The formation of brain metastases is a dreaded development, especially in lung cancer. There is also an increasing focus on gender-specific differences in medicine. Multiple myeloma also has variables that can influence the immune response. In addition, biomarkers are being researched in all entities in order to better predict the response to immunotherapy, for example, and to be able to adapt treatment management accordingly. The latest findings in these areas were recently presented.
Several studies have shown that gender is a biological variable that influences the immune response in different types of solid tumors; however, little information is available for hematologic malignancies. One study analyzed the differences in the composition of immune cells and the immune response in multiple myeloma between the sexes in more detail [1]. A computational biology study was conducted using transcriptomic data obtained from bone marrow aspirates of untreated patients with multiple myeloma under the MMRF-COMMPASS protocol. A total of 451 male and 313 female patients were included. An accumulation of activated dendritic cells and activated NK cells was detected in the samples from the female patients. In contrast, an accumulation of monocytes and macrophages M1 was observed in male patients. The GSEA analysis revealed an overregulation of natural killer cell degranulation, a positive regulation of the type I interferon-mediated signaling pathway and a regulation of natural killer cell proliferation.
Predicting disease progression
The aim of one study was to apply machine learning (ML) models to data from patients with multiple myeloma (MM) to assess whether ML models can identify high-risk features associated with faster disease progression [2]. Data from 15931 MM patients in France, Spain, the UK, Germany and Italy were extracted from Oncology Dynamics (OD), a large cross-sectional survey that collects data at the level of treated patients via a panel of cancer specialists. The analyses include data sets from six years (2017-2022). Progression-free survival (PFS) was measured as the time from the start of treatment to the time of progression. Underlying data included treatment regimen, line of therapy (LOT), ECOG status, suitability for stem cell transplantation (SCT), Durie-Salmon stage, cytogenetic risk, age and gender. Survival models based on machine learning were used to predict the results. In addition, Shapley values were calculated to evaluate the model’s decision-making and identify the most important risk drivers.
The data was divided into training data (80%) and test data (20%). The result of the model was the derived ML risk score: a higher risk score was associated with a shorter PFS. The model performance was good. The data show that a higher LOT and the fact that patients are not eligible for SCT are associated with an increased risk of disease progression. LOT, ECOG asymptomatic and certain drug regimens (e.g. lenalidomide or dexamethasone/lenalidomide), on the other hand, are associated with a longer PFS.
Tumor-infiltrating lymphocytes as biomarkers
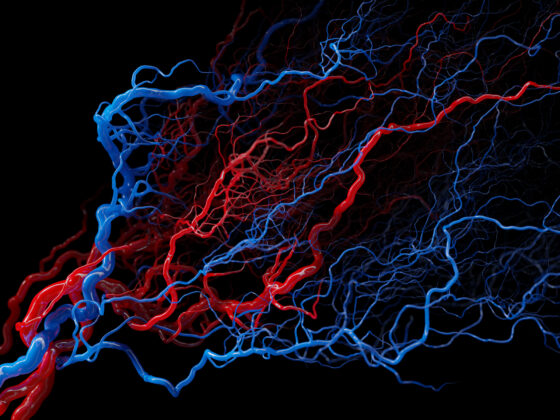
Tumor infiltrating lymphocytes (TILs) are a mixed population of immune cells that infiltrate the tumor microenvironment (TME) and play a critical role in recognizing and fighting cancer cells. The presence, localization and composition of TILs can be used as biomarkers for the prediction of clinical success and response to immunotherapy in different cancer types. The aim of one study was to analyze the correlation between the presence of TILs and gene expression in different types of cancer [3]. The study included 1003 patients with 39 different types of cancer. TILs were successfully evaluated in 922 patients (91.9%). The median (m) of the %TILs was 5%. The cancer types with higher %TILs were duodenal carcinoma, head and neck carcinoma and cervical carcinoma. The %TILs were higher in samples from primary tumors than in metastatic samples. Significant differences were also found depending on the site of metastasis: m=8% in lymph nodes vs. m=7.5% in lungs vs. m=3% in liver. A quantitative SAM analysis identified 31 genes that were significantly upregulated in tumors with a higher percentage of TILs. Among the ten most upregulated genes were nine immunological genes (i.e. CD8, PDCD1 and CD19) and the remaining gene MYC. However, the correlation between TILs and immune genes was moderate.
Congress: ESMO 2023
Literature:
- de los Angeles Clavo M, et al: Microenvironment immune differences between sexes in multiple myeloma. 84P. 22.10.2023. ESMO congress 2023.
- Pleguezuelo Witte ML, et al: Progression-free survival prediction of multiple myeloma patients in five European countries using machine learning models. 844P. 23.10.2023. ESMO congress 2023.
- Segui Solis E, et al: Tumor-infiltrating lymphocites and gene expression across multiple cancer-types: A translational analysis from the SOLTI-1904-ACROPOLI study. 2246P. 21.10.2023. ESMO congress 2023.
InFo ONKOLOGIE & HÄMATOLOGIE 2023; 11(6): 20 (published on 16.12.23, ahead of print)