Osteochondrosis dissecans is a circumscribed disease of the subchondral bone with localized circulatory disturbance, often a consequence of excessive repetitive mechanical stress. Predilection sites are areas of convex joint structures characterized by critical vascularization.
The preceding articles focusing on knee joint symptoms have addressed cartilage changes and meniscal damage as possible causes of symptomatology. Osteochondrosis dissecans (OD) can be included in this series. The clinical picture is characterized by fragmentation of articular cartilage together with subchondral bone. Five stages are distinguished (Table 1), which can be verified very well by magnetic resonance imaging [1]. In this context, the staging that has been valid since the introduction of MRI as a routine procedure in imaging diagnostics has retained its validity to this day.
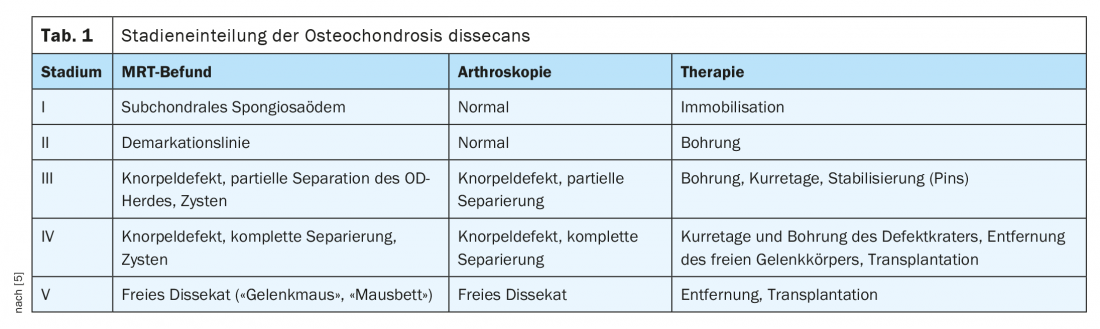
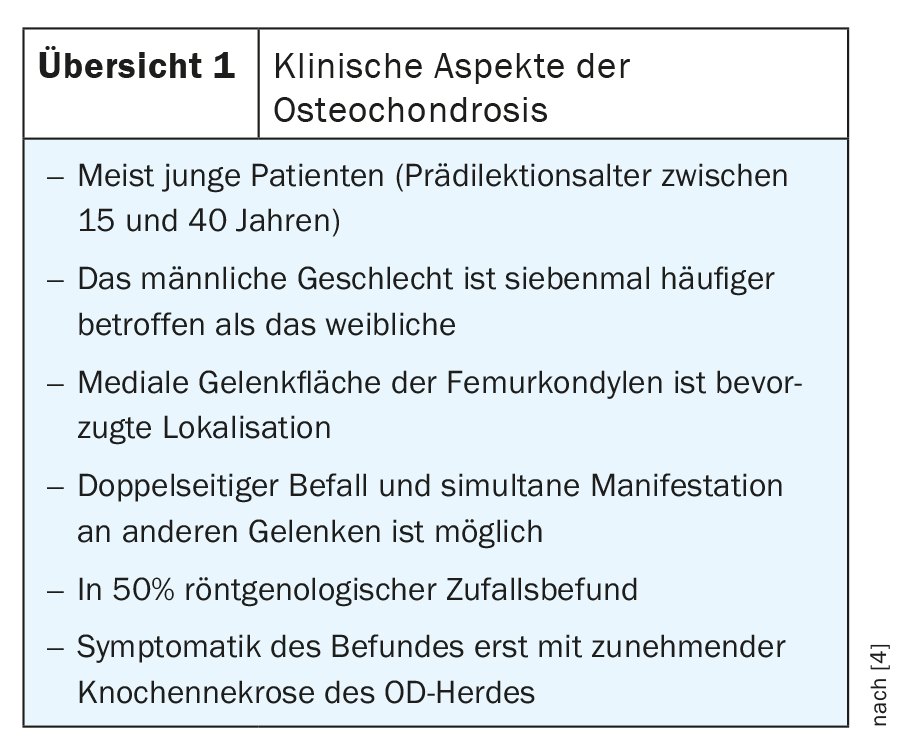
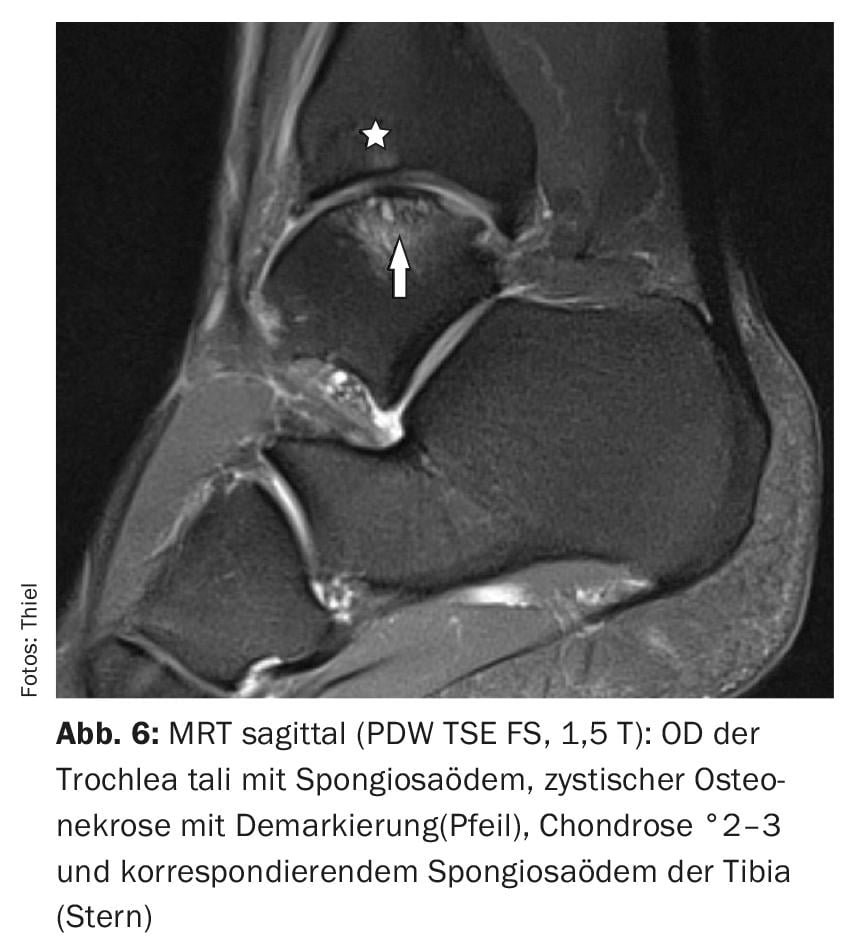
The staging of OD is of great importance, as further treatment planning depends on it. Today, advanced stages, particularly IV and V, are seen relatively infrequently, because in cases of corresponding knee joint symptoms, the MR tomographs that are available nationwide allow rapid, noninvasive visualization of intraarticular joint damage free of ionizing radiation in all age groups for differential diagnosis and adequate therapy. Early detection is very important because in the mostly young patients the defects of the joint surfaces can lead to early osteoarthritis [2,3]. Overview 1 lists important clinical aspects of osteochondrosis dissecans. This may also occur in other joints, such as the ankle (talus), elbow (condyle), or humeral head [4].
In the knee, Ahlbäck’s disease should be considered as a differential diagnosis when dealing with elderly patients. The localization of osteochondral fragmentation also varies: while OD is primarily found in the medial portion of the internal femoral condyle, Ahlbäck mainly affects the more peripheral main loading zone [5].
Radiographs are not useful for early diagnosis of OD. The initial spongiosaedema (stage 1) or the demarking (stage 2) escapes detection. Late changes, such as “mouse bed” or “joint mouse,” can be documented radiographically, including free calcified cartilage fragments (Fig. 1).

Computed tomographic examinations can detect detached OD foci and reliably localize osteochondral fragments already dislocated after intra-articular dislocation.
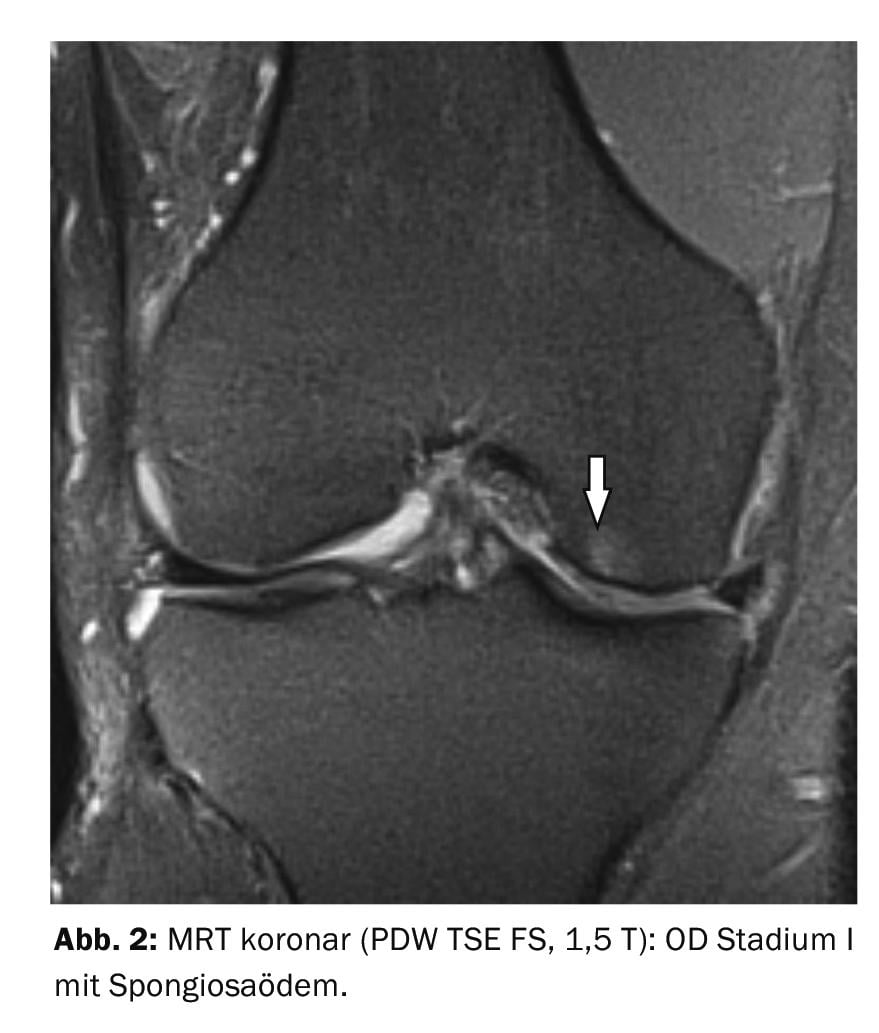
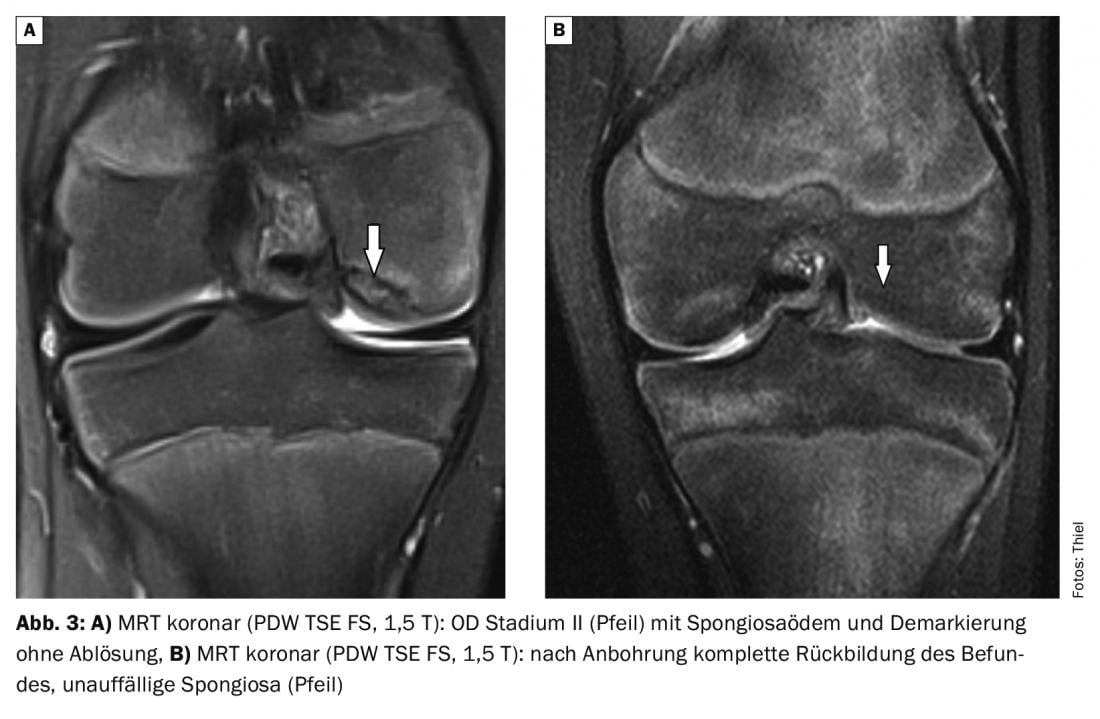
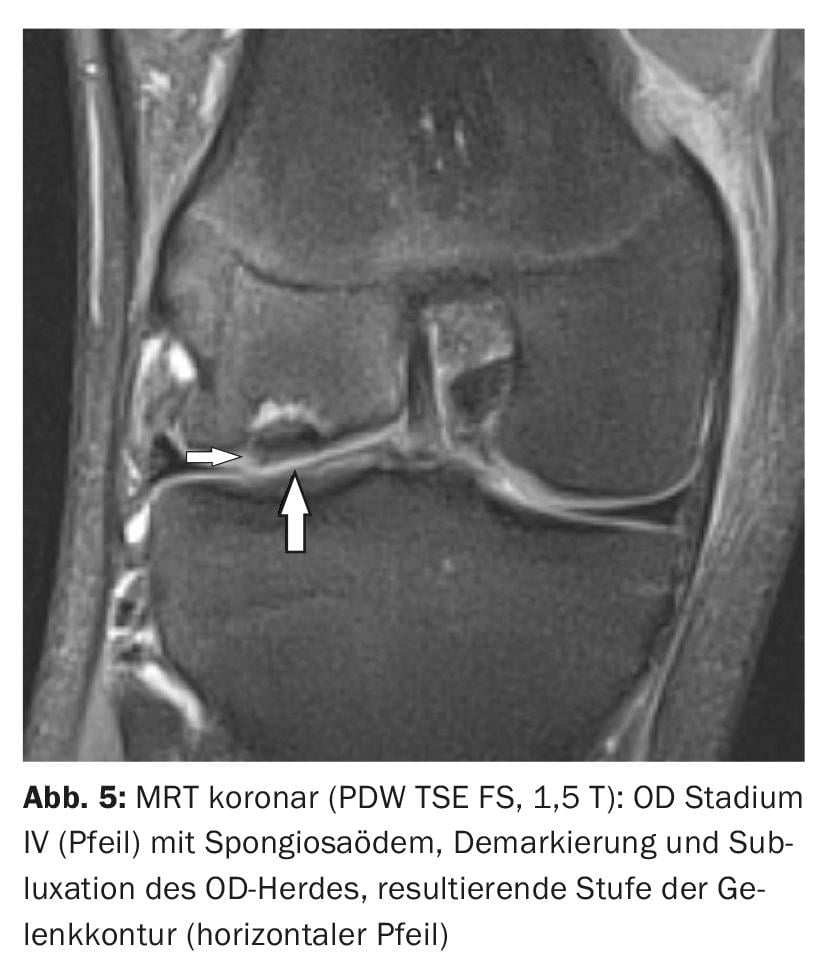
Magnetic resonance imaging is very good at distinguishing the different stages of OD (Fig. 2 to 6) . Progress monitoring during or after completed therapy is also the domain of magnetic resonance imaging. Intravenous contrast agent application allows more accurate assessment of the vitality of bony structures and concomitant inflammatory intra-articular changes.
Case studies
In case report 1 , an 88-year-old patient with knee pain and swelling shows numerous intra-articular calcification formations, compatible with small calcified cartilage fragments (Fig. 1). Findings of chondrocalcinosis medially and laterally, but no radiographic evidence of osteochondrosis dissecans or Ahlbäck’s disease. An OD stage I in the Case 2 (load-dependent pain) shows spongiosaedema without demarkation or alteration of the cartilage or the border lamella of the femoral condyle (Fig. 2). Case study 3: Course of stage II OD in a 19-year-old young man (painful restriction of movement) and the control after tapping (Fig. 3A and 3B) with harmonization of the cancellous bone structure about 9 months after surgery. Case studies 4 and 5 demonstrate OD stage III (17 years, male; complete detachment) and IV (20 years, male; subluxation of osteochondral fragment). An OD of the trochlea tali for comparison in case report 6. There was pain, limitation of motion, and swelling of the joints in each case.

Take-Home Messages
- Osteochondrosis dissecans and Ahlbäck’s disease are aseptic osteonecroses. Imaging diagnostics of choice is magnetic resonance imaging.
- They show no relevant differences in image morphological appearance, but are to be differentiated with regard to localization and main age of manifestation.
- The symptoms depend on the stage and can be pronounced up to recurrent joint blockages, severe pain and effusion-related swelling as well as limited load-bearing capacity of the joint.
- Treatment of OD is conservative in the initial stage and surgical at the latest when a completely isolated or luxated osteochondral fragment is formed.
- MRI is the gold standard for posttherapeutic controls.
Literature:
- Reiser M, Nägele M (eds.): Current joint diagnostics. Stuttgart, New York: Georg Thieme Verlag 1992; 39-42.
- Accadbled F, Vial J, Sales de Gauzy: Osteochondritis dissecans. Orthop Traumatol Surg Res 2018; 104(1S): S97-S105.
- König H: Magnetic resonance imaging of the knee joint. Konstanz: Schnetztor-Verlag GmbH 1992; 35-38.
- Burgener FA, Meyers SP, Tan RK, Zaunbauer W: Differential diagnosis in MRI. Stuttgart, New York; Georg Thieme Verlag, 2002: 360.
- Glaser C: Practicalities of preoperative cartilage imaging. Radiology up2date. 2, 2009: 103-113.
HAUSARZT PRAXIS 2021; 16(3): 35-37











