The 2020 annual congresses of the ATS and ERS were entirely under the influence of the SARS-CoV-2 virus: on-site events were greatly reduced, while online participation offerings increased and were well received, although not every single event could be transferred to the web. Of course, great emphasis was placed on the latest developments in asthma and COPD.
Professor Dr. Marek Lommatzsch from the Department of Pneumology at the University Medical Center Rostock (D) summarized the main points and findings concerning the two diseases. The main news were triple therapies in asthma and the use of ICS in COPD.
Prophylaxis of asthma and COPD
It is known that asthma is much less common when people live a traditional rural lifestyle. The common assumption is that the immune system needs to level off in the first few years of life: “It has type 1 and type 2 stimuli, and we believe that all microbiological stimuli are necessary for a rural child to level off from age 2 or 3. The patient’s immune system is normal at the age of 60 and is therefore not allergic,” explained Prof. Lommatzsch. “But if we take a big city child, which of course has less microbial stimuli and lacks balance, then that leads to children who later develop asthma to sort of take a wrong turn in that mis-stimulation.”
That the microbiome has a crucial role in the development of asthma is not news. However, one is learning more and more that COPD is probably not completely unaffected here either. The so-called “early origins of COPD” have been a topic at many symposia. It is currently assumed that patients do not suddenly develop their COPD at the age of 65, but that changes and remodeling processes, especially in the small airways, already begin in childhood and adolescence and in young adulthood. Cigarette smoking comes later, but then a prepared, pre-diseased airway is already there without the patient noticing. The expert referred to several studies [1] that suggest that COPD begins earlier than previously thought and that by then there is already a prepared airway that still gets the additional smoke damage. “And that, after all, is one of the possible explanations why only some smokers develop COPD and many don’t, even though they smoked just as much.”
Therapy of mild asthma
Prof. Lommatzsch described the GINA as an “international revolution”.
◊
-Guideline from last year, which carried out a radical swing: According to the international guideline, the preferred controller, i.e., the preferred option for mild asthma as an on-demand therapy, has since been ICS/formoterol instead of salbutamol. The bottom line of the underlying data is that the ICS/formoterol only as needed combo is primarily safer than the SABA as needed, fewer severe exacerbations occur. Since safety is an essential aspect, GINA is very consistent here. The problem on the other hand is that in various countries and areas – such as Europe – there is no approval at all for ICS/formoterol only when needed.
It is interesting in this context that in the new German NVL asthma ICS/formoterol is clearly mentioned as an option in stage 1 and 2 only if needed. However, not as a preferred option (because it is not allowed), but at least as a possible alternative. This is certainly important for German practice, as the majority of patients have been doing the as-needed use of ICS/formoterol instinctively for years anyway. Referring to ongoing studies, the pulmonologist said that the entry into a new era has taken place and it is quite expected that next year the first combi will come.
Triple therapy for asthma (ICS/LAMA/LABA).
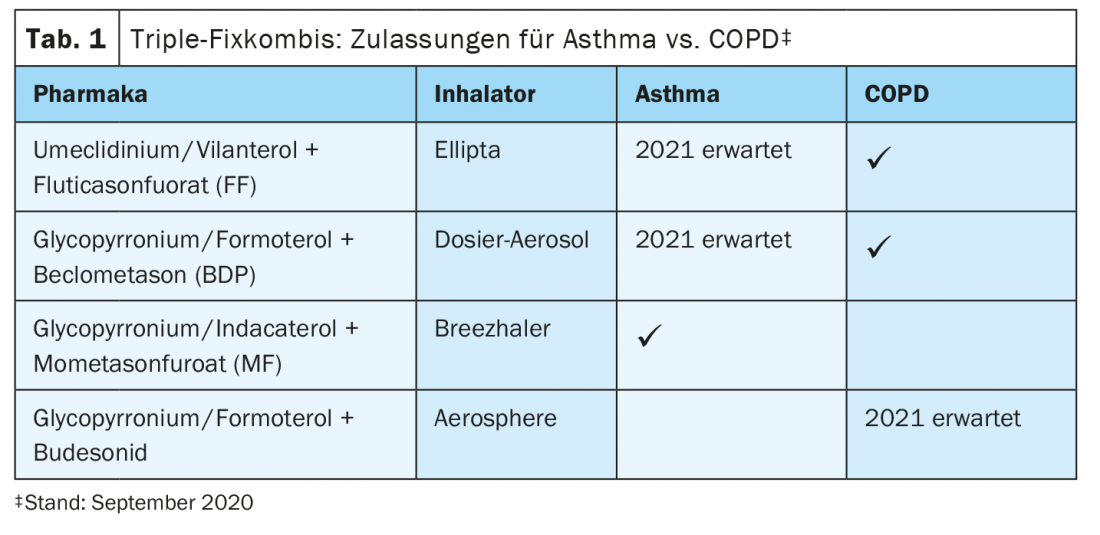
Triple therapy for COPD has been approved for some time. In asthma, this has now also happened: In the composition glycopyrronium/indacaterol + mometasone furoate, the triple combination has received EU approval, and two additional triple therapies are expected in the coming year (Table 1) . The TRIMARAN/TRIGGER trial, which investigated the glycopyrronium/formoterol + beclometasone combination, compared dual versus fixed triple therapy. The fact that the triple was superior to the dual therapy is not particularly surprising, but it was interesting to note that a free triple (BDP/FF plus tiotropium) is not inferior to the fixed triple and also remains an option.
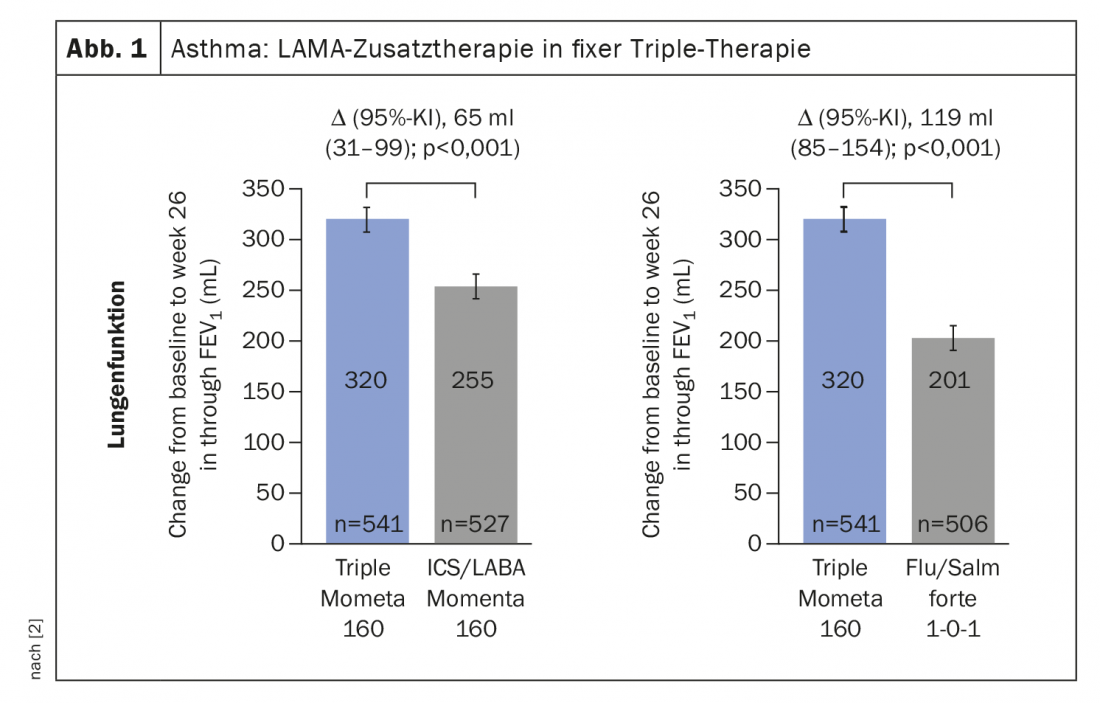
The IRIDIUM study on the now already approved triple preparation has highlighted another interesting aspect: Mometasone at a slightly lower dose had a stronger effect with the triple than ICS/LABA therapy at the highest dose. (Fig. 1). “I therefore believe that will be a big topic in the coming years: It may be possible to save steroid exposures with the triple-fix combinations,” Prof. Lommatzsch stated.
Therapy of severe asthma
The international guidelines recommend that in patients with severe asthma for whom inhaled therapy incl. of the triple combination is exhausted, biologics should be used as first-line agents. Oral steroids are second-line agents in such cases. There has been a paradigm shift here and as a physician nowadays you have to justify why you are treating a patient with prednisolone in long-term therapy instead of using a biologic.
There are currently 5 approved biologics; the anti-IgE-targeted omalizumab, the anti-IL-5-targeted reslizumab and mepolizumab, plus benralizumab (anti-IL-5(R)) and dupilumab (anti-IL-4/13). With the exception of reslizumab, all biologics are also approved for self-administration. With regard to the application criteria, it is not only the biomarker that determines which biologic is given, but very much also the medical history. Anamnestic measures and clues such as whether it is early-onset or late-onset asthma are at least as important as biomarkers or eosinophils. What is clear, however, is that all 5 biologics target the type 2 phenotype. “The question therefore always arises as to whether there is also type 1 or type-low asthma, and these discussions were again held intensively at the congresses,” Prof. Lommatzsch said. “In fact, we have more and more studies showing the same thing over and over again: Whether it’s with anti-TNF-alpha, anti-IL-17, anti-CXCR2, or, now currently presented at ERS, anti-IL-23 – the studies are all negative. Whenever it moves away from type-2- to type-2-low, it always fails.”
The expert therefore suspects “that so-called neutrophilic asthma probably exists only very, very rarely.” Patients who run as neutrophilic asthmatics may have another condition, such as a chronic infection, in his estimation. “We currently very much doubt – and all these studies also strongly underline this – that there really is a type 2 low asthma that could respond to certain biologics.
ICS in COPD therapy
In all patients with COPD, the first question a physician must ask is: Do they only have the problem of shortness of breath or do they also have exacerbations? For shortness of breath, bronchodilators are available therapeutically, and respiratory insufficiency therapy with oxygen or ventilation may also be considered. Some patients may also be helped palliatively by lung volume reduction. However, when exacerbations are added, inhaled steroids play a role. The decision to do so may be supported by blood eosinophils, as a count of >300 cells/μl makes an ICS benefit likely. In addition, however, there are other options for reducing exacerbations, ranging from rehabilitation measures to vaccinations and therapy of comorbidities to Roflumilast.
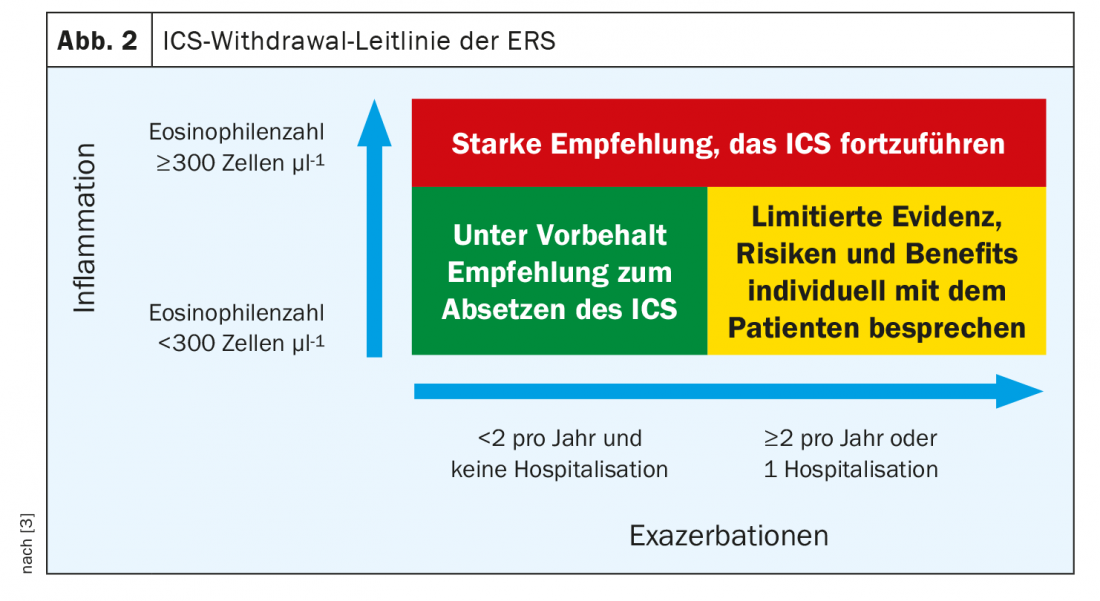
As shown in Table 1, two approved triple therapies already exist for COPD, and a third in the composition glycopyrronium/formoterol + budesonide is expected in 2021. The pivotal study for this (ETHOS), just like the studies of the other triples, shows that the higher the eosinophil counts, the more the patient benefits from adding the inhaled steroid. For this reason, the ERS has now issued an ICS widdrawal guideline that provides recommendations on when to safely discontinue an inhaled steroid. The bottom line reflects the study results: Patients who do not exacerbate and have few eosinophils can relatively safely avoid the inhaled steroid, whereas patients who exacerbate and have many eos should keep it at all costs (Fig. 2). However, according to Prof. Lommatzsch, not everyone should be given a triple because the ETHOS study has again clearly shown that there is a non-dramatic but nevertheless increased risk of pneumonia.
Finally, the pulmonologist pointed out a surprising aspect: under triple therapy, there is a certain reduction in mortality. “We can’t explain it mechanistically so far because it’s not done with exacerbations alone,” he acknowledged. However, now that two large randomized blinded trials, IMPACT and ETHOS, have shown the effect, the question of why inhaled steroids might reduce mortality must be addressed. If this is confirmed in further studies, one would of course have to think about whether and how to incorporate it therapeutically.
Source: Streamed-up-Seminar “PneumoLive: Post ATS/ERS”
Literature:
- Polverino F, Soriano JB: Eur Respir J 2020; 55: 1902457; doi: 10.1183/13993003.02457-2019.
- Kerstjens HAM, et al: Lancet Respiratory Medicine 2020; 10: P1000-P1012; doi: 10.1016/S2213-2600(20)30190-9.
- Chalmers JD, et al: Eur Respir J 2020; 55: 2000351; doi: 10.1183/13993003.00351-2020.
InFo PNEUMOLOGY & ALLERGOLOGY 2020; 2(4): 20-22 (published 12/2/20, ahead of print).