GLP-1 receptor agonists (RA) have been used in the treatment of diabetic patients since 2005. For patients, their introduction was a milestone, as GLP-1 RAs have the great advantage of being weight-reducing* and have little risk of intrinsic hypoglycemia. Likewise, cardioprotective effects make it a valuable weapon against diabetes mellitus. Soon, oral application will also be possible for the first time.
In the meantime, different substance classes are available in antidiabetic therapy for each pathophysiological factor. From this, the antidiabetic drug that is most beneficial for specific additional conditions can be specifically selected. For example, if a patient has already suffered a myocardial infarction or has a high risk profile for one, or if he or she may have end-organ damage, then this will influence the choice of antidiabetic therapeutic agent. In addition, synergistic effects can be exploited with drug combinations, such as when GLP-1 receptor agonists are combined with insulin. Synergistic effects of this combination include.
- HbA1c reduction
- Weight reduction
- lower insulin dose
- lower risk of hypoglycemia
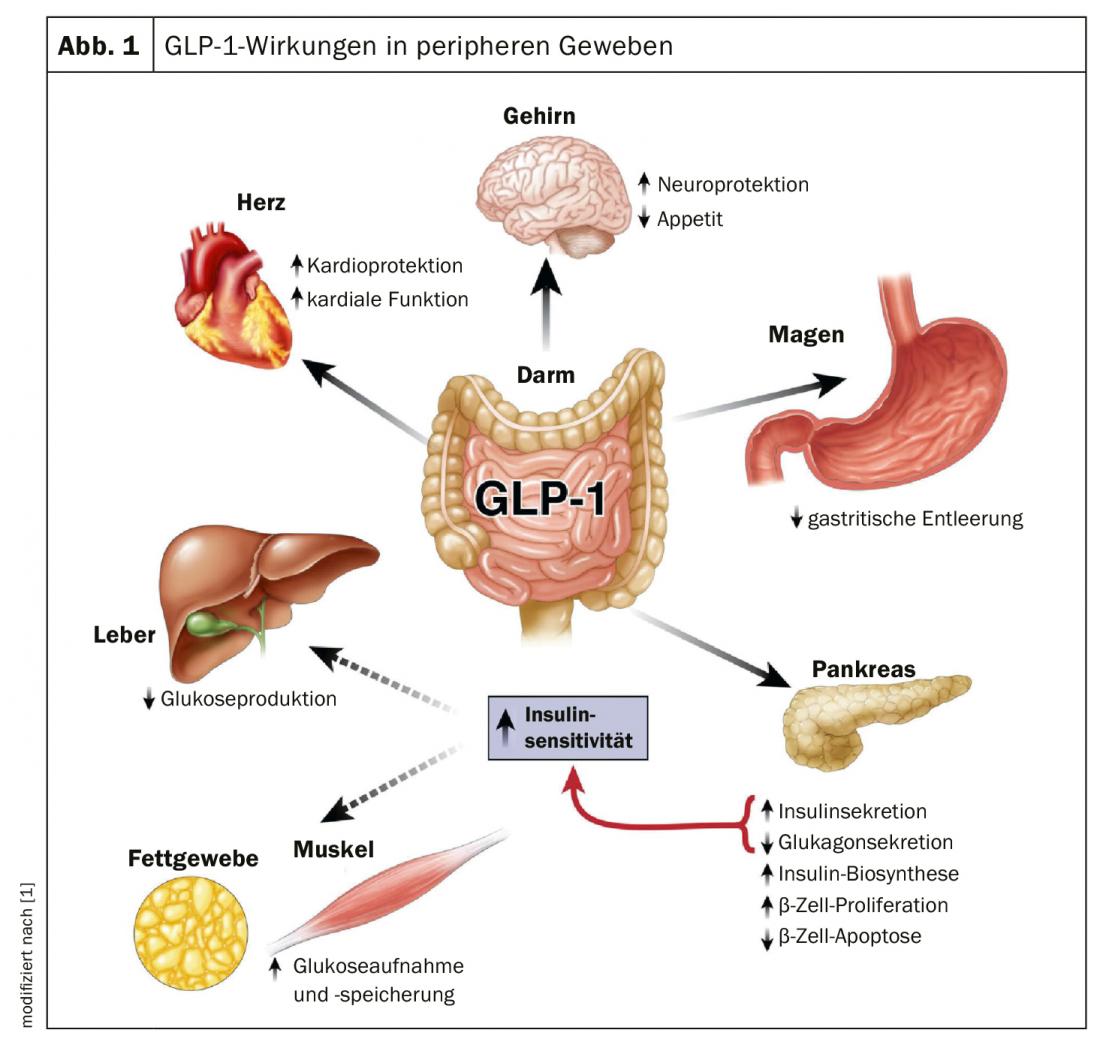
GLP-1 (glucagon-like peptide 1) is a “jack-of-all-trades,” as Dr. Stefan Fischli of the Cantonal Hospital Lucerne explained: it is not only a blood sugar-lowering hormone, it also leads to insulin secretion. This is typically glucose-dependent, meaning that insulin is only secreted when glucose levels are high. When it is deep, this does not happen. “And, of course, that’s one of the big advantages of GLP-1 receptor agonists: you don’t have to worry about hypoglycemia, and you don’t have to specifically train patients, for example, about driving and traffic.” Other benefits include decreasing glucagon secretion and stimulating insulin synthesis (Fig. 1). Also, a GLP-1 RA can be given in advanced renal failure (GFR <30 ml/min).
There are now a large number of GLP-1 preparations on the market. Dr. Fischli’s tip for colleagues: look at the preparations from the perspective of half-life. There are preparations that can be applied daily (exenatide, liraglutide, lixisenatide) and weekly (exenatide LAR, dulaglutide, semaglutide). Depending on the half-life, the mechanism of action also differs somewhat. “You can remember: The shorter the half-life, the more gastric emptying is inhibited and the more postprandial blood glucose levels are affected.” Weekly preparations, by their very nature, have a much longer half-life; all of these preparations result in increased reductions in fasting blood glucose, but do not affect postprandial levels as much. Also, certain preparations can be combined with insulin: Exenatide, liraglutide, lixisenatide and semaglutide are officially approved combinations according to the SL.
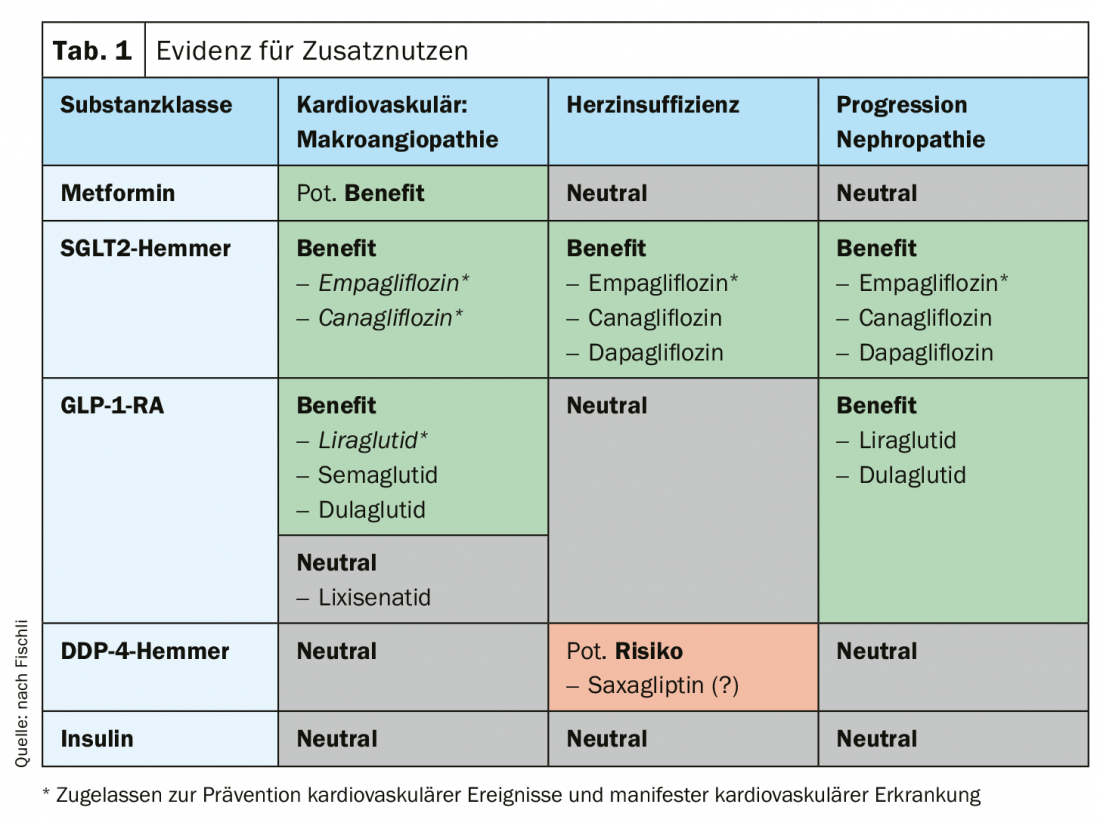
Comparison with other antidiabetic agents
When selecting the antidiabetic drug, the guidelines recommend being guided by the patient’s concomitant diseases and increasingly also by the additional benefit. In the absence of contraindications, metformin remains the basic substance. However, if the patient is at high cardiovascular risk or has established CV disease, a GLP-1 receptor agonist with CV add-on benefit is advisable (liraglutide, semaglutide, dulaglutide) or an appropriate SGLT2 inhibitor (empagliflozin, canagliflozin). If the patient has heart failure or nephropathy, an SGLT2 inhibitor is indicated (empagliflozin, dapagliflozin, canagliflozin). In the absence of such risk factors, the focus of treatment can be on hypoglycemia prevention (DDP-4 inhibitors, SGLT2 inhibitors, GLP-1-RA) or weight reduction* (GLP-1-RA, SGLT2 inhibitors) (Table 1).
* GLP-1 RAs are not indicated for weight loss when used as antidiabetic agents.
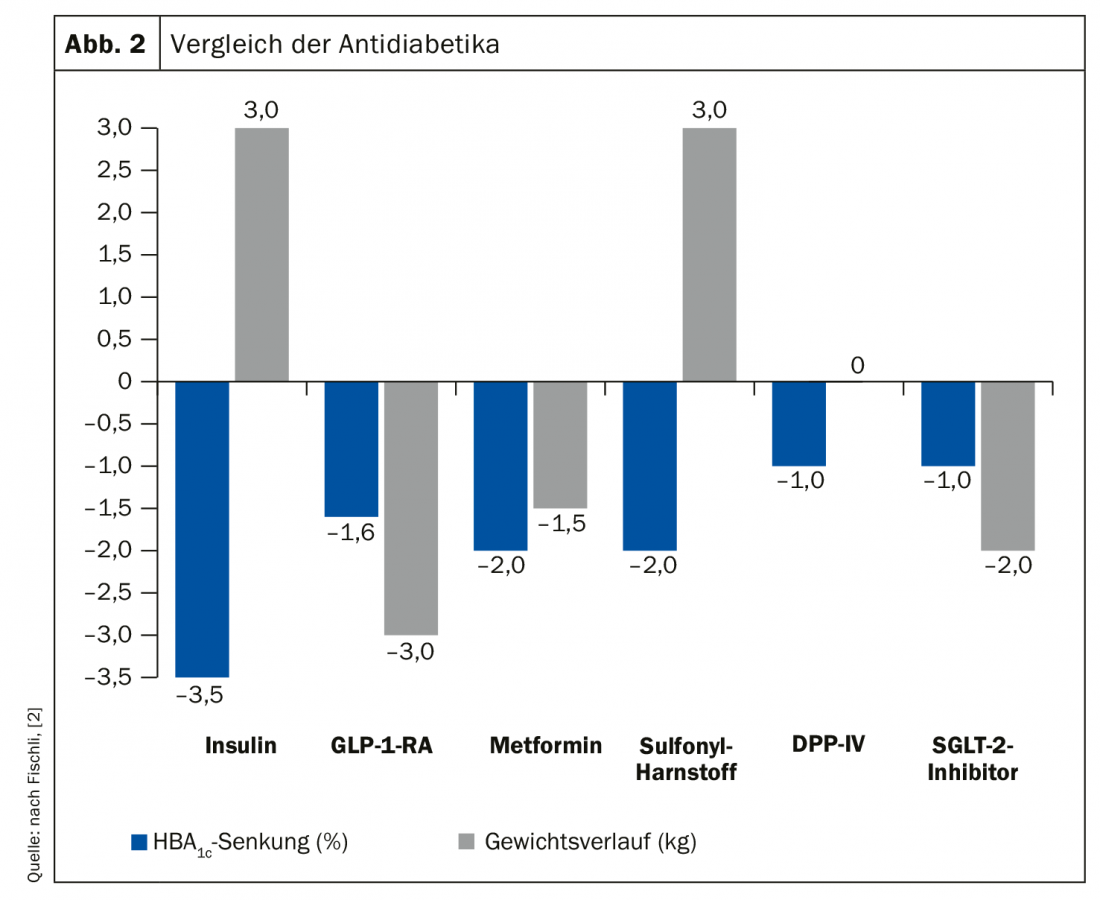
With the various options of antidiabetic therapies, one should always keep in mind what exactly can be achieved with a treatment. For example, a comparison of the various options (Fig. 2) shows that with insulin as the strongest antidiabetic drug, virtually all diabetes can be controlled, but at the price of a sharp increase in weight. A GLP-1-RA, on the other hand, has a weaker but still very decent HbA1c reduction and additionally has a weight-reducing effect on the plus side. Sulfonylurea, similar to metformin, has convincing HbA1c reduction, but again is associated with weight gain and increased risk of hypoglycemia. In principle, Dr. Fischli said, all these substances can be combined with the exception of GLP-1 receptor agonists and DDP-4 inhibitors. On the one hand, this combination is not approved, but on the other hand, it does not make pathophysiological sense. Currently, the combination of GLP-1-RA and SGLT2 inhibitor is not yet approved by the health insurer.
Oral GLP-1 is coming
In news, the first oral GLP-1 receptor agonist has been announced for launch in the fall of 2020. The functional principle: Semaglutide is coated with a so-called absorption enhancer (SNAC). This SNAC causes a pH increase locally in the area of the gastric mucosa so that it is not degraded. This increase also requires improved solubility so that semaglutide can then be absorbed through the gastric mucosa. In this case, only about 1% of the semaglutide is absorbed, requiring a higher initial dose. But you can achieve the same serum levels with it as with application by injection. Patients who cannot imagine injecting on a regular basis are thus given the option of accessing the benefits of this therapy with the orally administered GLP-1 receptor agonist. The preparation is taken daily, with water on an empty stomach 30 minutes apart from the next food intake. Similar to taking thyroid hormones, as Dr. Fischli explained.
Source: Forum for Continuing Medical Education/WebUp “Fresh wind in the new decade: advances in type 2 diabetes therapy thanks to GLP-1 receptor agonists,” July 16, 2020; www.fomf.ch/webup/diabetes-mellitus-typ-2-fokus-16-07-20
Literature:
- Baggio LL, Drucker DJ: Biology of Incretins: GLP-1 and GIP. Gastroenterology 2007; 132: 2131-2157; doi: 10.1053/j.gastro.2007.03.054.
- Adapted from Nathan: Diabetes Care 2009; Kendall: Am J Med 2009; Madsbad: Expert Rev Endocrinol Metab 2009; Richter: Cochrane Database 2009; Inzucchi: Diabetes Care 2015; Aroda: Clin Ther 2012; Meneghini: JCEM 2011; Vasilakou et al: Ann Int Med 2013.
HAUSARZT PRAXIS 2020; 15(8): 21-22 (published 8/16/20, ahead of print).