Sinusitis is one of the most common infectious diseases in children and adults, and antibiotics are often prescribed. However, in contrast to chronic rhinosinusitis, antibiosis is rarely necessary in the acute form of this disease.
The current guideline of the German Society of Otolaryngology distinguishes between acute, recurrent acute and chronic disease [1]. Acute rhinosinusitis is present when the typical symptoms of mucosal inflammation in the area of the nose and sinuses persist for a period of up to twelve weeks. In recurrent rhinosinusitis, repeated acute episodes occur at least four times a year, with symptoms completely resolving in the interim. In chronic rhinosinusitis, the symptoms last longer than twelve weeks by definition, although courses lasting for years are not uncommon. A distinction is made between chronic rhinosinusitis with nasal polyps (CRSwNP) and without nasal polyps (CRSsNP).
Acute rhinosinusitis is often viral and self-limiting
Acute inflammation usually occurs in the course of upper respiratory tract infections when swelling of the mucous membranes impedes the drainage of secretions from the sinuses. Typical symptoms of an acute episode of rhinosinusitis include nasal obstruction, anterior and/or posterior secretions, facial pain, olfactory dysfunction. Optional symptoms include fever and/or headache. It is often a viral cause of disease in the setting of a viral upper respiratory tract infection [2]. Bacterial rhinosinusitis is estimated to be present in only 0.5% to 2% of cases [2]. Nevertheless, antibiotics are often prescribed. Unnecessary use of antibiotics promotes the development of antibiotic resistance [3].
An overview of common influenza viruses and some other respiratory viruses is available at the following links: Influenza Working Group homepage: https://
influenza.rki.de, Respvir(https://rvdev.medical-dpc.com/inhalte/start-viren.html). By the 2018/2019 winter season, influenza viruses accounted for up to 40% and rhinoviruses up to 20% in Europe, depending on the season [3].
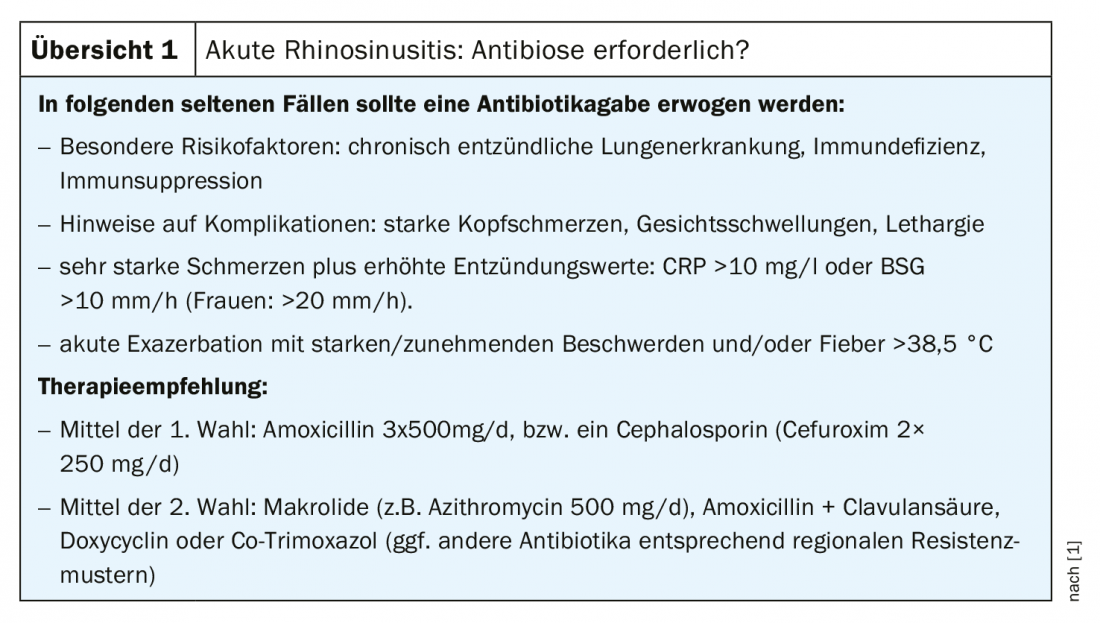
Only in rare cases is parenteral administration of antibiotics necessary for viral acute rhinosinusitis [3]. In acute uncomplicated courses, however, antibiotics are not indicated. In 60% to 80% of acute courses, affected individuals are symptom-free within two weeks without therapy, and after four weeks, this rate is as high as 90% [4]. In order to prevent complications and reduce the suffering pressure, the following symptomatic treatment options are recommended in the current s2k guidelines [1]: Decongestants (free of benzalkonium chloride, duration of application max. 10 days), analgesics, local corticosteroid applications, saline rinses, heat applications/inhalations, Sinupret® eXtract [5], eucalyptus extracts. Antibiotics should be prescribed for acute (recurrent) rhinosinusitis only in patients with specific risk factors and evidence of complications (review 1).
Treatment options for chronic rhinosinusitis
When the symptoms of rhinosinusitis persist for months, they progress to a chronic stage as a result of gradual obstruction due to increased tissue formation [3]. Possible bacterial pathogens of CRSwNP and CRSsNP are: S. aureus, enterobacteria, followed by pneumococci and Haemophilus influenzae. In patients with cystic fibrosis, P. aeruginosa must be considered [3]. Diagnosis is not clinical but requires cross-sectional imaging and/or endoscopy. Referral to a specialist is indicated in cases of unilateral polyps in the nasal cavity, nosebleeds, severe pain, orbital or prefrontal swelling, visual disturbances, acquired asymmetry of the midface or eyes, and when there is numbness in the trigeminal area [3]. Microbiological testing may need to be considered. Regarding comorbidities, chronic rhinosinusitis is often associated with asthma, especially in the presence of ASA intolerance.
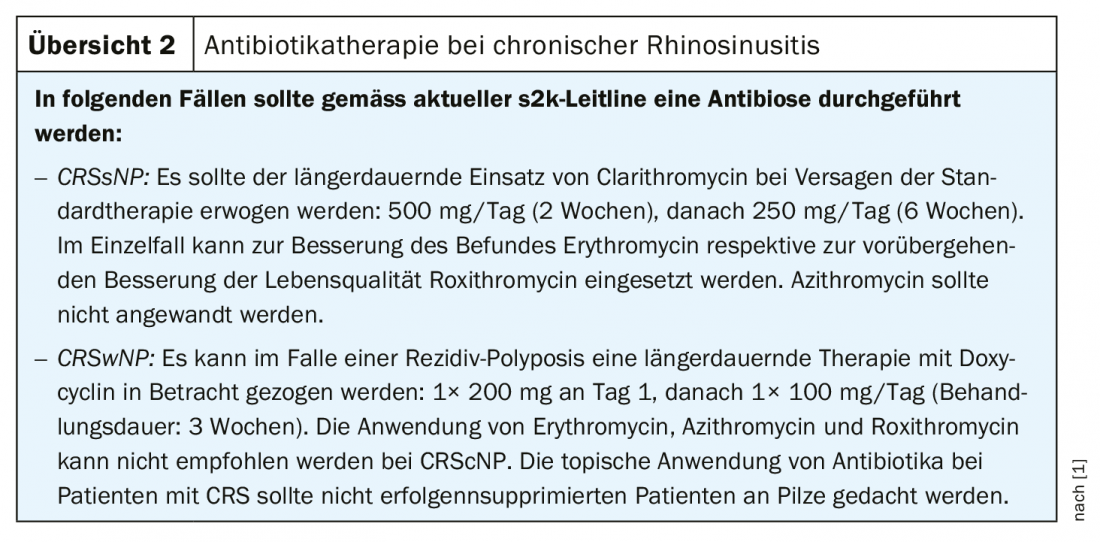
The current s2k guidelines recommend the following drug treatment options [1]: Decongestants should not be used in chronic rhinosinuitis to avoid the risk of developing rhinitis medicamentosa. Topical corticosteroids should be used in CRSsNP as well as, respectively, especially in CRSwNP; therapy with systemic corticosteroids may be considered in individual cases. In individual cases of failure of established therapies, selected biologics can be used in CRSwNP. In patients with confirmed NERD syndrome (NSAID-Exacerbated Resipratory Disease, analgesic intolerance syndrome) and CRSwNP, adaptive deactivation treatment should be given if recurrent polyps occur. The s2k guideline makes the following recommendations on antibiotic treatment for chronic rhinosinusitis [1] (overview 2) : In CRSsNP, prolonged use of clarithromycin should be considered if standard therapy fails. In individual cases, erythromycin and roxythromycin have been shown to improve findings and quality of life. Azithromycin should not be used. In CRSwNP, prolonged therapy with doxycycline may be considered in case of recurrent polyposis. The use of erythromycin, azithromycin, and roxithromycin in CRSwNP is not recommended. Topical antibiotics should not be used in patients with chronic rhinosinusitis.
If conservative therapy does not lead to a (permanent) improvement of the symptoms or if complications such as purulent inflammation of neighboring regions threaten, the current s2k guidelines recommend surgical therapy after exhaustion of medicinal measures [1]: In functional endoscopic surgery of the sinuses, constrictions or diseased mucosa and polyps are removed by means of an endoscope. Balloon dilatation involves using a catheter to insert a balloon and slowly inflate it at the entrance to the sinuses to widen narrowed openings. In some cases, inflammatory mucosal tissue can also be removed by laser treatment.
Biologics for chronic rhinosinusitis with nasal polyps (CRSwNP).
In CRSwNP, recurrence rates are also very high after paranasal sinus surgery. Approximately 25-50% of patients suffer a recurrence postoperatively. This rate is considerably higher still if those with risk factors such as asthma or aspirin intolerance are included. The high relapse rate also applies to patients who have already undergone several operations. With regard to standard drug therapy, side effects are problematic with long-term use of oral steroids. In severe CRSwNP, treatment with biologics has been shown to be effective in contrast to CRSsNP. The European Medicines Agency approved dupilumab for this indication in late 2019 [7]. It is the first monoclonal antibody approved in the EU for this indication. Dupilumab specifically blocks the allergic inflammatory mediators IL4 and Il13, which are frequently involved in CRSwNP. The monoclonal antibody inhibits the growth of polyps and clears the airways. In adults with severe CRSwNP, Dupixent® can be used as an add-on in the EU after unsuccessful treatment with conventional therapy. EMA approval was based on the phase III SINUS-24 and SINUS-52 trials, in which dupilumab 300 mg every two weeks was shown to be significantly superior to standard treatment (intranasal corticosteroids) compared with placebo plus steroids [6].
It is possible that another biologic will receive marketing approval in the foreseeable future. The U.S. Food and Drug Administration (FDA) has accepted the supplemental marketing application for the drug Xolair® (omalizumab) [7]. The application is based on results from the Phase III POLYP 1 and POLYP 2 studies of Xolair® in adults with chronic rhinosinusitis with nasal polyps who have had an inadequate response to intranasal corticosteroids. If approved, Xolair® would be the first antibody to provide symptom relief by reducing the size of nasal polyps. The U.S. agency’s decision is reportedly expected in the third quarter of 2020. Xolair® is already approved in the EU and the USA for various indications for the treatment of allergic inflammation. The mechanism of action of Xolair® is a blockade of immunoglobulin E (IgE), an important inflammatory mediator in allergic processes.
Literature:
- AWMF: S2k-Guideline Rhinosinusitis of the DGHNO and DEGAM, AWMF-Register-No. 017/049 and 053-012 www.awmf.org
- Lemiengre MB, et al: Antibiotics for clinically diagnosed acute rhinosinusitis in adults. Cochrane Database of Systematic Reviews 2012, Issue 10. art. No.: CD006089.
- Abele-Horn M: Infections of the head and neck region. In: Infection diagnosis and oral antibiotic therapy in adults. A guide for the outpatient setting. Bavarian State Office for Health and Food Safety 2019, pp 28.
- Fokkens WJ, et al: EPOS 2012: European position paper on rhinosinusitis and nasal polyps 2012. A summary for otorhinolaryngologists. Rhinology 2012; 50: 1-12.
- Sinupret® eXtract, www.sinupret-extract.de
- EMA: Dupilumab approved for chronic rhinosinusitis with nasal polyps, www.ema.europa.eu/en/documents/product-information/dupixent-epar-product-information_de.pdf
- Novartis: Novartis announces FDA filing acceptance of Xolair® (omalizumab) for treatment of nasal polyps. www.pharma.us.novartis.com/news/media-releases, DEC. 11, 2019.
HAUSARZT PRAXIS 2020; 15(4): 32-33











