Case report: A 32-year-old, previously healthy woman developed sudden, mild motor aphasia at 26 weeks’ gestation.
Imaging showed a left frontal intracerebral hemorrhage (Fig. 1a). The cause was an arteriovenous malformation (AVM) in the frontal operculum, with complex supply by branches of the middle cerebral artery. Venous drainage was superficial to the superior sagittal sinus and deep, toward the internal cerebral vein (Fig. 1b).

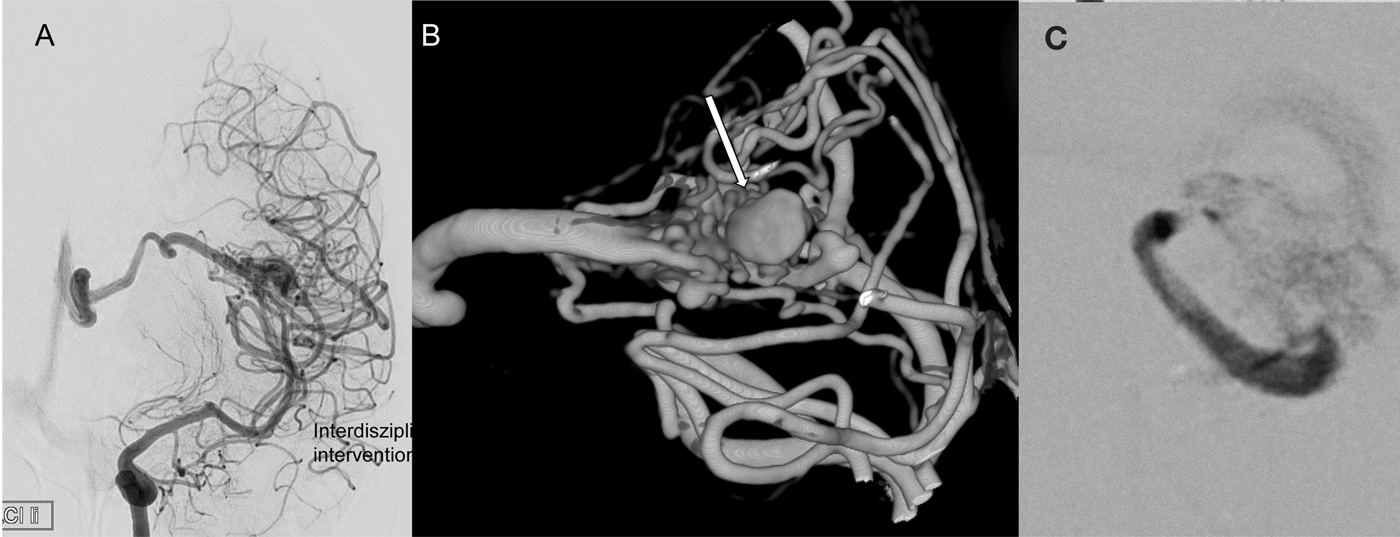
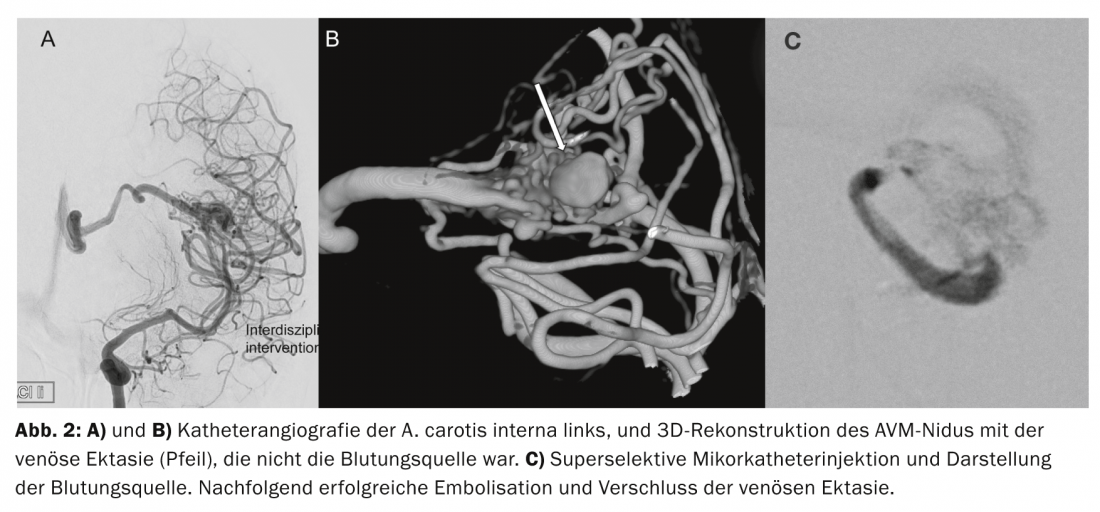
Because of the pregnancy, after interdisciplinary discussion, the decision was made to initially treat the relatively asymptomatic hemorrhage and small AVM conservatively. The symptoms subsequently resolved completely over a period of a few weeks. After problem-free delivery by cesarean section, catheter angiography was obtained for further evaluation and a decision was made to superselectively visualize the supply fraction with associated vascular ectasia presurgically and to address it endovascularly if necessary. This part of the angiomnidus was successfully partially embolized after superselective probing (Fig. 2). Complete elimination was not possible because of the close connection of normal arteries supplying the brain with the fine, perforating arteries supplying the AVM.
Post-interventional MRI was performed to plan further therapeutic steps. Functional images demonstrated a highly elongated location of the residual angioma with a direct relationship to the frontal operculum and motor speech region.
For this reason, to control speech and language function, the surgical procedure was planned while the patient was awake and performed in an interventional-surgical hybrid operating room. Here, the first step in the hybrid operating room was to create an angiography for navigation purposes. The reduced angiomnidus and embolus geometry were accurately recorded.
A frontolateral mini-craniotomy was then created under local anesthesia. After opening the superior frontal sulcus, the angioma was located and detached from supplying vessels under constant neuropsychological control (fig. 3). After transection of the deep draining vein, the entire angioma was removed in toto and the niches of the resection cavity were inspected by endoscope for angioma remnants.

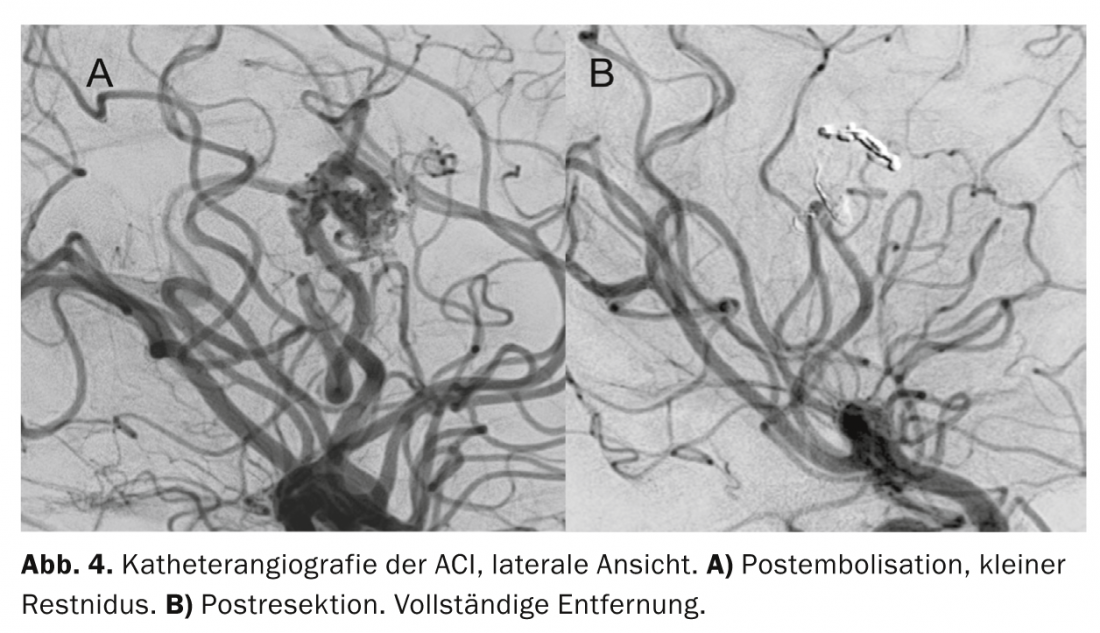
Finally, still with the skull open and awake, the angiography was repeated (Fig. 4) . The examination could not detect any residual nidus or pathological venous drainage. The patient survived the procedure without neurological or neuropsychological deficits. On the following day, complete resection without complications was documented by MRI.
Discussion: Spontaneous intracerebral hemorrhage occurs most commonly in the territories of perforating arteries in the basal ganglia and is usually associated with arterial hypertension. They account for about 15% of all strokes. However, in atypical location and especially in young patients, vascular malformation must be considered and looked for.
If angiographic evidence of hemorrhage due to an AVM is obtained, further action depends on the clinical condition. In cases of large and space-occupying hemorrhages with the threat of entrapment, immediate surgical relief is performed. In a neurologically stable condition, resorption of the hemorrhage can usually be awaited and the AVM treated later. Detailed imaging of the vascular pathology, including the relationship to the surrounding brain tissue, provides the basis for an interdisciplinary treatment plan, which is tailored to a specific patient situation according to the experience of the treating physicians. Due to a large variability of presentation, morphology and localization, clear guidelines can only be defined to a limited extent, which also becomes apparent when consulting the continuously controversial publications.
Therefore, of utmost importance is the discussion in an experienced, interdisciplinary neurovascular team with access to all treatment options, i.e. endovascular interventional, neurosurgical operative and stereotactic radiosurgical therapy options – this under appropriate monitoring, i.e. neurological, neuropsychological, neuroanesthesiological, neurointensivist and neuroradiological. Such a case should thus be discussed in an interdisciplinary neurovascular board with interventional, surgical, and radiotherapy experience.
Primary therapy is usually interventional neuroradiological by superselective probing and embolization of parts of the AVM or even the whole AVM. In the case of partial occlusion, supplementary surgical removal is performed if the localization is superficial or close to the surface. Stereotactic radiosurgical treatment is considered mainly in cases of deep localization and small size of the AVM. The current study situation calls for very cautious treatment planning in AVMs that do not present by hemorrhage. However, in the presence of hemorrhage, a degenerated portion of the AVM can usually be identified, and detailed treatment planning by an experienced team allows treatment with a favorable prognosis if the extent is limited and the location is favorable.
Summary: Intracerebral AVMs are conspicuous by hemorrhage, epileptic seizures, and/or by neurologic deficits. Symptomatic AVMs are usually treated, especially bled AVMs because of a high risk of rebleeding. If embolization does not achieve complete elimination, the AVM is surgically removed. Classically, large-scale cranial openings are used. However, there is a high risk associated with these extensive craniotomies, as healthy cerebral arteries are also exposed to potential injury.
In our case, we were able to successfully partially embolize the eloquently located angioma and subsequently remove it in a hybrid operating room. Skin incision, soft tissue injury, skull opening, and brain surface exposure were minimized. The decisive factor was the interdisciplinary collaboration, which allowed minimal surgical stress and yet maximum safety while the patient was awake.
Acknowledgements: We thank Britta Gaida, MD, for her collegial cooperation in providing anesthesiologic care.
Prof. Dr. med. Robert Reisch
Marton Eördögh
Karen Wachter, MD
Prof. Dr. med. Stephan G. Wetzel
PD Dr. med. Zsolt Kulcsar
Literature:
- HJ Steiger, et al: Neurosurgery of arteriovenous malformations and fistulas. A multimodal approach. Springer Verlag – Vienna 2002.
InFo Neurology & Psychiatry 2014; 12(4): 30-33.