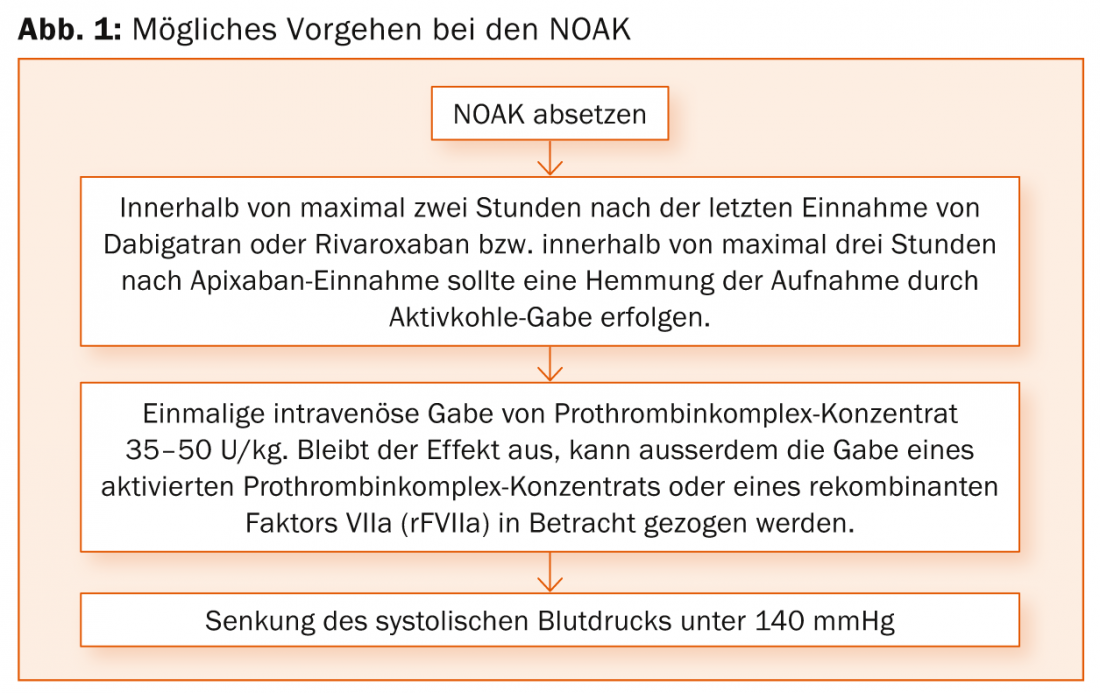
The procedure for intracranial hemorrhage under NOAK is summarized in Figure 1 .
Risk markers for ischemic strokes.
The Northern Manhattan Stroke Study (NOMAS) is one of the largest stroke cohort studies in the world. Among other things, the goal is to study stroke risk factors in a multiethnic urban population. The sub-study presented at the SHG congress [5] is a nested case cohort study within NOMAS. In it, they tested the two biomarker candidates procalcitonin (PCT) and MRproANP. A total of 172 first-time ischemic strokes, including fatal ones, and twice as many controls (stroke-free participants) with available baseline blood were studied. The hypothesis was that known stroke risk factors such as acute or chronic infections with inflammation, endothelial damage, and atherosclerosis could be read off the PCT – potentially making procalcitonin a marker for stroke likelihood. In addition to PCT, MRproANP might also indicate an increased risk of strokes, but this time as an expression of hemodynamic dysfunction, e.g., in underlying chronic heart failure, St.n. Myocardial infarction or atrial fibrillation.
The case and control cohorts consisted of 59 and 65% from women, the mean age was 72 resp. 68 years. With respect to all ischemic strokes, the hazard ratio in the highest quartile was 3.45 for MRproANP (95% CI 1.58-7.53) and 1.98 for PCT (95% CI 1.02-3.83)-this after adjusting for important demographic and medical risk factors. In other words, the risk of stroke was significantly greater with elevated marker levels. Cardioembolic stroke even showed a 15-fold increase in risk in the highest MRpro ANP quartile (HR 15.34; 95% CI 3.64-64.64). Of course, according to the authors, further studies are now needed to confirm the results.
Source: 18th Annual Meeting of the Swiss Brain Stroke Society (SHG), January 29-30, 2015, Geneva.
Literature:
- Huttner HB, et al: Hematoma growth and outcome in treated neurocritical care patients with intracerebral hemorrhage related to oral anticoagulant therapy: comparison of acute treatment strategies using vitamin K, fresh frozen plasma, and prothrombin complex concentrates. Stroke 2006 Jun; 37(6): 1465-1470.
- Dentali F, et al: Safety of prothrombin complex concentrates for rapid anticoagulation reversal of vitamin K antagonists. A meta-analysis. Thromb Haemost 2011 Sep; 106(3): 429-438.
- Hart RG, et al: Intracranial hemorrhage in atrial fibrillation patients during anticoagulation with warfarin or dabigatran: the RE-LY trial. Stroke 2012 Jun; 43(6): 1511-1517.
- Eerenberg ES, et al: Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation 2011 Oct 4; 124(14): 1573-1579.
- Katan M, et al: Procalcitonin, Copeptin and Midregional Pro-atrial Natriuretic Peptide as Markers of Ischemic Stroke Risk: The Northern Manhattan Study. Stroke 2014; 45: A54.
InFo NEUROLOGY & PSYCHIATRY 2015; 13(2): 32-34.











