Teamwork between primary care physician, nephrologist, transplant center and patient is essential. 50% of transplanted patients die with functioning kidney transplant. In the early phase after transplantation, the focus is on the adjustment of immunosuppression and the detection of rejection and infection in particular. Treatment of nonimmunologic complications, especially cardiovascular risk factors, is extremely important. Regular tumor controls should be performed, especially of the skin. Always watch for drug interactions, especially for immunosuppressants.
Kidney transplantation is the preferred renal replacement procedure for the majority of patients with chronic renal failure and is associated with the best quality of life and life expectancy for the patient. Currently, 5-year renal graft survival is over 70% for organs from deceased donors and over 80% for living donors [1].
Today, approximately 50% of transplant recipients with functioning grafts die due to cardiovascular complications followed by tumors and severe infections. Therefore, regular monitoring and treatment of comorbidities play a crucial role. The long-term outcome of transplantation depends largely on the quality and regularity of follow-up care. Here, good cooperation between the primary care physician and the transplant center is crucial.
Early phase after transplantation
The early phase of monitoring (first postoperative year) is predominantly performed directly at the transplant center, with temporal control intervals extended to up to three months after the initial phase. After the first year, the nephrologist close to the patient’s home, in cooperation with the family doctor, takes over the main part of the regular care, supplemented by annual check-ups at the transplant center.
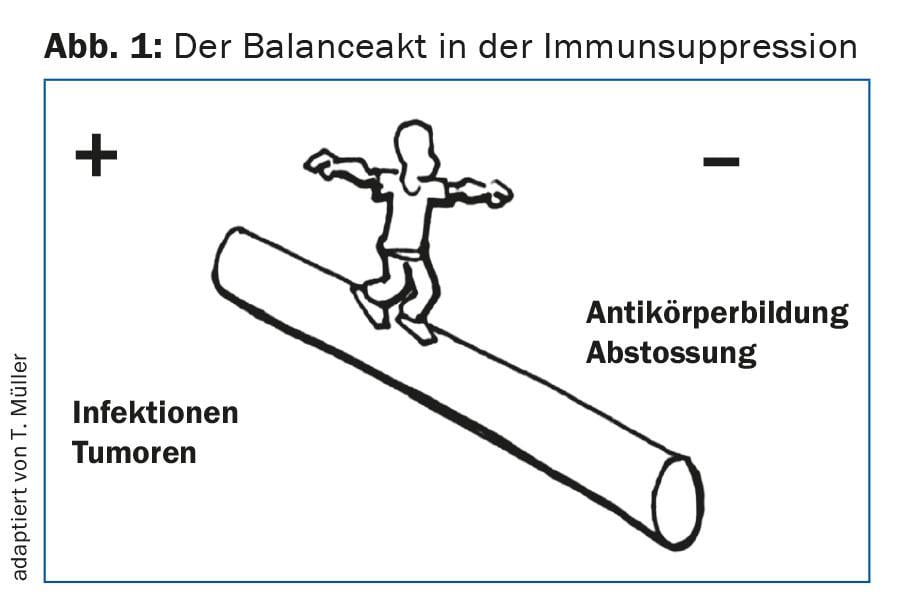
The initial close monitoring is necessary for early detection of acute immunological complications such as acute rejection reactions. To prevent this, i.e. to avoid under- or overimmunosuppression, a very individualized setting of immunosuppression is necessary (Fig. 1) . Furthermore, it is important to recognize infections, especially viral infections, in the early phase. In particular, these include CMV reactivation or CMV primo-infections, which can have severe consequences if left untreated [2]. In addition, close monitoring for possible BKV (polyomavirus) replication is necessary, as significant BKV viremia can lead to BK nephropathy and this, if untreated, can lead to rapid loss of graft function.
Controls in the long-term course
In the long-term course, greater importance is attached to the recording of non-immunological complications, including the control and adjustment of blood pressure as well as possible lipometabolic disorders and bone metabolism.
Because of the improved long-term survival of kidney transplant patients, we are now confronted with the consequences of long-term immunosuppressive therapy. Here, the increased risk of malignant skin tumors should be mentioned in particular. Non Melanoma Skin Cancer (NMSC) represents the highest proportion of all post-transplant malignancies at 40%. In NMSC, 90-95% are squamous and basal cell carcinomas. The risk of such carcinoma is significantly higher in immunosuppressed patients than in the general population [3], and the overall tumor risk is approx. increased two- to threefold [4]. For this reason, close monitoring of the skin is crucial and possibly a change in immunosuppressive therapy is necessary if NMSC occurs.
A major factor in the late phase of care is the problem of chronic changes in the graft, which almost always occur for reasons that are still unclear and shorten the functional life of the graft. The course of creatinine and proteinuria is crucial in functional diagnostics. A creatinine increase of more than 15% requires clarification. For protein excretion, determination of the protein-creatinine or albumin-creatinine quotient in spontaneous urine is usually sufficient. Here, too, the course over time and the increase in protein excretion are decisive. Significant changes should be discussed with the transplant center. It may then be necessary to decide on additional investigations such as screening for antibodies to the graft or even a kidney biopsy.
In the long-term phase, it is important that in case of illness, deterioration of kidney function, fever, pain or drug intolerance, contact is made with the transplant center again and again, even outside the agreed appointments, since in these situations a rapid clarification is often required, in the context of which inpatient treatment may also be necessary.
Patient self-measurements are also a very important part of standard monitoring. This includes measuring blood pressure, pulse, temperature and body weight, first daily and then intermittently. In particular, an elevated body temperature (usually an increase of more than 0.5°C above the individual normal range) and/or a significant weight gain from one day to the next of more than 1 kg are alarm signs that patients should report.
Immunosuppressive drugs
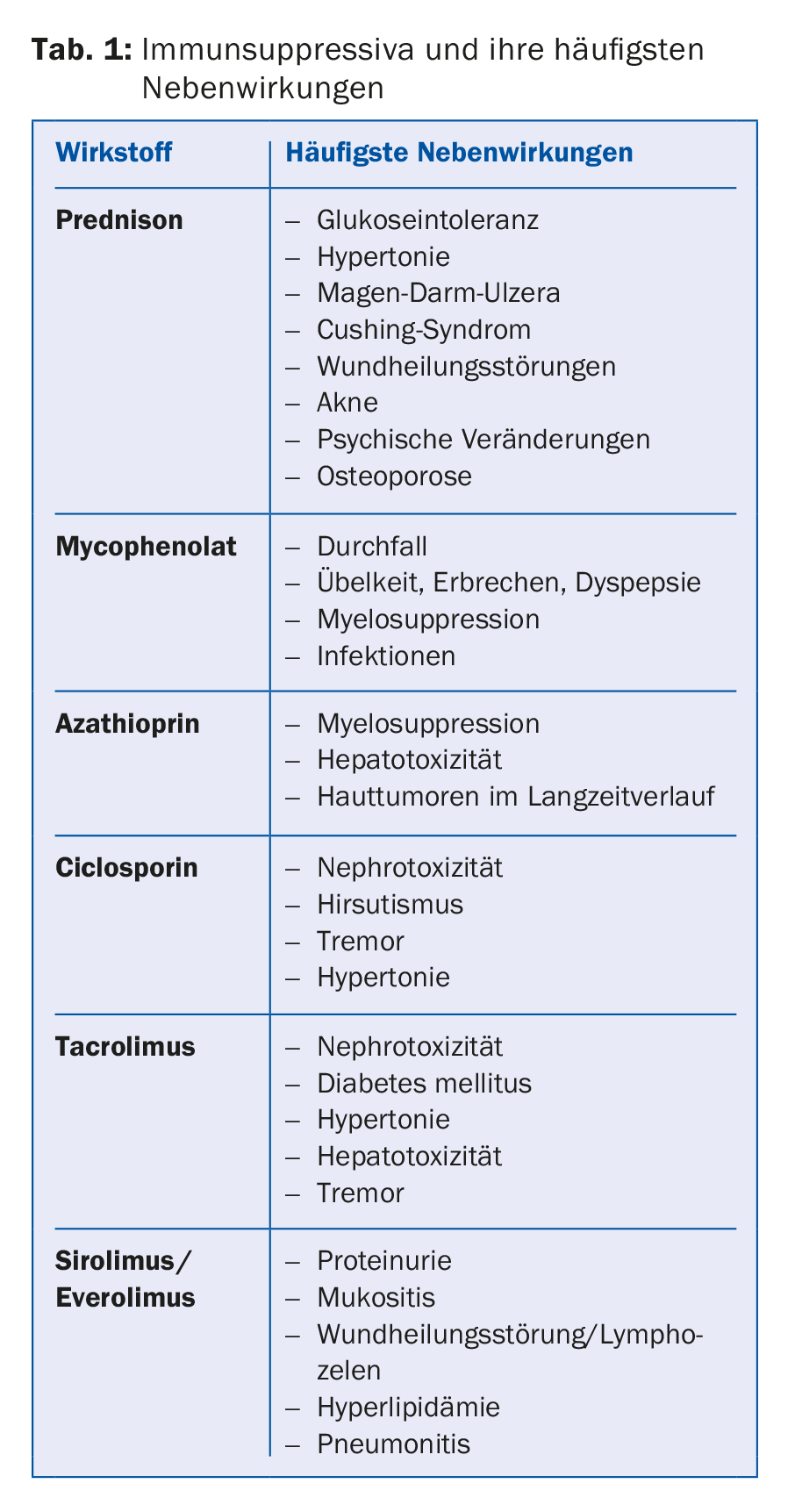
With a transplant, the patient is not cured, he must take regular medication for life. Therefore, the issues of side effects and interactions must always be discussed with the transplant center. Standard of care is double therapy in patients at low immunological risk or triple therapy in patients at higher risk. Immunosuppressive treatment usually consists of a calcineurin inhibitor, most commonly tacrolimus (Prograf® or Advagraf®, the latter being the sustained-release form of tacrolimus), and in some cases alternatively ciclosporin (Sandimmun Neoral®). In addition, an antiproliferative substance is used, in most cases mycophenolate (CellCept® or Myfortic®), more rarely azathioprine (Imurek®). In the early postoperative phase, a glucocorticoid is usually added as a third immunosuppressant, which is phased out after about six months depending on the immunological risk and the center guidelines (Table 1).
The adjustment of the dose, especially of the calcineurin inhibitors, is based on the so-called valley level, the determination of the drug concentration in the blood twelve hours after the intake of the last dose. Individual target levels are aimed at, adapted to the clinic (immunological situation, infectious or tumor complications).
For immunosuppressants, the preparations recommended by the transplant center should be used. Changes in therapy, dose, or switching to generic drugs should only be made in consultation.
Calcineurin inhibitors, like many other drugs, are metabolized via CYP3A, therefore great caution should be exercised when prescribing new drugs due to potential interactions. In particular, macrolide antibiotics (especially clarithro- and erythromycin) can lead to severe toxicity of calcineurin inhibitors by inhibiting CYP3A. However, herbal medicines also have a high potential for interaction. For example, a significant reduction in calcineurin inhibitor levels can occur with St. John’s wort, and a large increase with grapefruit juice, with the risk of consecutive rejection or overimmunosuppression.
Other drugs
In dental procedures and endoscopies with or without biopsies, antibiotic prophylaxis is not mandatory merely because the patient requires systemic immunosuppression. Antibiotic therapy according to the endocarditis prophylaxis regimen is usually indicated only in patients who would receive antibiotic prophylaxis even without immunosuppression and/or when procedures are planned in an infected area. In case of doubt, the individual situation of the patient should be assessed with the transplant center depending on the immune status.
In analgesic therapy, NSAIDs and COX II inhibitors should be avoided at all costs because of various possible renal side effects (vasomotor-induced acute renal failure, tubulointerstitial nephritis, salt retention, etc.), as is generally the case in all patients with impaired renal function.
Drug dosage must take into account renal function. In a very well functioning graft, the glomerular filtration rate (GFR) is usually above 60 ml/min and 1.73 m2 body surface area. According to the professional information, the dose must be adjusted for the different GFR ranges.
Urinary tract infections
The most common infections that occur after kidney transplantation are urinary tract infections. In principle, only symptomatic urinary tract infections should be treated in the long-term course. Prior to initiation of empirical therapy (usually with ciprofloxacin or amoxicillin/clavulanic acid), it is mandatory to take a urine culture for subsequent resistance-tailored treatment.
For recurrent urinary tract infections, first, empiric therapy is selected according to prior antibiotic resistance. On the other hand, contact should be made with the transplant center in order to clarify possible causes (e.g., reflux in the transplantation age, etc.). Furthermore, the consumption of cranberries resp. Cranberry juice recommended as a prophylactic measure, in some cases the use of L-methionine for urinary acidification can also be discussed.
Hyperuricemia and gout
Due to decreased renal uric acid clearance, hyperuricemia is a commonly observed complication of calcineurin inhibitor therapy. Especially with ciclosporin, gout attacks have been described in 5-10% of patients.
For the therapy of an acute gout attack, the short-term administration of steroids for three to five days (approx. 20-50 mg/d) recommended. NSAIDs should be strictly avoided. Prophylaxis with allopurinol should not be administered to patients on continuous therapy with azathioprine because this combination can lead to severe neutropenia/agranulocytosis.
Diarrhea and gastrointestinal complaints
Diarrhea and gastrointestinal discomfort are common problems in immunosuppressed patients. If a patient complains of diarrhea (>3 liquid-mushy defecations) lasting longer than two days, an infectious etiology should first be sought (general fecal bacteriology, norovirus). In case of persistence and/or concurrent fever, the patient should be sent to the transplant center (clarification of CMV infection/CMV colitis, etc.). If drug-induced diarrhea is suspected, which is frequently observed especially infection-triggered with mycophenolate, the dose of immunosuppressants can be adjusted. In cases of diarrhea, early tacrolimus level monitoring is also always indicated, as increased absorption of tacrolimus may occur, resulting in high levels.
Cardiovascular risk factors
Cardiovascular risk factors should be consistently treated. Arterial hypertension is present in 60-80% of renal transplant patients [6]. In principle, all substance classes of antihypertensives can be used; initially, a calcium antagonist is usually used primarily, and in the case of stable transplant kidney function, ACE inhibitors or ATII blockers (RAAS blockade) are also used. If proteinuria exceeds 1 g/24 h, a RAAS-blocking agent is the first choice. The target blood pressure for most transplant recipients is 130/80 mmHg (in home measurements); in some cases, target values must be set individually.
Dyslipidemia should also be treated intensively with lifestyle measures, especially weight control. However, drug therapy with a statin is often still required. The LDL target value is <2.6 mmol/l. Interactions with immunosuppressants must also be considered here.
Smokers should always be motivated to stop using nicotine and should be offered smoking cessation programs. Obese patients may benefit from nutrition counseling. Prophylaxis with acetylsalicylic acid is recommended for atherosclerotic cardiovascular disease.
Diabetes mellitus
Diabetes mellitus often recurs after transplantation. In particular, tacrolimus, sirolimus, steroid therapy, and older age are risk factors for the so-called “New Onset of Diabetes after Transplantation” (NODAT). For therapy of NODAT, in addition to the usual lifestyle measures and oral antidiabetic drugs such as DPP4 inhibitors (sitagliptin), insulin is often considered early. If immunosuppression can be reduced in the course of the disease, glucose metabolism returns to normal in some patients. Therapy goal according to KDIGO guidelines is an HbA1C <7-7.5%.
Desire to have children
If you wish to have children, it is essential to contact the transplant center to openly discuss the risks and dangers. Also, a change in medication is usually mandatory prior to any pregnancy. Pregnancy in a woman after kidney transplantation is basically a high-risk pregnancy and requires close interdisciplinary care at the transplant center.
Vaccinations and travel
As a rule, complete vaccinations – according to the Swiss Vaccination Recommendation for Persons Before and After Solid Organ Transplantation – should have been given prior to transplantation at the time of listing. After transplantation, live vaccines such as rubella or measles are contraindicated due to immunosuppression. All non-living vaccinations should be refreshed regularly according to vaccination recommendations. Annual influenza vaccination is also recommended. However, it should be remembered that the vaccine response is often somewhat attenuated under immunosuppressive therapy.
When traveling to countries with an increased risk of gastrointestinal infections, prior consultation is recommended, for example at a center for travel medicine. Information on the resistance situation there can be obtained here. Based on this, the recommended empirical therapy to be taken in case of emergency is determined.
Conclusion
In summary, the success of transplantation, especially with regard to graft survival and patient quality of life, depends critically on close collaboration between the primary care physician, nephrologist, transplant center, and patient.
Literature:
- Matas AJ, et al: OPTN/SRTR 2012 Annual Data Report: Kidney.
- Kumar D, et al: The AST Handbook of Transplant Infections, Wiley-Blackwell, 2011.
- Zwald FO, et al: Skin cancer in solid organ transplant recipients: advances in therapy and management part I: Epidemiology of skin cancer in solid organ transplant recipients. J Am Acad Dermatol 2011; 65(2): 253-261.
- Engels E, et al: Spectrum of Cancer Risk Among US Solid Organ Transplant Recipients. JAMA 2011; 306(17): 1891-1901.
- Kasiske B, et al: KDIGO clinical practice guideline for the care of kidney transplant recipients: a summary. Kidney Int 2010; 77: 299-311.
- Danovitch G: Handbook of Kidney Transplantation, Wolters Kluver, 2010.
HAUSARZT PRAXIS 2015; 10(12): 20-24