Should an asymptomatic colorectal primary tumor with nonresectable synchronous liver metastases be resected initially or only if there is a good response after chemotherapy? This question was discussed again at the 23rd United European Gastroenterology Week. A retrospective study suggests equivalence between the two approaches. Another study focused on follow-up after curative surgery for AJCC stage II-III tumors. There was exciting news about locally advanced rectal cancer at the 2016 Gastrointestinal Cancers Symposium in San Francisco.
Colorectal cancer is the third most common cancer worldwide and ranks fourth in causes of death [1]. The primary metastatic site is the liver, with liver metastasis detected synchronously with the diagnosis of the primary tumor in approximately 20% of patients. In another 25%, liver metastases develop after an interval for treatment of colorectal cancer (metachronous metastases).
The vast majority of patients with stage IV colorectal cancer have non-resectable liver metastases at the time of diagnosis. Resectability is now primarily defined by the possibility of R0 resection of metastases and by the volume of healthy liver tissue remaining postoperatively (at least 30% of liver volume) [2]. In patients with metastatic colorectal cancer and nonresectable liver metastases, the value of initial palliative resection of the primary tumor followed by first-line chemotherapy versus immediate chemotherapy followed by resection for good response is unclear [3–6]. This question is then also the subject of clinical studies.
New data from UEGW
A retrospective analysis on the topic was presented at the United European Gastroenterology Week (UEGW) in Barcelona [7]. Included were 148 patients with colorectal cancer and synchronous unresectable liver metastases. Patients were followed for a median of 45.5 months. Fifty-seven percent of patients were treated with initial chemotherapy, followed at most by primary tumor resection and further postoperative chemotherapy for downsizing of liver metastases (group 1). The other 43% underwent surgical excision of the primary tumor, followed at most by first-line chemotherapy for downsizing of liver metastases (group 2). Baseline characteristics of the two study groups were comparable. The primary endpoint was overall survival after a median of 48 months.
Group 1: 34 of the 85 patients in this group eventually underwent colorectal resection. Of these, 33 received second-line chemotherapy. Ten cases required emergency surgery during the first chemotherapy: two perforations and four obstructions required resection with stoma, two patients received a stoma without resection, and two received a self-expanding metal stent. Overall survival was 15.3%. Liver metastases were resected after a good response to conversion chemotherapy in 20% of patients and treated ablatively with percutaneous radiofrequency in 16%.
Group 2: 42 of the 63 patients in this group received chemotherapy after surgery (median after 1.43 months). Overall survival was 19%. Resection of liver metastases was possible in 30.2% of cases, and percutaneous radiofrequency ablation was performed in 19%.
Both treatments equally effective?
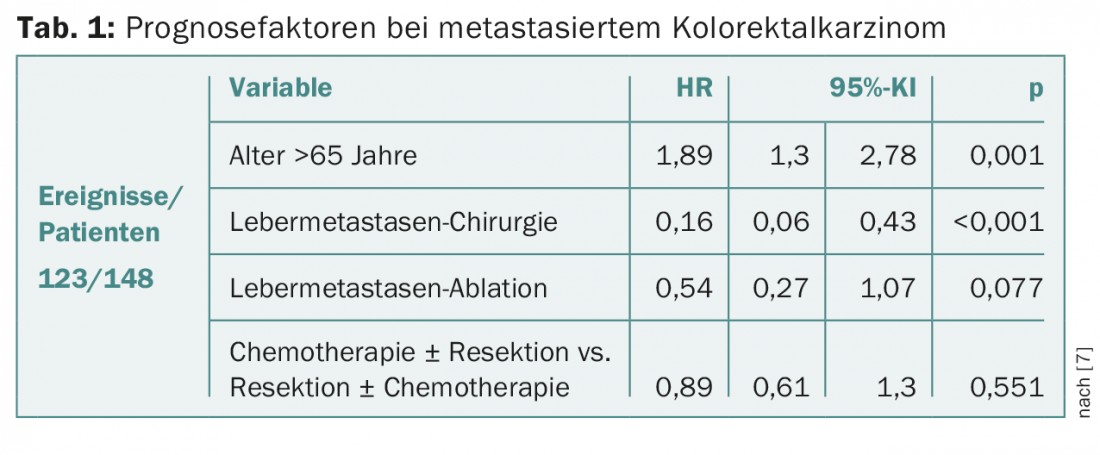
The two groups did not differ significantly in terms of survival rates (15.3% vs. 19%; p=0.633). However, when comparing individuals who received colorectal resection to those without surgery in the overall population, significant differences were found (p=0.025). In the second group, the rate of liver metastasis resection was higher, but just not significant (20% vs. 30.2%; p=0.056). Chemotherapy regimens were comparable, but in the first group anti-VEGF and -EGFR monoclonal antibodies were used more often overall (53.8% vs. 22.5%; p=0.014) and treatment was discontinued more often due to disease progression. In multivariate analysis, age (>65 years) and absence of liver metastasis surgery were relevant negative prognostic factors (Table 1) . Considering only the operated and chemotherapy-treated patients in both groups, better survival was seen with postoperative chemotherapy, deep lymph node involvement, and age less than 65.
The authors conclude that, taking into account the limitations of a retrospective analysis, both treatment pathways are equally effective. In fact, in synchronously metastatic colorectal cancer, it is usually the control of the metastases or the progression of the disease that determines the prognosis rather than the resection status of the primary tumor.
Follow-up after curative surgery
The goal of postoperative follow-up of colorectal carcinoma is the early diagnosis of (asymptomatic) recurrence in order to induce a new curative resection and, ergo, a prolongation of survival time. A Portuguese study, also presented at the congress [8], tested the effects of intensive structured follow-up over five years in 404 patients with AJCC stage II-III colorectal cancer after curative surgery (Table 2).
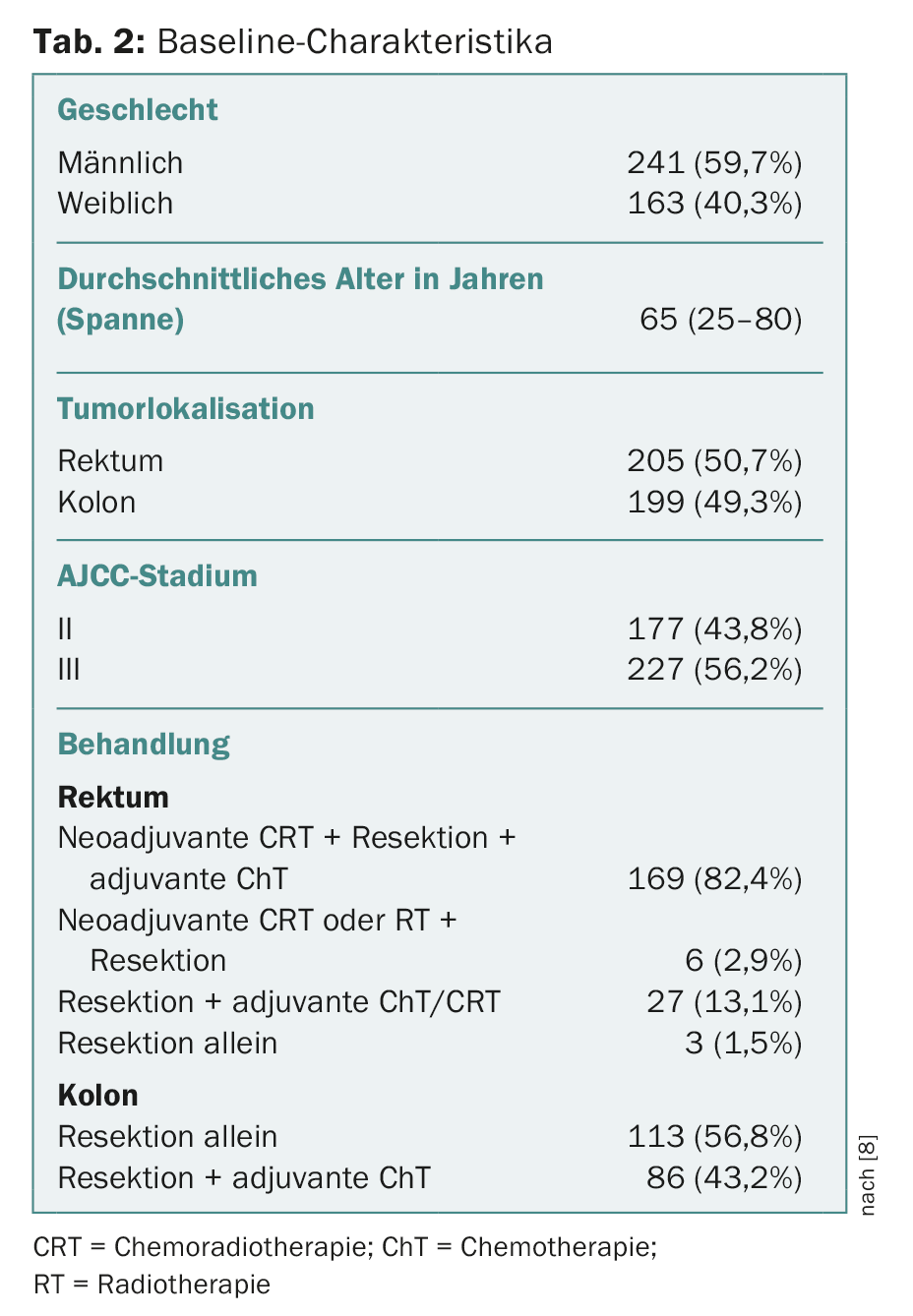
The Instituto Português de Oncologia de Lisboa Francisco Gentil (IPOLFG) program consisted of periodic history and physical examination, collection of tumor markers CEA and CA 19-9, CT thorax/abdomen/pelvis, and colonoscopy (Table 3) . The primary endpoint was the rate of recurrent resections with curative intent.

On average, follow-up lasted 37 months. The follow-up program showed good diagnostic accuracy for the detection of recurrence (AUC 0.885). The recurrence rate was 12.9%, with most cases detected in the first three years (88.4%). Metastases were significantly more common than locoregional recurrences (86.5% vs. 13.5%). Elevation of tumor markers was responsible for detection in 46% of cases, CT in 40%, colonoscopy in 8%, and symptoms in 6%. 21 patients underwent curative resection. Here, 2-year survival was 95.2%, compared with 59.9% for unresectable recurrences (p=0.016). Age over 70 years (RR 5.43; 95% CI 1.33-22.17; p=0.018) and tumor location in the colon (RR 0.237; 95% CI 0.064-0.873; p=0.030) were significantly associated with unresectability of recurrence.
According to the authors, this intensive postoperative follow-up program thus showed a clear benefit: Of the 52 patients (12.9%) with detected recurrence, almost half, or 21 patients (40.3%), were able to undergo curative resection again.
ASCO-GI: New regimen for locally advanced rectal cancer.
Compared with five weeks of chemotherapy/radiotherapy, which is the standard preoperative treatment for locally advanced rectal cancer in many countries, a shorter (five-day) course of radiotherapy followed by three two-day cycles of consolidation chemotherapy over a seven-week period produced equally good results with better tolerability (and lower costs). The corresponding phase III study was presented at the 2016 Gastrointestinal Cancers Symposium in San Francisco [9]. The study included 515 patients with locally advanced rectal cancer (stage cT3 or cT4 without distant metastases). One group received 5-FU, Leucovorin®, and oxaliplatin along with radiation (50.4 Gy), and the other received FOLFOX-4 one week after five days of radiotherapy (5× 5 Gy). It should be noted that the addition of oxaliplatin is not currently the current standard.
An equal number of patients from the two arms could undergo radical surgery. After three years, disease-free survival did not differ significantly. Overall survival showed a trend in favor of the shorter regimen (73% vs. 64.5%; p=0.055). In addition, significantly fewer acute adverse events occurred (74% vs. 83%; p=0.007).
The authors also see great potential of shorter radiation therapy especially for patients with metastases in the liver or lungs, as it allows chemotherapy to be started much earlier for metastasis control.
Source: 23rd United European Gastroenterology Week, October 24-28, 2015, Barcelona; Gastrointestinal Cancers Symposium, January 21-23, 2016, San Francisco.
Literature:
- Ferlay J, et al: Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015 Mar 1; 136(5): E359-386.
- Clavien PA, et al: Strategies for safer liver surgery and partial liver transplantation. N Engl J Med 2007 Apr 12; 356(15): 1545-1559.
- Venderbosch S, et al: Prognostic value of resection of primary tumor in patients with stage IV colorectal cancer: Retrospective analysis of two randomized studies and a review of the literature. Ann Surg Oncol 2011; 18(12): 3252-3260.
- Ferrand F, et al: Impact of primary tumor resection on survival of patients with colorectal cancer and synchronous metastases treated by chemotherapy: results from the multicenter, randomised trial Federation Francophone de Cancerologie Digestive 9601. Eur J Cancer 2013; 49: 90-97.
- Poultsides GA, et al: Outcome of primary tumor in patients with synchronous stage IV colorectal cancer receiving combination chemotherapy without surgery as initial treatment. J Clin Oncol 2009; 27: 3379-3384.
- McCahill LE, et al: Primary mFOLFOX6 Plus Bevacizumab Without Resection of the Primary Tumor for Patients Presenting With Surgically Unresectable Metastatic Colon Cancer and an Intact Asymptomatic Colon Cancer: Definitive Analysis of NSABP Trial C-10. J Clin Oncol 2012; 30(26): 3223-3228.
- Arolfo S, et al: Colorectal Cancer with Synchronous unresectable Liver metastases. Which is the best treatment? UEGW 2015; P1677.
- Rodrigues RV, et al: Intensive Follow-Up After Curative Surgery For Colorectal Cancer. UEGW 2015; P1671.
- Bujko K, et al: Neoadjuvant chemoradiation for fixed cT3 or cT4 rectal cancer: results of a Polish II multicentre phase III study. 2016 Gastrointestinal Cancers Symposium; Abstract 489.
InFo ONCOLOGY & HEMATOLOGY 2016; 4(1): 48-50.