Usually a simple explanation can be found for benign discoloration of finger and toe nails: subungual hemorrhage, onychomycosis, exogenous pigment, or the use of specific medications. On the other hand, a rare cause of nail changes that is feared because of its still poor prognosis is subungual melanoma. This must not be overlooked and must be excluded by a biopsy.
Subungual melanoma accounts for approximately 0.7-3.5% of all malignant melanomas (MM) in fair-skinned individuals. At diagnosis, the disease is often already in an advanced stage.
The preferred localizations are the thumb and the big toe. In dark-skinned individuals, subungual melanomas account for approximately 25% of malignant melanomas. One famous victim of the disease is Bob Marley, who died of metastatic subungual malignant melanoma at the age of only 36.
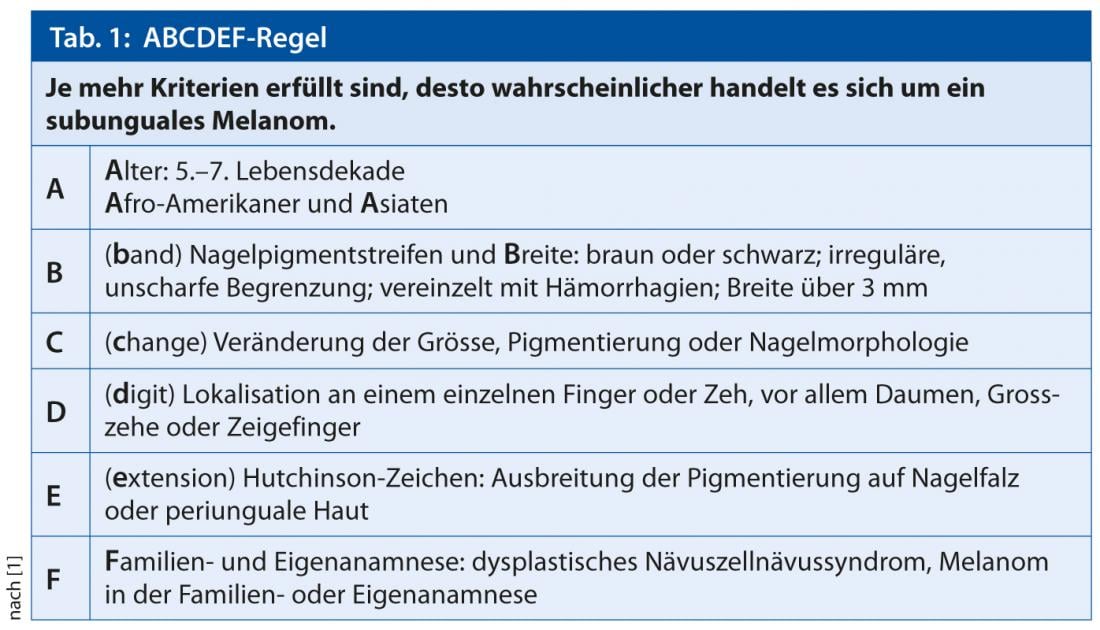
The median age of onset is now 66 years, and five-year survival rates are just over 50%. Prof. Dr. med. Carola Berking from Munich referred to these figures at the “3rd Munich International Summer Academy of Practical Dermatology” (ISA). “If there is a change in pigment, very wide stripes, or appearance of the Hutchinson sign, subungual melanoma and the ABCDEF rule should definitely also be considered,” she said (Table 1).
Indications from anamnesis and local findings
According to Prof. Berking, the following points provide initial anamnestic indications that a nail change is not harmless after all: lack of trauma, no relevant medication, already present for a long time but currently new changes, malignant melanoma in the patient’s own or family history. Ultraviolet (UV) radiation, on the other hand, does not appear to be significant in subungual melanoma.
Strip-shaped nail pigmentations are called Melanonychia striata or Melanonychia longitudinalis and can occur not only with the malignant melanoma, must nevertheless always urgently dermatoscopically and often also bioptically be clarified, demanded the expert. “Subungual melanoma should be considered for any new onset of longitudinal melanonychia in adulthood, as well as for a very wide (>3 mm), dark brown to black pigment streak and fuzzy or blurred margins,” Prof. Berking concluded. Fissuring, thinning, ulceration or destruction of the nail plate are suspect. Also a proximally wider pigment stripe than distally (triangle), caused by a fast growth of the tumor, an increase of pigment or an asymmetry are possible indications of a melanoma. Another clue, but not proving: the Hutchinson’s sign, a patchy pigmentation spreading to the proximal nail fold or periungual skin.
Subungual melanoma of the nail bed is much more difficult to diagnose. It is usually amelanotic, can displace or destroy the nail plate, and is often not noticed as malignant until it becomes an ulcerated nodule. In these amelanotic subungual melanomas, which occur in up to 25% of cases, differentiation from other conditions such as granuloma pyogenicum, warts, fibrokeratoma, glomus tumor, myxoid cyst, or unguis incarnatus can be very difficult. They are often confused. Dermoscopy and biopsies help further (see also interview). Differential diagnoses of pigmented subungual melanoma include benign changes such as lentigo simplex, melanocytic nevus, or benign melanocytic hyperplasia.
Therapy
Microscopically controlled surgery can often ensure complete excision with functionally and cosmetically acceptable results, so that amputation is now usually obsolete. 3-D histology allows precise analysis of the resection margins [3]. En bloc resection of the entire nail organ (plus nail fold) followed by full-thickness skin grafting, e.g. from the upper arm, is now the method of choice [4].
Source: “3rd Munich International Summer Academy of Practical Dermatology” (ISA), July 21-26, 2013, Munich.
Literature:
- Gauwerky KJ, Berking C: Malignant melanoma of the nail organ. Dtsch Med Wochenschr 2010; 135: 1431-1434.
- Pralong P, et al: Dermoscopy of lentigo maligna melanoma: report of 125 cases. Br J Dermatol 2012; 167(2): 280-287.
- Debarbieux S, et al: Perioperative confocal microscopy of the nail matrix in the management of in situ or minimally invasive subungual melanomas. Br J Dermatol 2012; 167(4): 828-836.
- Neczyporenko F, et al: Management of in situ melanoma of the nail apparatus with functional surgery: report of 11 cases and review of the literature. JEADV 2013; Epub 11.3.2013, DOI: 10.1111/jdv.12131.