The spectrum of treatment for lower urinary tract symptoms ranges from “watchful waiting” to medication and surgery, depending on severity, individual patient wishes, and morbidity. In general, the most important treatment goals include reducing bothersome symptoms as quickly as possible and improving quality of life. But what does this mean in concrete terms? A Systematic Review published in 2021 took a close look at patient demands for treatment.
Lower urinary tract symptoms (LUTS) are common, especially in older men. These are urological complaints composed of symptoms of the storage and emptying phases. One of the main causes of LUTS in men is an enlarged prostate (BPE, benign prostatic enlargement) based on benign prostatic hyperplasia (BPH), which results in subvesical obstruction and thus bladder outlet obstruction (BOO). BOO caused by BPE is called benign prostatic obstruction (BPO).
The initial evaluation includes a medical history and physical examination as well as validated questionnaires such as the IPSS (The International Prostate Symptom Score) and the BPH Impact Index. In addition, imaging, urodynamic measurements, and cystoscopy may be useful in making treatment decisions. When patients do not respond to drug treatment or develop complications, surgical intervention should be considered, with transurethral resection considered the standard procedure for most [1].
Secondary analysis on patient expectations and preferences.
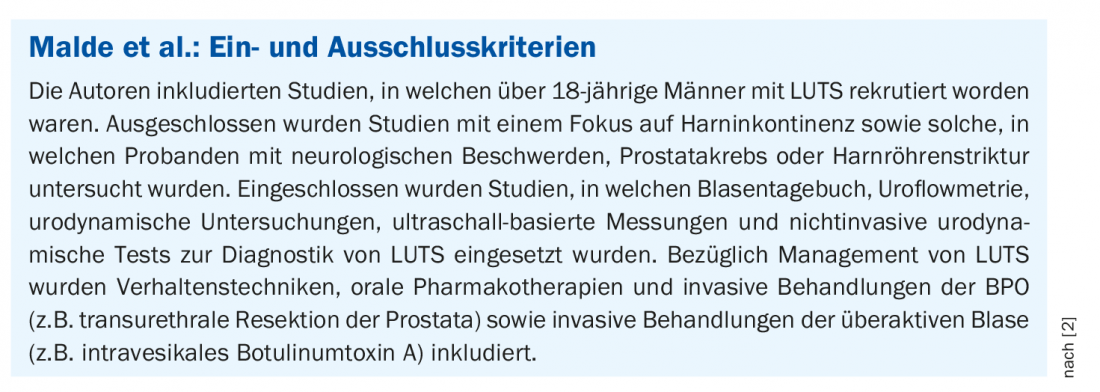
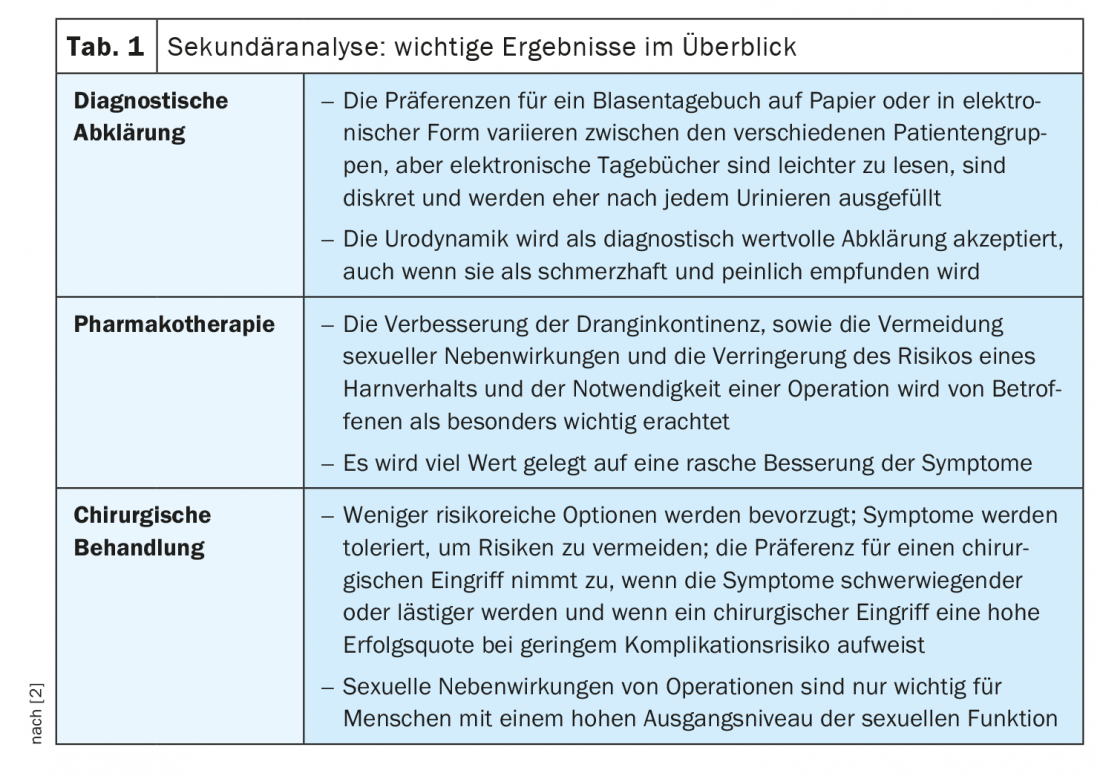
Within the framework of a patient-centered treatment approach, the selection of therapy options is tailored to the respective patient characteristics, taking into account individual preferences. To systematically review the empirical evidence on patients’ wishes and expectations for screening and treatment, Malde et al. performed a secondary analysis, which was published last year in the journal European Urology [2]. Researchers identified records (through Aug. 31, 2020) of quantitative and qualitative studies in electronic databases. The quality of evidence and risk of bias were assessed using the Grading of Recommendation, Assessment, Development, and Evaluation (GRADE) and the Confidence in the Evidence from Reviews of Qualitative Research (GRADE-CERQual). 25 quantitative and 3 qualitative studies as well as 1 mixed-methods study with a total of 9235 subjects were included, which met the inclusion and exclusion criteria. of the Systematic Review (box). Fifteen studies focused on the evaluation of drug treatment options [2] (Table 1). These were the most important evaluation criteria:
- Treatment effectiveness
- Effect on stabilization of the underlying disease process.
- Type of side effects
- Prevention of complications of benign prostatic hyperplasia and
- Burden/cost of treatment.
Improvement of urge incontinence and nocturia as priorities.
Two discrete-choice experiments [3,4] reported that preference for improvement of urge incontinence was nearly four times higher than for nocturia and 18 times higher than that for improvement of increased daytime micturition frequency. These findings are consistent with a report that urge incontinence, nocturia, and increased daytime micturition frequency are the most commonly reported impairments [4]. Patients reported that they found increased daytime micturition frequency annoying, disruptive to daily activities, and embarrassing and limiting, while urge incontinence limited social life and decreased self-confidence. Moreover, subjects reported that nocturia disrupted sleep, led to daytime sleepiness and decreased self-confidence, and also disrupted their partner’s sleep, leading to concerns about the impact on the relationship [4].
Good benefit-risk profile is rated as very important
In survey-based studies, 34-97% of respondents indicated a preference for treatment that produced rapid improvement in symptoms within a few weeks to months [5–8]. Whereas in a US survey, 64% of men preferred disease stabilization to rapid symptom improvement, and 69% were willing to take two medications to achieve symptom relief [6]. Less invasive treatment options with a low risk of adverse events were consistently preferred (7 studies, 1763 participants) [2]. Sexual side effects (erectile dysfunction, loss of libido, and ejaculatory dysfunction) were more important than nonsexual side effects (dizziness and headache) in the preference decision. Up to 93% preferred treatment without sexual side effects. A qualitative analysis also reported that side effects of sexual function were more important than non-sexual side effects (e.g., nausea, dizziness, and dry mouth) [4]. This was not the case in men who were no longer sexually active or who were already experiencing sexual dysfunction independent of LUTS. Nine studies (2354 participants) that looked at reducing long-term disease-related complications reported that 68-85% preferred treatment that reduced the risk of surgery to treatment that reduced the risk of acute urinary retention (AUR), the other major long-term complication.
Drug treatment is preferred by the majority
From two studies with a total of 263 participants, only 12% of patients found taking their medication burdensome [9,10]. When asked to choose between the two alpha-blockers tamsulosin and silodosin, the majority (70%) preferred tamsulosin, with 24% citing less frequent dosing as a reason for their preference.
Regarding the option of surgical intervention, the evaluation of the secondary analysis showed that the majority is willing to tolerate their symptoms to a high degree of impairment [2]. Sexual side effects from surgical procedures were an important consideration for those with high baseline levels of sexual function but not for those with lower levels. The majority of attitudes toward catheterization were negative: 68% reported that catheterization for acute urinary retention affected quality of life more than undergoing surgery [11].
Literature:
- Mcvary KT, et al: Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol 2011; 185: 1793-1803.
- Malde S, et al: A Systematic Review of Patients’ Values, Preferences, and Expectations for the Diagnosis and Treatment of Male Lower Urinary Tract Symptoms. Eur Urol 2021; 79(6): 796-809.
- Mankowski C, et al: Men’s preferences for the treatment of lower urinary tract symptoms associated with benign prostatic hyperplasia: a discrete choice experiment. Patient Prefer Adherence 2016; 10: 2407-2417.
- Ikenwilo D, et al: The best of both worlds: an example mixed methods approach to understand men’s preferences for the treatment of lower urinary tract symptoms. Patient 2018; 11: 55-67.
- Eberth B, et al.: Does one size fit all? Investigating heterogeneity in men’s preferences for benign prostatic hyperplasia treatment using mixed logit analysis. Med Decis Making 2009; 29: 707-715.
- Kaplan S, Naslund M: Public, patient, and professional attitudes toward the diagnosis and treatment of enlarged prostate: a land-mark national US survey. Int J Clin Pract 2006; 60: 1157-1165.
- Weibl P, et al: Patient’s behavior and attitudes toward the management of benign prostatic hyperplasia among patients with the risk of disease progression: prospective study by “Prostate and Expectations of Treatment Epidemiology Re- search (PETER) study group”. Wien Klin Wochenschr 2015; 127: 363-368.
- Weibl P, et al: Patient’s and physician’s behavior on the management of benign prostatic hyperplasia among the patients at the risk of clinical progression. A multicenter noninterventional trial in Slovakia by “Prostate and Expectations of Treatment: Epidemiology Research” (PETER) study group. Wien Klin Wochenschr 2015; 127: 434-439.
- Edelman M, et al: Patients’ attitudes toward deprescribing alpha-blockers and their willingness to par- ticipate in a discontinuation trial. Drugs Aging 2019; 36: 1133-1139.
- Watanabe T, Ozono S, Kageyama S: A randomized crossover study comparing patient preference for tamsulosin and silodosin in patients with lower urinary tract symptoms associated with benign prostatic hyperplasia. J Int Med Res 2011; 39: 129-142.
- Kawakami J, Nickel JC: Acute urinary retention and surgery for benign prostatic hyperplasia: the patient’s perspective. Can J Urol 1999; 6: 819-822.
HAUSARZT PRAXIS 2022; 17(11): 22-23